Shutterstock.com
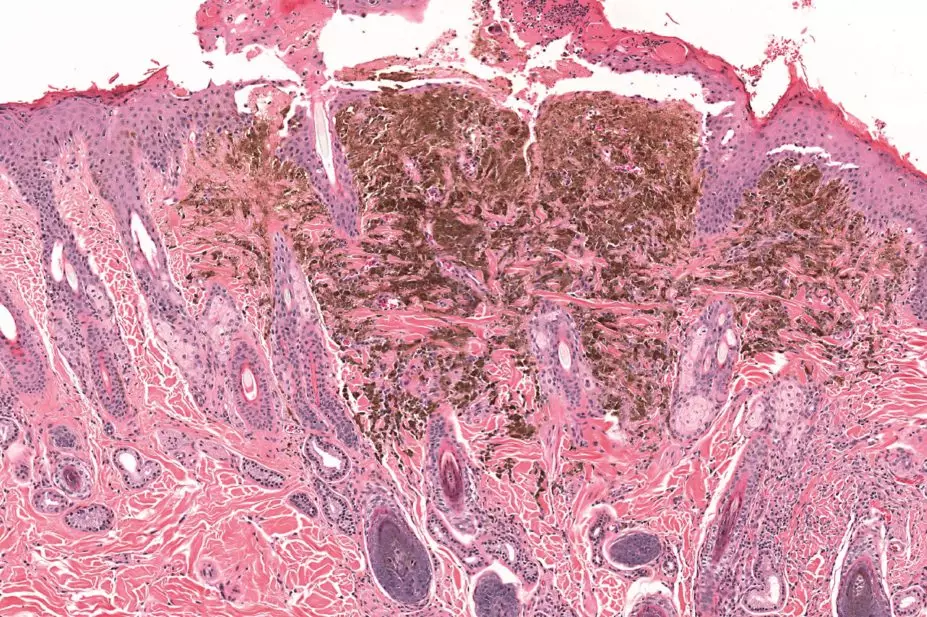
A virus-derived oncolytic immunotherapy has shown activity against melanoma in a phase III clinical trial, researchers reported in the Journal of Clinical Oncology
[1]
on 26 May 2015.
The drug, Talimogene Laherparepvec (T-VEC), is the first oncolytic immunotherapy to demonstrate a clinical benefit in a randomised controlled trial, and thus represents a major advance in the fight against human cancers.
“This study reports another treatment strategy based on harnessing the power of our immune system to destroy melanoma, offering new hope to many patients,” says Muzlifah Haniffa, spokesperson for the British Skin Foundation and honorary consultant dermatologist at Newcastle University.
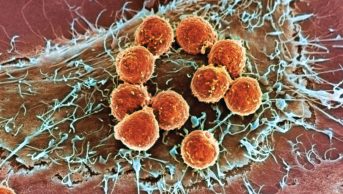
T-VEC, which was developed by Amgen, is a modified form of the herpes simplex virus type-1 that has been genetically engineered to produce granulocyte-macrophage colony-stimulating factor (GM CSF), a molecule that stimulates the body’s immune system to mount tumour-specific T-cell responses.
The virus has been also been modified to selectively replicate in and lyse tumour cells, while being rendered non-pathogenic through functional deletion of the neurovirulence factor ICP34.5 and deletion of the ICP47 gene.
In early-phase clinical studies, T-VEC demonstrated intratumoural replication and expression of GM CSF along with an acceptable safety profile. Subsequently in a phase II study, T-VEC therapy was associated with an overall response rate (defined as a reduction in tumour burden of ≥30%) of 26% in patients with stage IIIC/IV melanoma, with these responses observed in both injected and uninjected lesions.
Now, results of an open-label phase III trial have confirmed the clinical efficacy and tolerability of T-VEC in 436 patients with unresected stage IIIb/IV melanoma. Patients were randomly assigned to receive intralesional T-VEC or subcutaneous recombinant GM-CSF for at least 24 weeks.
The primary endpoint was the durable response rate (defined as the rate of complete response plus partial response lasting ≥6 months continuously and beginning within the first 12 months). The response rate was 16.3% of patients given T-VEC compared with just 2.1% of patients given GM-CSF, at a highly significant odds ratio of 8.9 (p<0.0001).
Secondary endpoints, including overall survival and overall response rate, also favoured T-VEC. The experimental therapy was particularly effective in patients with early-stage disease (stage IIIB/IIIC/IVM1a) and in treatment-naïve individuals, underlining the potential value of T-VEC as a first-line therapy for metastatic melanoma that is not amenable to surgery.
The most common adverse events with T-VEC were fatigue, chills and pyrexia; the only grade 3/4 adverse event occurring in ≥2% of T-VEC-treated patients was cellulitis and there were no treatment-related deaths.
“Our study showed that T-VEC can deliver a significant, durable benefit for people with melanoma. It is encouraging that the treatment had such a clear benefit for patients with less advanced cancers — ongoing studies are evaluating if it can become a first-line treatment for more aggressive melanomas and advanced disease,” says Kevin Harrington, one of the trial investigators and professor of biological cancer therapies at the Institute of Cancer Research, London.
The trial was led in the UK by researchers at the Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, London, and involved 64 research centres in the United States, the UK, Canada and South Africa.
References
[1] Andtbacka RHI, Kaufman HL, Collichio F et al. Talimogene Laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol 2015. doi: 10.1200/JCO.2014.58.3377.