
Alamy Stock Photo
The Pharmaceutical Journal has joined forces with health and hygiene company RB to launch an editorial learning campaign to help pharmacists support patients with foot problems more effectively.
The programme will result in a series of articles published online culminating in a special issue Focus on foot care due in August 2017. The campaign will comprise a series of training articles, expert advice on consultation and business skills, and an infographic highlighting the foot problems most commonly seen by pharmacists.
The collaboration builds on previous work by The Pharmaceutical Journal and RB in 2016 on dry eye conditions.
“Our partnership with RB is a great example of two organisations working together to support working pharmacists and pharmacy teams,” says Tony Scully, publisher of The Pharmaceutical Journal.

Source: MAG / The Pharmaceutical Journal
“The challenge with addressing a broad topic like ‘foot care’ is identifying discrete learning objectives,” explains Scully. “The member survey provided real insight into the learning needs of pharmacists.”
“RB is the ideal partner, giving us the support to create a unique learning campaign providing pharmacists with best clinical practice, aimed solely at supporting pharmacists and their teams to better serve patients,” he adds.
To help inform the campaign, The Pharmaceutical Journal surveyed members of the Royal Pharmaceutical Society (RPS) in April 2017 to gauge how often foot conditions are seen in pharmacy and find out how confident pharmacists are in dealing with them.
“The challenge with addressing a broad topic like ‘foot care’ is identifying discrete learning objectives,” explains Scully. “The member survey provided real insight into the learning needs of pharmacists, helping the editorial team identify the most important topics from which to commission original learning content.”
More than 1,300 RPS members contributed to the survey from across Great Britain. Most respondents were from England, in particular, London (7%), the West Midlands (4%), Greater Manchester (3%) and Lancashire (3%). Scotland was the next best represented country, with 3% of respondents from Glasgow.
The majority were community pharmacists (57%), working in large multiples (31%). But there was also representation from hospital pharmacy (17%), students (8%), pre-registration students (5%) and retired pharmacists (2%). Pharmacy technicians and pharmaceutical scientists made up just under 1% of respondents.
Confidence issues
The survey revealed that while many pharmacists (30%) encounter a foot condition more than once a week, 53% feel uncomfortable diagnosing physical foot conditions and around 35% are uncomfortable diagnosing dermatological foot conditions.
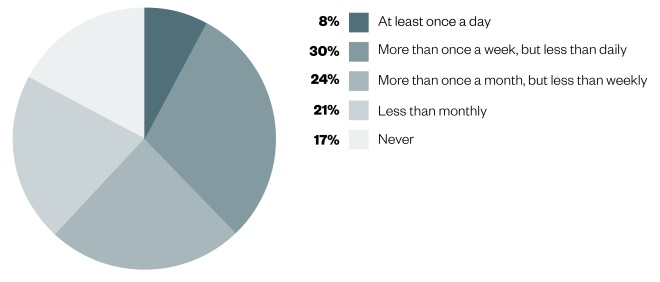
Question: How often do you see foot conditions in practice?
Source: The Pharmaceutical Journal
Thirty percent of those who responded claimed that they see foot conditions in their practice more than once a week but less than daily (n=1,305).
One respondent said that if a patient presents with a foot care problem they cannot treat they would just refer: “I wouldn’t manage their care. I am not comfortable in dealing with foot care topics.”
Richard Leigh, consultant podiatrist at the Royal Free London NHS Foundation Trust, says the figures are not surprising: “Much of the differential diagnosis requires removal of callus to determine what is underneath and I would not advise anyone without the necessary training and qualification to attempt this,” he says.
According to Leigh, diagnosing dermatological foot conditions requires knowledge of the underlying issues, from straightforward fungal infections to connective tissue disorders, and diagnosing physical foot conditions requires an understanding of biomechanics, which is a speciality in its own right.
“It involves understanding the mechanics of the lower limb and its disorders. It also may involve the manufacture of orthotics to maximise the mechanical potential and usually to reduce or prevent pain,” he adds.
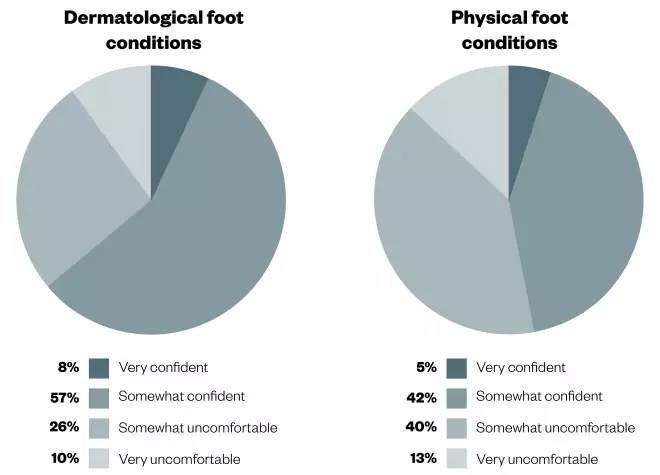
Question: How confident to you feel diagnosing dermatological and physical foot conditions?
Source: The Pharmaceutical Journal
Most of the respondents claimed to be somewhat confident when diagnosing dermatological foot conditions, however forty percent claimed to be somewhat uncomfortable diagnosing physical foot conditions (n=868).
But as Trevor Prior, consultant podiatric surgeon at Homerton University Hospital and director of Premier Podiatry Limited, says, pharmacists are at the forefront of patient care and will often be one of the first healthcare practitioners a patient sees.
“It would seem sensible to get a clear picture of the conditions that will present commonly and then develop an education package around these conditions. This could help with diagnosis, advice for early intervention, and when to refer,” he adds.
Philip Newland-Jones, consultant pharmacist in diabetes and endocrinology at University Hospital Southampton NHS Foundation Trust and spokesperson for the RPS, says: “Pharmacists make a considerable contribution to multi-professional approaches to foot health across the NHS. For conditions such as diabetes, pharmacists working in the community and in GP practices add value to the annual checks undertaken at GP and specialist diabetes clinics by simply asking patients with diabetes questions about their feet as part of the dispensing process and advising on referral as necessary.
“With this proactive approach pharmacists can play their role in helping to improve foot health and preventing ulceration and amputations.”
Athlete’s foot, verrucas, corns and calluses and sweaty/smelly feet are the foot conditions most frequently seen by pharmacists daily, the survey reports. Blood under toenail and flat feet/inward roll of ankle were the least commonly encountered conditions seen by pharmacists daily. After everyday foot conditions, 33% of respondents said that gout was the most common additional foot condition seen in their practice.
Matthew Fitzpatrick, consultant podiatrist and provost, College of Podiatry, and a visiting lecturer at the University of Southampton, suggests a list of seven questions for pharmacy teams to ask patients to help with differential diagnosis:
- How long has the condition lasted?
- What type of pain is it? Shooting, burning, tingling, aching, localised, spreading?
- What makes the pain better or worse?
- When does it come on? Is it a morning pain? Does it come on first thing?
- Is there any familial link?
- Have you seen someone else about this and what did they suggest?
- What are the aims/expectations?
“Maintaining problem-free, comfortable feet is important for our general wellbeing and mobility but foot care as a category spans a hugely diverse number of ailments, patient needs and issues,” says Samantha Bradley, head of professional relations and medical marketing at RB.
“This makes it a confusing therapy area for patients, with pharmacy perfectly placed to offer treatment and advice,” she adds.
Barriers to discussing foot care
The survey also revealed that 84% of respondents only discuss foot care with patients if they are specifically asked about it or if they are diabetic, and 7% said they never mention foot care to patients. 59% of respondents identified barriers, such as time pressures, that prevent them from discussing foot care with patients. A further 22% said it was simply because patients did not want to discuss foot care, with 17% saying that they themselves did not feel confident discussing foot care with patients.
“Not all pharmacists will have access to a dedicated room to allow a confidential examination and may well not have sufficient support to allow the time to make such an assessment,” says Prior, in response to the results. “I could see that this, in conjunction with a perceived lack of expertise would be a fairly obvious barrier.”
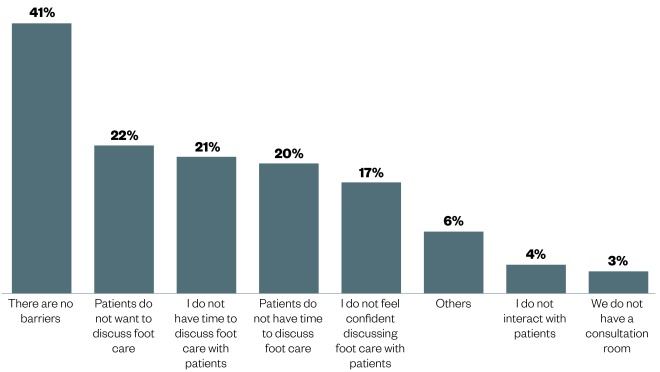
Question: What barriers exist that prevent you discussing foot care with patients?
Source: The Pharmaceutical Journal
Twenty one percent of those surveyed said that they did not have time to discuss foot care with patients (n=698)
Francisco Alvarez, a practice pharmacist at Sandown Health Centre, Isle of Wight, says that pharmacists have a long way to go to master issues that are secondary or tertiary to those being discussed with the patient. “Asking pharmacists to simply introduce [foot care] is not feasible due to work pressures. In general practice, for example, patients are not actively approached with foot care questions unless they are diabetic.”
Alvarez suggests a national campaign to raise awareness of the role of pharmacists to the public. “This would lead to an increase in the number of queries to pharmacists — as was the case with chloramphenicol [eye] drops and amorolfine nail lacquer,” he says.
Further education
Most respondents said that if a patient presents with a foot problem that they cannot treat, such as a diabetic foot ulcer, they would refer the patient to another healthcare professional such as a GP or podiatrist. However, some respondents said that they would first consult the NHS website or search the internet for information before making a recommendation.
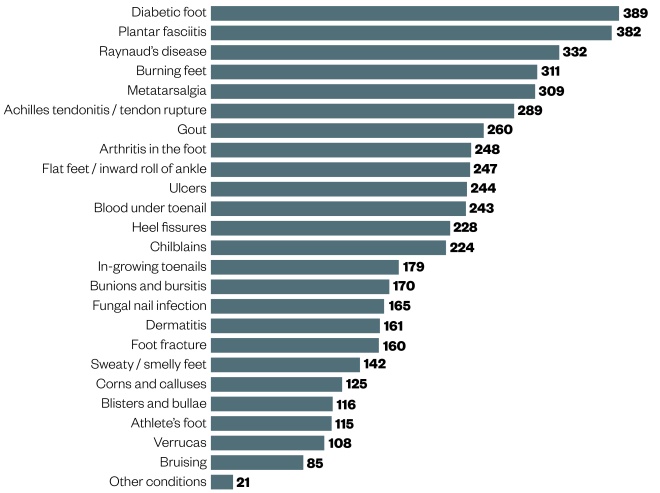
Question: What foot condition(s) would you like to learn more about?
Source: The Pharmaceutical Journal
According to the pharmacists surveyed, diabetic foot, plantar fasciitis and Raynaud’s disease are the top three foot conditions they would like to learn more about. Respondents were permitted a maximum of three answers (n=748)
“I would google what I assume it could be to see images online. Then I would visit the NHS page to see what the recommended treatment is and I would print the page for the patients and also discuss it,” wrote one pharmacist.
When asked what foot conditions they would like to learn more about, 52% said they would like to learn more about diabetic foot in order to deal with it better in their practice. Just over half (51%) said they would like to know more about plantar fasciitis, 42% mentioned burning feet and 41% said they would like to know more about metatarsalgia.
Kingsbury says that pharmacists’ CPD cycle should identify areas where they need more knowledge and training: “Patient-based training to give them familiarity with conditions and also training to allow them to identify incidents where referral is necessary,” she says.
Fitzpatrick, who works as both a consultant podiatrist and a visiting lecturer, suggests training, in partnership with the RPS, could help increase confidence among pharmacists.
“With some infographics, online web tutorials and support with funding from the RPS, we can enable those on the pharmacy front line to be more equipped and confident to spot simple things and then know what is needing to be referred on,” he says.
Collaborative working
Fitzpatrick suggests building networks between pharmacy and podiatry and focusing on conditions that can be helped in a pharmacy setting.
“Sharing knowledge, experience around medicines management with those in podiatry would be a good thing to foster,” he says.
“In my opinion, this could be a big step forward for both professions,” says Prior, who is based at Homerton University Hospital. “Having collaborative working can only be of benefit for the patients and, in turn, can only be positive for the professionals. This may be an area the two professions should consider evaluating more formally.
“With the advent of independent prescribing within podiatry, a working relationship [with pharmacy] would seem even more important,” he adds.
While Leigh, a consultant podiatrist at the Royal Free London, agrees that pharmacists working alongside podiatrists could help increase their scope of knowledge, he says he thinks the pharmacists’ main role in dealing with foot conditions is in the use of over-the-counter (OTC) medication for basic dermatological conditions with pharmacy review and use of OTC insoles.
“Other treatments require specialist intervention and prescription, of both medication and orthotics, and patients should see a podiatrist,” he says.
Over summer 2017, The Pharmaceutical Journal will be publishing a series of articles in partnership with RB to support pharmacists in dealing with a variety of foot conditions.
RB provided financial support in the production of this content. The Pharmaceutical Journal retains full editorial control.
UK/SC/0617/0031
You may also be interested in
The importance of diverse clinical imagery within health education

Entrustable professional activities: a new approach to supervising trainee pharmacists on clinical placements

