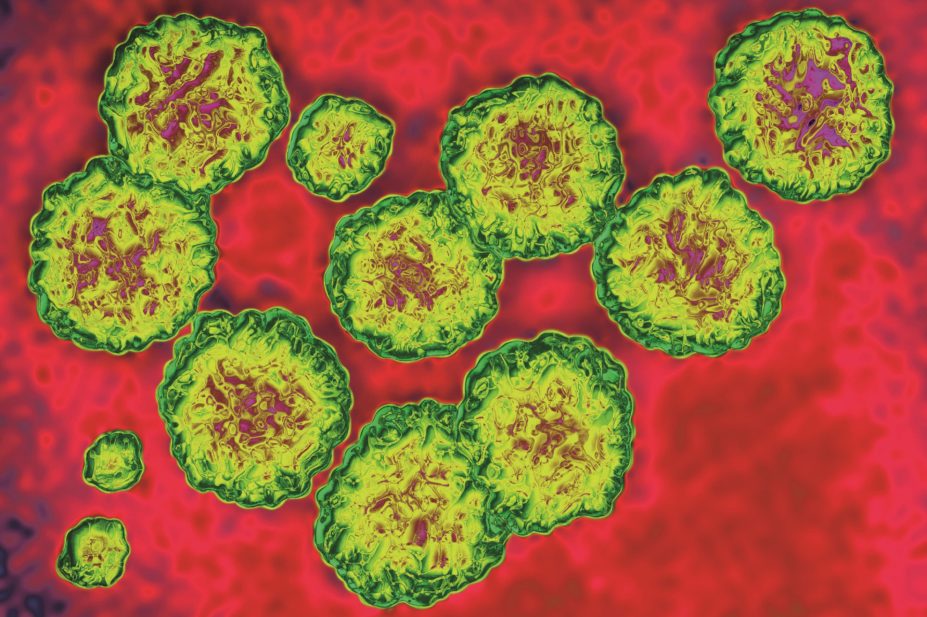
James Cavallini / Science Photo Library
The National Institute for Health and Care Excellence (NICE) has recommended that three additional and expensive treatments should be made available on the NHS to treat routine hepatitis C infection in certain patients.
In final guidance, NICE says ledipasvir-sofosbuvir (Gilead Sciences’ Harvoni), ombitasvir-paritaprevir-ritonavir (Abbvie’s Viekirax), with or without dasabuvir (Abbvie’s Exviera), and daclatasvir (Bristol-Myers Squibb’s Daklinza) should be used to treat adults with some genotypes of chronic hepatitis C.
“Access to the new, highly efficacious, direct acting antiviral agents in easy to manage all-oral regimens has revolutionised the treatment and outcomes for patients with hepatitis C virus cirrhosis,” says Valerie Ross, lead pharmacist at Barts Health NHS Trust, London, adding that the approval of the three therapies “represents a paradigm shift” in the way the condition is treated.
“Widening the national recommendations to include patients at an earlier stage of their disease process will significantly reduce the incidence of liver cancer, arrest the formerly inevitable progression of liver damage, and transform the lives of patients and their families living with hepatitis C.”
A 12-week course of ledipasvir-sofosbuvir is now recommended as a possible treatment for adults with chronic hepatitis C genotypes 1 or 4 that has been treated before but has not responded sufficiently, and for untreated adults with genotype 1 or 4 and cirrhosis. A 12-week course of ledipasvir–sofosbuvir costs £38,980. An eight-week course should be given to adults with genotype 1 without cirrhosis.
Ombitasvir–paritaprevir–ritonavir, with or without dasabuvir, is recommended as a possible treatment for adults with hepatitis C genotypes 1a, 1b, or 4, with and without cirrhosis. The treatment is taken for 12 or 24 weeks, depending on the genotype and whether there is cirrhosis. A 12-week course of ombitasvir–paritaprevir–ritonavir costs £32,200, and an additional £2,800 when combined with dasabuvir. The treatment can also be combined with ribavirin.
Daclatasvir is recommended as a possible treatment for adults with hepatitis C genotypes 1, 3 or 4 who cannot take interferon and, where there is significant fibrosis, for adults with genotype 1 hepatitis C without cirrhosis and those with genotype 4 hepatitis C with or without cirrhosis. It is taken with sofosbuvir or peginteron alfa, and sometimes with ribavirin for 12 or 24 weeks. The average cost of daclatasvir plus sofosbuvir is £59,501 for a 12-week course.
Adele Torkington, lead pharmacist for infectious diseases at North Manchester General Hospital, says the only patients who have had access to these agents so far in England have been those with advanced liver disease. “We hope that by increasing the number of patients who can be treated for hepatitis C we will be able to reduce the transmission rate, which is sadly on the rise in MSM [men who have sex with men] communities due to the increase in ChemSex [having sex under the influence of drugs],” she says.
Torkington adds that hepatitis C is a rewarding therapeutic area for pharmacists to become involved in “due to the wide ranging drug-drug interactions and the need for adherence to these very expensive regimes”.
Charles Gore, chief executive of The Hepatitis C Trust, says the availability and funding of the three hepatitis C therapies will be a major step towards eliminating the disease. “Achieving this requires more than just medication, however, as the majority of infected individuals are either undiagnosed or not under care,” he says. “We must not only tackle the disease itself with a comprehensive public health plan to diagnose, treat and cure patients, but also the stigma associated with it, which in some cases is stopping people from accessing testing and treatment.”
The treatments will become available on the NHS within three months.


