
Shutterstock.com
Researchers have raised concerns that antiretroviral drugs given to HIV patients may be increasing susceptibility to syphilis.
Their theory, which needs further research, could explain steep rises in new and repeat cases of syphilis (Treponema pallidum) in gay and bisexual men in the past decade, they report in Sexually Transmitted Infections
[1]
(online, 16 January 2017).
“If our hypothesis is correct, persons on [highly active antiretroviral therapy] HAART for treatment of HIV infection and persons taking HAART for pre-exposure prophylaxis (PrEP) are at higher risk of infection with T. pallidum, and perhaps other infectious and noninfectious agents,” says Michael Rekart, clinical professor in medicine and global health at the School of Population and Public Health, University of British Columbia, Canada. “Their healthcare practitioners should inform these patients and screen them for these conditions more frequently.”
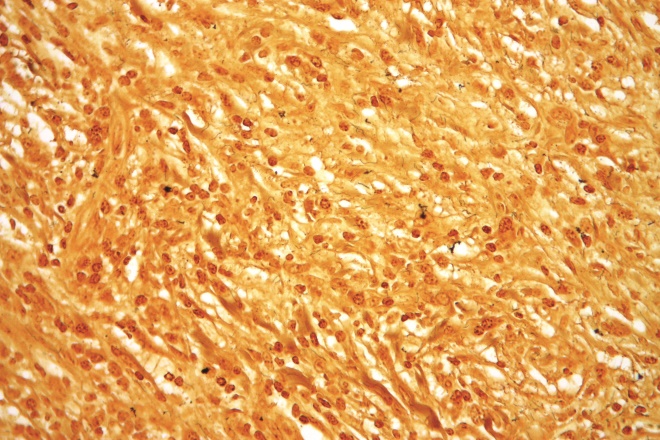
Source: Nephron / Wikimedia Commons
Syphilis is a sexually transmitted disease that can lead to long-term complications if not treated correctly
Use of highly active antiretroviral therapy (HAART) could be linked with higher rates of sexually transmitted infections in general because men who are no longer scared of HIV participate in unprotected sex, but that does not explain why syphilis rates have risen faster than other infections, such as chlamydia or gonorrhea, the researchers say.
Using two risk models, they tested the ideas that HAART would result in more sexual partners and that immune system changes linked to HAART would boost susceptibility to syphilis infection in different scenarios.
Their calculations suggested that either of these factors could lead to an outbreak of syphilis that would be substantially bigger than expected and that together they could produce a peak greater than that caused by either factor alone and matching the sorts of figures seen in the “real world”. This suggests that both behavioural and immune factors are working together to produce the increased rates of syphilis that have been reported, they say.
The researchers also point to research showing that HAART dampens the type of immune system response – harnessing T cells – that the body uses to attack T. pallidum, but that the same response is not as important in the immune response to chlamydia and gonorrhea.
Rekart says several areas of evidence support their theory. These include the “unexpected and dramatic increases” in syphilis in most high-income countries including the UK, several peer-reviewed papers including studies showing that a high proportion of new syphilis cases were taking HAART when they acquired their infection, and the fact that HAART increasing the risk of infection with syphilis is “biologically plausible by several pathways”.
“Our hypothesis needs to be tested under laboratory conditions using experiments in macaques and verified in prospective cohort studies,” says Rekart. “If certain HAART agents are eventually shown to suppress immunity more than others, first and second line HAART recommendations may need to be altered.”
Michael Brady, medical director at sexual health charity the Terrence Higgins Trust, says the study proposes an interesting hypothesis but should be interpreted with caution.

Source: Terrence Higgins Trust
Michael Brady, medical director at sexual health charity the Terrence Higgins Trust, wants the research to be treated with caution
“While syphilis rates in men who have sex with men (MSM), with or without HIV, are rising in the UK, it’s not the case here that rates are higher than those of chlamydia and gonorrhoea.
“Similar increases in gonorrhoea diagnoses in MSM have also been seen in the UK, for example,” he adds.
“It may be that the reason for the increasing infection rates over the past few years has more to do with sexual behaviour than any potential interaction between HIV therapy and the immune system.
“While these findings may warrant further research, they are certainly a reminder of the importance of good sexual health promotion and easily accessible sexual health services to test for and treat STIs.”
References
[1] Rekart ML, Ndifon W, Brunham RC et al. A double-edged sword: does highly active antiretroviral therapy contribute to syphilis incidence by impairing immunity to Treponema pallidum? Sexually Transmitted Infections 2017. doi: 10.1136/sextrans- 2016-052870


