Wikimedia Commons
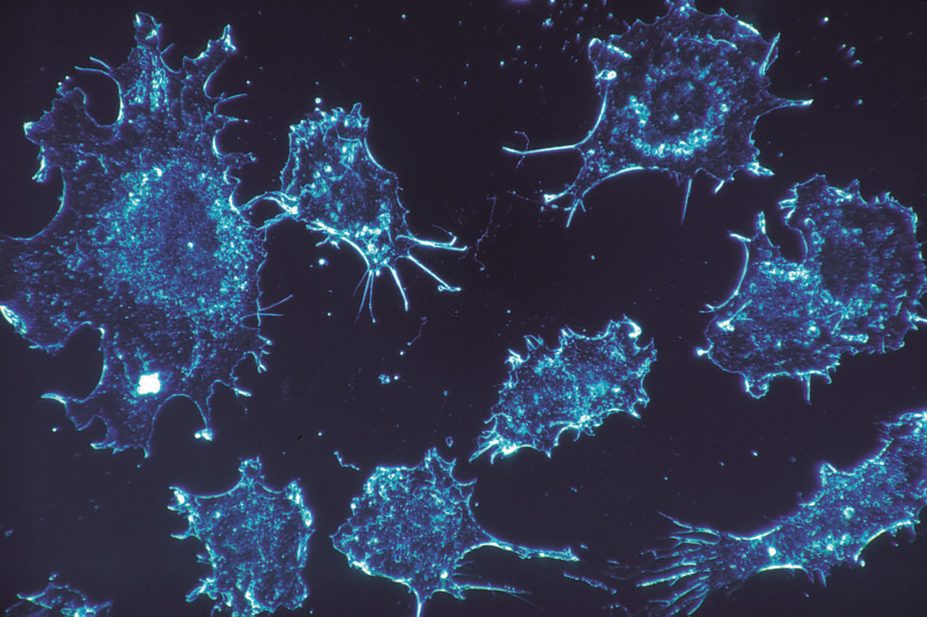
Scientists have developed a therapy that could outsmart cancer cells that have become immune to certain treatments, according to a study published in Cancer Cell
[1]
. By targeting a protein expressed by treatment-resistant lymphoma and leukaemia cells, researchers were able to make the cells vulnerable to treatments that had previously failed.
Researchers discovered that rituximab, a monoclonal antibody treatment, was being destroyed by treatment-resistant B lymphocyte (B cell) cancer cells. In mice grafted with treatment-resistant human tumours, researchers were able to treat the disease by combining rituximab with a newly developed drug that protects it from being destroyed by the cells. This drug, known as 6G11, could also be used to thwart resistance to treatment with other monoclonal antibodies, the researchers suggest.
Mark Cragg, professor of experimental cancer research at the University of Southampton, who led the study, says the results in the humanised mouse model and in human cancer cells are “encouraging” and the team plans to carry out the first human studies in around 60 rituximab-resistant patients in 2015.
The research adds to a growing group of cancer treatments that harness the body’s immune system to fight the disease. In the case of B cell cancers, which are themselves immune cells, interaction with the immune system becomes even more complex. Cragg says that the strategy they have employed shares aspects of immune checkpoint inhibitor treatments for cancer, in that it blocks signals that tell the immune system not to respond.
Monoclonal antibodies are widely used to treat cancer, where they bind to cancer cells and tell the immune system to destroy them. But a subset of patients are either intrinsically resistant or develop resistance to these therapies. To be effective, rituximab sits on the surface of cancerous B cell where it blocks normal cell function and labels the cell for destruction by macrophages. In cancers that are resistant to rituximab, researchers discovered that a protein called FcγRIIB triggers the internalisation and degradation of rituximab, removing it from the cell surface.
FcγRIIB belongs to a family of proteins called Fc receptors which are found on the surface of immune cells, such as B cells and macrophages. These Fc receptors bind to the Fc portion of antibodies, ie, the bottom part of their “Y” shape. Depending on the type of Fc receptor, it will either stimulate or inhibit a response from the immune “effector” cell (in this instance, a macrophage). In the case of FcγRIIB it dampens the immune response. When it is expressed on the surface of cancerous B cells it binds to rituximab, also on the surface of the cell, and triggers its removal. And in a double whammy, when FcγRIIB is expressed by macrophages, it can bind to rituximab on the surface of the cancerous B cell and tell the macrophage not to destroy the cell.
In a bid to block the FcγRIIB receptor, researchers led by a team at the University of Southampton developed a new monoclonal antibody called 6G11. In a mouse model it was discovered that administering 6G11 with rituximab could overcome resistance. It both prevents rituximab internalisation by FcγRIIB on the surface of B cells and prevents FcγRIIB on the surface of macrophages from dampening the immune response, thus maximising the capacity of rituximab to stimulate a response from the immune system.
Researchers believe that 6G11 also has potential to aid treatment of B cell cancers with other monoclonal antibodies, such as alemtuzumab. It could even be of use in non-B cell cancers, by preventing FcγRIIB on macrophages from dampening the immune response to other monoclonal antibodies.
Administering 6G11 on its own also effectively depleted the cancerous B cells, although not as effectively as combination treatment. The researchers hypothesise that the new 6G11 monoclonal antibody is intrinsically cytotoxic to B cells – by attaching to the offending FcγRIIB receptor, it attracts the attention of the immune system in the same way as rituximab and other monoclonal antibodies.
This cytotoxicity has the potential to affect different immune cells that also express FcγRIIB. By a stroke of luck, the researchers found that other FcγRIIB expressing cells in the humanised mouse model were not affected. “Interestingly, other FcgRIIb positive cells were not deleted. Presumably they are protected in some way. Possible because they express less FcgRIIb. It’s a process we don’t understand,” says Cragg.
The research focuses on cancers that affect the B cells of the immune system, including follicular lymphoma, diffuse large B cell lymphoma, chronic lymphocytic leukaemia (CLL) and mantle cell lymphoma (MCL) . Rituximab is used extensively to treat these cancers, but it is much less effective in CLL and MCL and even in cancer types that are usually susceptible, resistance can be present or develop later.
Based on these pre-clinical studies, the researchers believe that human trials are now warranted.


