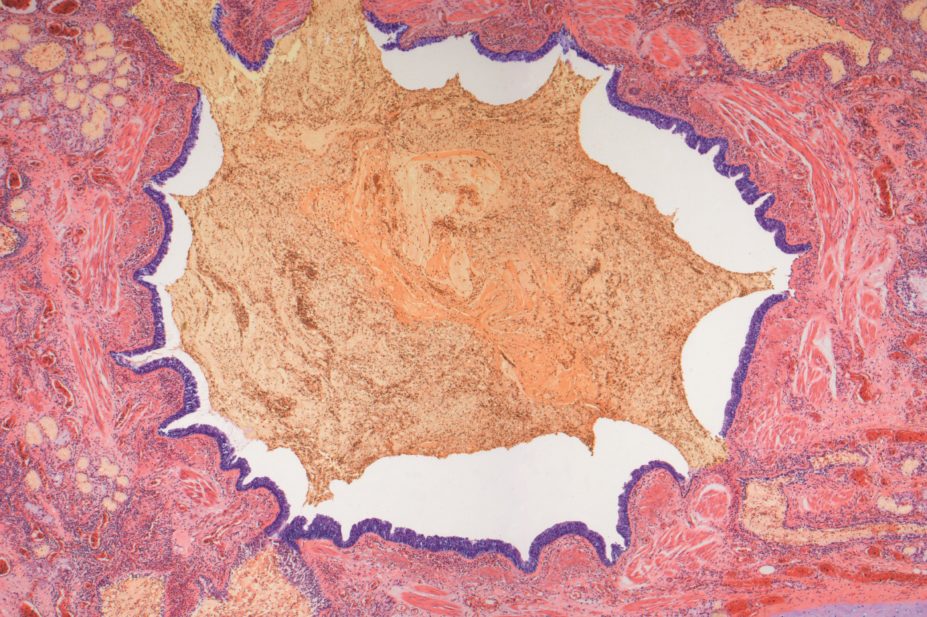
Steve Gschmeissner / Science Photo Library
The US Food and Drug Administration (FDA) has approved Teva Pharmaceutical Industries’ humanised monoclonal antibody reslizumab (Cinqair) as a treatment for severe asthma.
The biologic treatment, which is given as a four-weekly infusion alongside other drugs, is indicated to help those patients with severe asthma who still have serious asthma attacks despite being on regular medication. It is expected to be launched in the United States during the second quarter of 2016. Reslizumab’s approval follows that of GlaxoSmithKline’s new asthma drug mepolizumab (Nucala) in the United States in late 2015.
Severe asthma can be difficult to treat; oral or parenteral corticosteroids are effective, but compliance with these therapies can be poor. In phase III clinical trials[1]
, reslizumab reduced clinical asthma exacerbations compared with placebo in a subgroup of patients with elevated blood eosinophils, and improved lung function.
“Reslizumab provides physicians with another tool for non-responding patients, and by reducing exacerbations it has potential to cut the doses of steroids,” says Albert Rizzo, senior medical adviser to the American Lung Association and section chief in pulmonary/critical care medicine at the Christiana Care Health System in Newark, Delaware.
Reslizumab must be administered intravenously by a healthcare professional in a clinical setting that can manage the potential risk of anaphylaxis. The requirement for a four-weekly clinic visit could affect adherence but, as Rizzo suggests, it is for patients already struggling with asthma control, and so they have an incentive to continue with treatment.
Reslizumab targets interleukin-5, which is linked with severe asthma and increased levels of eosinophils, and is specifically indicated for patients with an eosinophilic subtype.
“We are beginning to understand that there are a lot of different asthma subtypes and that it’s more complicated than just allergic vs. non-allergic asthma,” says Rizzo. “This means that different patients may respond to different drugs. Because bronchoscopies are very invasive, there is a need for more research into simpler and less invasive biomarkers, such as periostin, which has potential in refining asthma subtypes and predicting response to targeted therapy.”
Teva has submitted reslizumab for approval to the European Medicines Agency (EMA) for the treatment of inadequately controlled asthma in adult patients with elevated blood eosinophils, despite an inhaled corticosteroid (ICS)-based regimen. A decision is expected in the second half of 2016.
Despite the launch of efficacious new drugs and continuing research, there are still unmet needs in asthma, Rizzo adds. These include patient education on using inhalers correctly, and the importance of continuing to take maintenance medication even when feeling well.
References
[1] Brusselle G, Germinaro M, Eid S et al. Abstract OA287: Reslizumab in patients with late-onset asthma with elevated blood eosinophils, in European Respiratory Society (ERS) International Congress 2015. 2015: Amsterdam, the Netherlands.