
Taro911 / Dreamstime.com
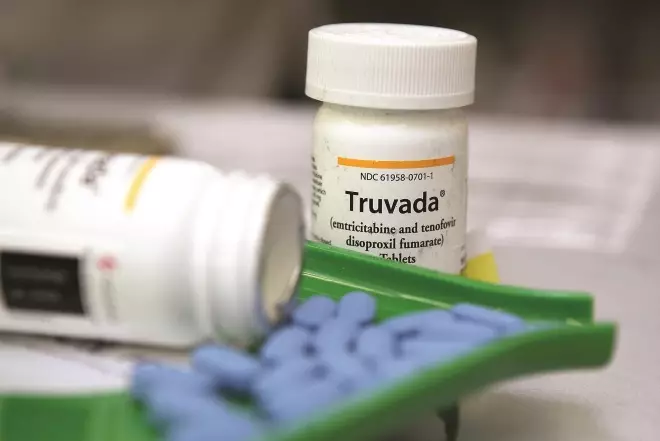
Truvada
Source: Justin Sullivan / Getty Images News
Two or more antiretrovirals are often combined in one tablet to aid adherence
There is currently no known cure or effective preventive vaccine for HIV, and the management of people with HIV infection involves life-long drug therapy. Within the UK, combination antiretroviral therapy (cART) using three medicines is usually recommended by the British HIV Association (BHIVA)[1]
. The aims of treatment are, primarily, to prolong and improve quality of life and reduce transmission of the virus. In some cases, preventing transmission of HIV will be the main aim of treatment (eg, to prevent mother-to-child transmission)[2]
.
According to Public Health England, 85% of diagnosed HIV-positive people in the UK are currently receiving cART[3]
. The intention of treatment is to suppress viral replication below the limits of detection (currently <50 copies/ml), thereby halting the destruction of CD4+ lymphocytes (CD4+ cells). This allows the CD4+ cell count to rebound, enabling recovery of immune system functionality. Early detection of HIV and treatment with cART is essential to achieve successful outcomes for the patient and reduce onward transmission. This article describes the management of HIV using cART — explaining its initiation, how to change therapy, the side effects associated with it, drug-drug interactions and adherence.
Antiretrovirals
Antiretrovirals (ARVs) can be divided into five main classes depending on where they act in the HIV replication cycle (see Box 1). Ritonavir is no longer used as an ARV but for its pharmacoenhancing properties. It is used to “boost” the concentration of protease inhibitors to allow for less frequent dosing and produce a better pharmacokinetic profile. Cobicistat, which has no ARV activity, is also used as a pharmacokinetic enhancer. It is available in a combination product containing elvitegravir (Stribild), and is also approved for use with atazanavir and darunavir (as an alternative to ritonavir).
| Box 1: Mechanisms of action of currently available antiretrovirals | |||
Class | Target stage of HIV replications cycle | Mechanism of action | Examples |
Nucleoside/nucleotide reverse transcriptase inhibitor (NRTI) | Reverse transcription | Compete with natural nucleosides for binding to the active site of reverse transcriptase. NRTIs are incorporated into DNA, resulting in chain termination and incomplete sections of DNA | Abacavir Didanosine Emtricitabine Lamivudine Stavudine Tenofovir Zidovudine |
Non-nucleoside reverse transcriptase inhibitor (NNRTI) | Reverse transcription | Structurally different from NRTIs. Act before incorporation of HIV DNA into host cell DNA by binding directly to reverse transcriptase at regions away from the active site | Efavirenz Nevirapine Rilpivirine Etravirine |
Protease inhibitor | Maturation | Inhibit the protease enzyme to prevent cleavage of viral proteins and maturation of HIV | Darunavir Fosamprenavir Indinavir Lopinavir Saquinavir Tipranavir Ritonavir* |
Fusion/entry inhibitor | Fusion and entry | Bind to extracellular proteins, block the fusion or entry of HIV into a host cell | Enfuvirtide Maraviroc†|
Integrase inhibitor | Integration | Inhibit the enzyme integrase, preventing integration of proviral DNA into host DNA | Raltegravir Elvitegravir Dolutegravir |
* Only used for pharmacoenhancement †CCR5 antagonist | |||
Starting therapy
The decision to start therapy is determined by a person’s CD4+ cell count as well as other factors, such as hepatitis B and C co-infection. BHIVA guidelines for the treatment of HIV-1-positive adults1 provide specific recommendations about when to start therapy in different circumstances.
There are several options for first-line therapy. BHIVA recommends that treatment-naive patients begin cART using two nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs) in combination with one additional medicine from any of the following three ARV classes:
- Non-nucleoside reverse transcriptase inhibitors (NNRTI)
- Ritonavir-boosted protease inhibitors
- Integrase inhibitors
Monotherapy with zidovudine was once the only option for HIV treatment. However, this approach was found only to be better than placebo for six months before resistance occurred and HIV rebounded. In the mid-1990s, highly active ARV therapy combining three active ARVs was demonstrated to provide the greatest chance of suppressing the virus.
Therapy is patient-specific and multifactorial; haematological and biochemical parameters — eg, viral load, CD4+ cell count, renal and hepatic function and genetic markers such as human leukocyte antigen (HLAB* 57:01) status — are taken into account and can directly affect the choice of ARVs used. Hepatitis, tuberculosis, neurocognitive impairment, cardiovascular risk, other HIV-associated comorbidities and the potential for drug interactions with current or future medicines must also be considered, as well as patient preference for particular medicines or formulations.
Some patients may have transmitted (primary) resistance, meaning that the virus has genetic mutations associated with ARV resistance despite the patient never having been exposed to treatment. The prevalence of primary drug resistance in the UK is around 11%[4]
. BHIVA recommends that resistance testing is undertaken for all newly diagnosed patients to guide treatment choice. Full guidelines for when and how to start cART are available on the BHIVA website (see “Useful resources”).
Monitoring
BHIVA recommends that patients are assessed at baseline (ideally three months before starting cART), within two to four weeks of starting treatment, and then three to six monthly thereafter (unless management is problematic)[5]
. The following haematological and biochemical tests should be undertaken to assess treatment response and monitor for toxicity:
- Viral load
- CD4+ cell count
- Full blood count
- Creatinine
- Estimated glomerular filtration rate
- Liver function tests
- Glucose
- Bone profile
Effective cART for treatment-naive patients should achieve viral suppression, demonstrated by an undetectable viral load within 12 to 24 weeks of commencing therapy. If viral decline is slow, then adherence should be checked along with other possible reasons for poor response (such as drug interactions or resistance). Patients can be described as being stable on therapy when they have maintained viral suppression (<50 copies/ml) and a sustained CD4+ cell response.
Toxicity
There is considerable variability in the severity of side effects experienced by patients receiving cART, ranging from unnoticeable to unbearable. Patients may experience side effects early in their therapy or later as a result of long-term toxicity.
Common initial side effects of all antiretrovirals include nausea, vomiting, headache and diarrhoea. Abnormal liver function tests, hepatotoxicity and, rarely, Stevens-Johnson syndrome can also occur in the early stages of therapy. Additionally, efavirenz can cause central nervous system side effects, such as dizziness, vivid dreams and morning drowsiness. Protease inhibitors are known to cause gastrointestinal disturbances, which can be managed using appropriate medicines.
Side effects often coincide with peak drug levels in the blood and can be more intense during the first few days of treatment until a steady state is achieved. Changing the timing of doses or taking them with or without food can often help minimise effects.
Long-term side effects include reduced renal function and bone mineral density, dyslipidaemia, diabetes and changes to glucose control. Peripheral neuropathy, lipodystrophy and changes to body shape are typically only seen in patients who were taking older ARVs and are now rarely seen in practice.
There are ways to manage some of these longer-term toxicities. For example, metabolic syndrome (dyslipidaemia, diabetes and changes to body shape) can be managed pharmacologically using lipid-lowering medicines and antidiabetic treatment, and through lifestyle interventions such as smoking cessation, diet modifications and encouraging exercise.

Blood sample
Source: Taro911 / Dreamstime.com
Regular blood tests are needed to assess treatment response and monitor toxicity
Interactions
Clinically significant drug-drug interactions are highly prevalent among people receiving cART for HIV. People who are infected with HIV are now living longer, hence they are more likely to develop comorbidities requiring treatment. Patients, their clinicians and pharmacists need to be aware of the interactions that occur between ARVs and several commonly prescribed medicines, over-thecounter products and herbal remedies.
Protease inhibitors, NNRTIs and cobicistat have the greatest potential for interactions with other ARVs and with non-antiretroviral medicines. Most interactions occur through induction or inhibition of the cytochrome P450 3A4 (CYP3A4) enzyme. Other enzymes and transport proteins, such as p-glycoproteins, are also involved.
There are numerous drug-drug interactions, which are often highly complex. Single drugs can have multiple pathways for metabolism, and three-way interactions can occur, whereby one drug interacts with two others in the regimen, which, in turn, may interact with each other.
Not all interactions are adverse: ritonavir strongly inhibits CYP3A4 and this is used to boost other protease inhibitors (as described above).
Patients may be receiving medicines from multiple sources and pharmacists play an important role in educating patients, and other healthcare professionals, about the consequences of drug interactions and encouraging them to check with an HIV team before using new medicines, herbal products or illicit drugs. Pharmacists who are screening prescriptions for patients taking cART should be aware of the following general points:
- Atazanavir and rilpivirine require an acid environment for absorption; therefore, proton pump inhibitors should not be used. H2-receptor antagonists and antacids can be used with caution only if the timing of doses is adjusted according to their summaries of product characteristics.
- Medicines that contain iron, magnesium and aluminium (ie, medicines that contain polyvalent cations) — such as multivitamins and indigestion remedies — interact with integrase inhibitors, reducing absorption. They should either be avoided or taken at least four hours before or after a dose of an integrase inhibitor.
- Interactions can occur with medicines administered by other routes that would not usually be anticipated to lead to a reaction. For example, concentrations of nasal, inhaled and intra-articular corticosteroids can be enhanced by protease inhibitor-based regimens, causing corticosteroid toxicity (there have been several reports of Cushing’s syndrome caused by this interaction).
- Different medicines within the same class can have different interaction profiles. For example, protease inhibitors and cobicistat can cause significant increases in simvastatin levels (approximately 600%), as a result of CYP3A4 inhibition, and concomitant use is contraindicated. However, atorvastatin — which is not solely metabolised by CYP3A4 — can be used with a dose adjustment.
- Therapeutic drug monitoring can help ensure adequate levels of cART and is commercially available for NNRTIs, protease inhibitors and integrase inhibitors. However, it is seldom used within the context of drug interactions in practice.
- Dose adjustments of the concomitant medicine, cART components, or both, may be necessary.
- Any decisions to change cART should be made in conjunction with the patient’s HIV specialist doctor.
Adherence
Patients need to take at least 95% of their doses on time. Resistance to cART can develop rapidly when medicines are taken late, missed or stopped suddenly. The latter is especially important for combinations containing medicines with differing half-lives. Levels of ARVs with longer half-lives will remain in the body after those with shorter half-lives have cleared — effectively resulting in a period of monotherapy, which can lead to the development of resistance.
HIV treatment is lifelong and adhering to therapy is essential for sustaining viral suppression. Advances in drug development have led to newer medicines being better tolerated and regimens being more convenient for patients. However, patients can struggle to adhere to their regimen for many reasons. These include:
- Failure to accept HIV-positive status and, subsequently, the need for therapy
- Lack of understanding of the benefits of cART, especially if non-symptomatic
- Perceived adverse impact on lifestyle (food requirements, strict timings of medicines, etc)
- Fear of disclosing HIV status to others
- Fear of side effects and of developing stigmatising side effects (eg, lipodystrophy)
- Perceived harm from taking antiretrovirals
- Intolerance to side effects
- Misunderstanding how to take doses
- Forgetting to take medicine
Most HIV clinics will provide adherence support and counselling for patients to help them adhere to therapy. In the UK, 90% of patients are in contact with specialist care and, in 2011, 70% of patients on treatment achieved an undetectable viral load.3 However, many clinics report this is true for more than 90% of their patients. This has been achieved through delivering patient-centred care that is based on evidence, and having dedicated teams available to provide adherence support. Counselling sessions should be tailored to patients’ needs — addressing relevant factors and concerns linked to individual issues as well as providing general information (see Box 2).
Box 2: Counselling checklist
The following information should be covered when counselling HIV-positive patients on their therapy:
- Show and explain the regimen medicines to the patient
- Inform the patient of the planned start or switch date
- Explain what combination therapy is and why is it used
- Explain how the medicines work, with regards to CD4+ cell count and viral load
- Explain the importance of adherence and consequences of missing doses (ie, development of resistance)
- Inform the patient of how and when to take the medicines. Supply written details if needed
- Discuss the use of reminders, such as mobile phone alerts and medicines compliance aids
- Tell the patient what side effects they could experience and how to manage them
- Explain what the patient should do if he or she misses a dose. (Patients on twice a day dosing regimens can take a missed dose as soon as possible if it is less than eight hours since it was due. Patients on once daily regimens have 12 hours to take a missed dose. Any longer and the dose should be omitted. The next dose should never be doubled)
- Explain what to do if vomiting or diarrhoea occurs. (If more than two hours have passed since the dose was taken then most of it will have been absorbed and there is no need to retake it. However, if less than two hours have passed the dose should be retaken)
- Document and advise on current and any future potential concomitant medicines
- Explain to the patient that he or she must never run out of medicines. Advise on what they should do if they are travelling abroad and if a repeated prescription is needed
- Provide the patient with contact numbers for the pharmacy, clinic and medicines information and to call before any new medicines, over-the-counter products or herbal remedies are started
Switching therapy
There are several reasons why a patient may want or need to switch therapy. These include: intolerable side effects; to simplify a regimen; to avoid potential or actual drug interactions (when patients may have achieved virological suppression); and for patients in whom virological or immunological failure has occurred.
Virological failure is when therapy fails to suppress viral load to below 50 copies/ml or when there is a sustained viral load rebound. These can be associated with poor adherence, baseline resistance to antiretroviral therapy, inadequate plasma drug levels or lack of cART potency (the regimen was not potent enough to bring the viral load down quickly).
BHIVA recommends that all patients who fail virologically for the first time should have a resistance test performed and the results used to guide the choice of new treatment. It is important to determine whether poor adherence is the cause of virological failure before switching the regimen because this would compromise the success of further treatment.
Ideally, CD4+ cell count should return to within the normal range of 500–1,200 cells/μl. Immunological failure is when a patient’s immune system fails to respond to treatment and CD4+ cell counts do not rebound to normal, despite having a sustained undetectable viral load. This is mostly seen in older patients and patients who start treatment when their CD4+ counts are low (<250 cells/μl). Such patients can be difficult to treat, but switching to a new regimen may achieve an increase in CD4+ count (certain medicines can, at times, produce higher CD4+ count increases). CD4+ count is only a surrogate marker of HIV, and it is important to monitor such patients closely for any symptoms of disease progression.
For patients who have achieved viral load suppression, BHIVA recommends that differences in side effect profile, drug interactions and resistance patterns should be considered before switching any component of cART. It also recommends against switching a protease inhibitor to an NNRTI or an integrase inhibitor as a third agent in the circumstance of previous NRTI resistance.1 This is because these medicines have a lower barrier to resistance and three fully active drugs are required in a regimen for it to be effective.
For patients who have virological failure, BHIVA recommends reviewing all previous resistance tests to confirm resistant mutations and to switch as soon as possible to avoid accumulating further resistance. Intensification by simply adding an active antiretroviral to the current regimen is not recommended and may lead to further resistance.
Multiple resistance
Management of treatment-experienced patients is complex and there are often limited available treatment options. Referral to a multidisciplinary team “virtual” clinic is recommended; patients are discussed remotely by HIV medical staff, specialist HIV pharmacists and, if available, a virologist. In triple class resistance, cART should include at least two, preferably three, fully active medicines with at least one active protease inhibitor and one medicine that has a novel mechanism of action (CCR5 antagonist, integrase or fusion/entry inhibitor).1 When a fully viral-suppressive regimen cannot be constructed, because of limited or no therapeutic options, patients may be eligible to receive innovative new medicines through research trials, expanded access or named patient programmes.1
Inpatient care
For patients on cART who have been admitted to hospital and are required to be nil by mouth (NBM), it is important to establish the indication (eg, surgery), intended duration and timing of the NBM period, and if there are other routes of administration available.
ARVs can be taken by patients who are NBM using small sips of water and should continue in the perioperative period with as little interruption as possible, particularly for patients co-infected with hepatitis B virus who are receiving a regimen that has dual activity. However, it should be noted that several ARVs have specific administration requirements and can fail if taken on an empty stomach or with only a nutritional drink, eg, rilpivirine.
Some medicines used during surgery have the potential to interact with cART. For example, protease inhibitors interact with anxiolytics and midazolam is contraindicated with ritonavir. General anaesthetics (eg, halothane), however, do not cause significant interactions. When cART interruption is required, an HIV specialist should be consulted so the components of the regimen can be stopped in accordance with their individual half-lives.
Any causes of swallowing difficulties should be established promptly and, if there is no time frame for resolution, plans need to be made for using alternative routes of administration for the medicines and feeds, such as insertion of nasogastric or nasojejunal tubes. Alternative forms and routes of administration should be discussed with the HIV specialist team because it might be necessary to switch cART.
Further information about alternative dosage forms, such as liquid formulations, tablets that can be crushed or dispersed, chewable tablets, granules and injections, and food considerations for patients taking ARVs, can be found in summary tables on the University of Liverpool HIV resource website.


