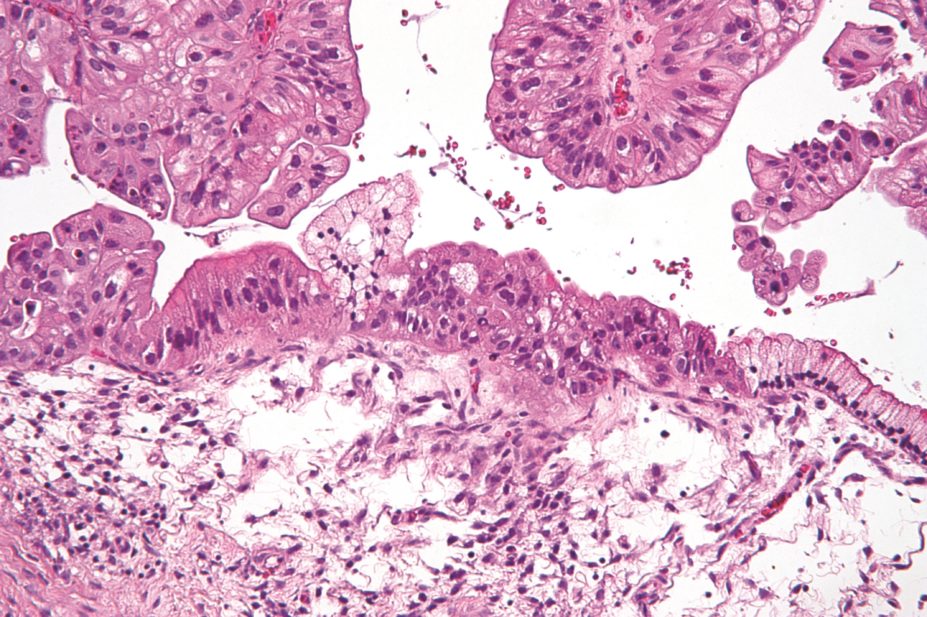
Nephron / Wikimedia Commons
Primary chemotherapy followed by delayed surgery is an acceptable alternative to primary surgery, the current standard of care, in women with advanced ovarian cancer, according to the results of a clinical trial.
Ovarian cancer is the leading cause of death from gynaecological cancer in developed countries, with more than 75% having advanced disease at diagnosis.
The study, which included women with newly diagnosed stage 3/4 ovarian cancer, found that women who underwent primary chemotherapy had fewer side effects and equivalent or better overall survival than women who received surgery prior to chemotherapy.
“Whether to have chemotherapy before major surgery for ovarian cancer has always been a dilemma for women and their surgeons,” says Peter Johnson, chief clinician at Cancer Research UK, which helped to fund the research. “Thanks to this study we can say that having chemotherapy first makes the surgery safer, the stay in hospital shorter and women’s quality of life better.”
In the phase III open-label trial, involving 87 hospitals in the UK and New Zealand, 552 women were randomly assigned to undergo primary surgery followed by six cycles of chemotherapy or to receive three cycles of chemotherapy, then surgery, followed by three more cycles of chemotherapy. A variety of carboplatin-based chemotherapy regimens were used.
Results published in The Lancet
[1]
show that median overall survival was 22.6 months with primary surgery versus 24.1 months with primary chemotherapy, giving a hazard ratio for death of 0.87 in favour of chemotherapy.
Grade 3 or grade 4 adverse events within 28 days after surgery were significantly more frequent with primary surgery than with primary chemotherapy, at 24% versus 14%, as were deaths, at 6% versus <1%. Rates of grade 3 or grade 4 chemotherapy-related toxicity were not significantly different between the groups, although the only fatal toxic effect, neutropenic sepsis, occurred in the primary chemotherapy group.
Geoff Saunders, consultant oncology pharmacist at Christie Hospital, Manchester, says the results show that delaying primary surgery and introducing neoadjuvant chemotherapy does not disadvantage women diagnosed with stage 3/4 ovarian cancer.
“It would appear from this study that this may even improve surgical outcomes for some women with decreased length of stay and fewer post-surgical complications. Overall, this increases options for newly diagnosed patients, potentially introducing effective therapy in those for whom surgery is not an option at presentation,” he says.
Saunders thinks the study may drive a change in practice although long-term outcomes would have to be monitored. “A potential concern could be around interprofessional communication as there needs to be good coordination between surgical, medical oncology and pharmacy teams in providing patient care ensuring smooth transfer between disciplines and timely recommencement of planned treatments,” he notes.
References
[1] Kehoe S, Hook J, Nankivell M et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. The Lancet 2015. doi:10.1016/S0140-6736(14)62223-6.


