Nadia Attura
Emily Rose had her first experience of work as a pharmacist aged just 14 when she spent time in an community pharmacy owned by some family friends. However, it was not until she developed her love of science at school that she saw pharmacy as a potential career path. “I realised that it was an area where I could combine my communication skills and my love of working with people with my scientific knowledge,” she says.
Now, 15 years later, Rose has been awarded the accolade of ‘I Love My Pharmacist’ winner 2015 for her outstanding commitment to pharmacy and, in particular, to the field of rheumatology. Winning the competition, which Rose says she entered after being persuaded by colleagues, is a “real honour”.
“I feel like I represent a high number of pharmacists going above and beyond the call of duty for small reward and recognition so I hope that I’m raising the profile for all others who are working hard,” she adds.
Efficient service
Her achievement honours her work on developing a new rheumatology pathway, which is currently saving the NHS more than £200,000 a year. “The most important outcome was to improve care and safety for each individual patient,” says Rose.
The service, developed in line with guidance from the UK National Institute for Health and Care Excellence (NICE), introduced a monitoring pathway to provide a safe and reliable service for arthritis patients. It also involves prescribing repeat biological therapy after clinical review, which is recorded on an electronic database. The database is used for improving the rheumatology telephone advice line service for patients on long-term therapy, as well as providing analysis reports to feed back to prescribers.
She explains: “We’re seeing patients more regularly and deprescribing when treatment is no longer appropriate, or finding a more effective drug for a patient helping us to make savings.”
Journey to rheumatology
Rose’s career began with a band 6 general rotations post covering the dispensary, manufacturing and wards at the North Bristol NHS Trust before she started her clinical diploma in pharmacy practice at the University of Bath, where she studied pharmacy as an undergraduate.
While doing her diploma, Rose was accepted onto a rotational band 7 post at the same hospital where she gained a taster of many different clinical sectors, as well as valuable exposure to the field of pharmacoeconomics. “I rotated through surgery and neurology,” she reflects. “I also had the opportunity to work in the HIV department and the dedicated satellite pharmacy. It was at that point that I was keen on specialising in something where I would see patients, build a rapport with them and build up their care over a longer timeframe.”
Rose came into the field of rheumatology unexpectedly, when a job for a rheumatology specialist pharmacist became available at Southmead Hospital in Bristol. “On one hand, I did feel fairly unexperienced,” she says, “I had just about finished my diploma and I’d only been doing my band 7 post for a year.”
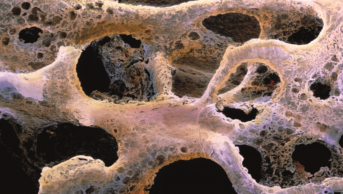
However, she soon realised that the role was exactly what she had been looking for. “Rheumatology is an exciting part of musculoskeletal medicine where there’s a lot of research and a considerable number of new drugs constantly coming to the market,” she says. “Also, it’s an outpatient specialty so you get a lot of face-to-face contact with a diverse group of patients and an opportunity to use the independent prescribing qualification to support a clinical team.”
Making her mark
Despite Rose’s lack of experience, the clinical lead consultant rheumatologist was sold by her positive attitude and comprehensive pharmacy training. However, because she was the first pharmacist to join the rheumatology team, Rose was aware that she needed to make a good impression; adapting her work to fit in with the team but also having the confidence to make changes. “I felt a responsibility to the pharmacy profession to gain the respect of the other medical professions,” she quips.
On arriving in the department in 2013, Rose realised that improvements were needed. “The team were very good at carrying out the appropriate baseline checks when starting patients on treatment for their rheumatological conditions, but monitoring and follow up were less robust,” she says.
By the end of that year, Rose’s new pathway was being implemented. This required 400 homecare arthritis patients to be added, retrospectively, on to the new database. Following a trial run in January 2014, the service was rolled out in March 2014, starting with four patients, then eight, then 16 and so on. By the end of the summer 2015, all the patients were on the system.
Sharing expertise
Rose has now been asked by clinicians from other specialist areas, such as gastroenterology, and other rheumatology teams in the south west of England to work with them to enable them to start developing a similar pathway.
“A colleague said to me that sharing the work is as important as doing the work and I think it’s easy, with the stresses of the daily workload, to feel that we don’t have time to share the work we’re doing,” she concludes. “Why should my patients in rheumatology have a safe and robust pathway when patients in another hospital do not?”