
BSIP SA / Alamy Stock Photo
Summary
Migraines occur in 15% of the adult population in the UK. The majority of patients are diagnosed with acute migraines, also known as episodic migraines, which are associated with <15 headache days per month and last 4–72 hours. These migraines can occur with variable frequency; on average these attacks occur once or twice a month. Around 3% of patients develop chronic migraines, which are associated with >15 headache days per month for three or more consecutive months.
Typical symptoms of migraine attacks include nausea, vomiting, photophobia, phonophobia and can include osmophobia. There are no specific diagnostic tests for migraines and diagnosis is based on patient history.
Acute treatment aims to control symptoms and improve quality of life. On first diagnosis, patients should begin with simple analgesia. However, if this fails to control symptoms, then management should progress to 5HT1 receptor agonists. Anti-emetics can be used in patients with nausea and vomiting associated with migraine.
Prophylaxis is the preferred management option for patients with chronic migraines and the choice of drug should be based on the patient’s comorbidities and the medicine’s side-effect profile.
Migraines occur in 15% of the adult population in the UK[1]
. They are painful and disabling, and typically present as a headache associated with gastrointestinal symptoms and a preference for a dark and quiet environment[1]
. Symptoms can be severe, preventing patients from carrying out normal daily activities, and can significantly affect quality of life. It is estimated that there are approximately 190,000 migraine attacks each day in the UK, with around 100,000 people absent from school or work because of them[1],[2]
,[3]
. As a result, the UK economy incurs an annual cost in excess of £1.5bn[1]
. Patients are commonly affected from their late teens into their 50s[1]
and migraines are more commonly seen in women than in men. The pathophysiology is not fully understood, but ongoing research is helping to direct new management strategies[4]
.
According to the World Health Organization, among adults of all ages, migraine is one of the top 20 causes of disability expressed as years of healthy life lost to disability[5]
. Migraines also have a significant effect on a patient’s mental health; for example, depression is three times more common in migraine sufferers compared with healthy individuals[6]
. The availability of over-the-counter (OTC) treatments for migraine increases the risk of patients overusing medicines and may be a cause of under-diagnosis[1]
.
Migraine symptoms, their intensity and their impact on quality of life varies between patients and often between attacks. Therefore, management of migraines should be individualised for each patient. Although no cure has been found, there are many options available to help manage symptoms, reduce frequency of attacks and improve the patient’s quality of life.
This article aims to provide a summary of migraine for pharmacists including evidence and practice-based treatments for their management in adults.
Pathophysiology
Migraine is a disorder characterised by dysfunction of sensory processing[7]
. Patients with siblings who have migraines are three times more likely to experience a migraine attack compared with the general population. It is thought that there is a genetic component and that familial migraines are related to gene mutations[4]
. Mutations linked with familial hemiplegic migraine (FHM) have been identified in the α1A subunit of the P/Q-type voltage-gated calcium channel on chromosome 19. Mutations in the ATP1A2 gene, encoding the alpha2 subunit of the Na+/K+ pump, have been linked with familial hemiplegic migraine type 2 (FHM2)[8]
.
The pathophysiology of migraine is unknown. One possible mechanism is cortical spreading depression, a process in which a slow wave of neuronal and glial depolarisation spreads across the cerebral cortex. This is thought to lead to the activation of trigeminal afferents causing inflammation in the pain-sensitive meni
nges, which then results in a migraine[4],[7]
,
[9]
.
The activation of the trigeminovascular system is also thought to have a role in the pathophysiology of migraines[9
],[10]
. Sensory neurons from the trigeminal ganglion in the face and upper cervical dorsal root in the spine innervate the dura matter and vascular system in the cranium[4]
. Stimulation of the trigeminal ganglion results in the release of vasoactive neuropeptides, including calcitonin gene-related peptide (CGRP), substance P and neurokinin A. These neuropeptides lead to neurogenic inflammation, causing vasodilation (CGRP is a potent vasodilator) and plasma protein extravasation, prolonging and intensifying the pain in migraine.
Neurogenic inflammation may also lead to sensitisation[4]
, in which neurons become highly responsive to stimuli. This is likely to be responsible for many of the clinical symptoms of migraine, including the throbbing nature of the pain and increased sensitivity to pain[4]
.
The role of serotonin is unclear, although medicines that affect serotonin (e.g. tricyclic antidepressants) have been successful in the acute treatment of migraines. Serotonin may have a direct action on the cranial vasculature, affecting central pain control pathways, or its role may be related to the corticol projections of the serotonergic nuclei in the brainstem[4]
.
Previously, it was suggested that migraine headaches were caused by vasodilation and visual auras were caused by vasoconstriction. However, this theory has since been disproved[4]
,
[11]
.
Symptoms
The majority of patients who experience migraines are diagnosed with acute migraines, also known as episodic migraines. Episodic migraine attacks are associated with <15 headache days per month and last 4–72 hours. These migraines can occur with variable frequency; on average, the migraine attacks occur once or twice a month. Around 3% of patients develop chronic migraines, which are associated with >15 headache days per month for three or more successive months[3],[12]
.
Migraines are usually a unilateral pulsating headache, but can present as bilateral pain. They build up over a few minutes to hours and are moderate to severe in intensity[3]
. Typical symptoms of migraine attacks include nausea, vomiting, photophobia, phonophobia and can include osmophobia[7]
.
A migraine attack starts at the prodrome stage[8]
,
[13]
, with symptoms of euphoria, depression, irritability, food cravings, constipation, neck stiffness and increased yawning. An aura may gradually develop. The headache then occurs. During the postdrome phase, patients will feel exhausted or drained and some may feel mild elation or euphoria[4]
.
Auras are focal neurological symptoms that usually affect the patient’s vision, but can also involve other senses causing motor or speech problems[4]
. Auras affect around one-third of migraine sufferers, and typically last 5–60 minutes, which may or may not precede a headache[1],[3]
. Symptoms may be classified as either positive or negative. Patients may experience positive aura as flickering lights, spots, zigzag lines, or tingling and negative aura as visual loss or numbness. Different aura symptoms may occur one after the other[3]
.
The risk of migraine attacks in susceptible individuals can be increased by factors such as stress, depression and oestrogen. Although often unavoidable, such factors can be managed to help control frequency of attacks. It is important to distinguish these predisposing factors from trigger factors, which are associated with environmental, dietary and lifestyle factors and can be managed through avoidance and lifestyle changes[1],[3]
.
Diagnosis
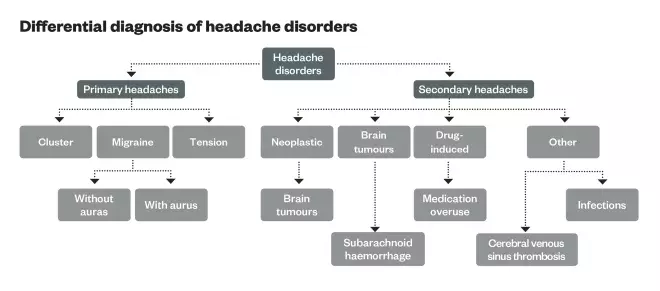
Patients presenting with a suspected migraine for the first time should be assessed to identify warning features suggestive of secondary headaches (see ‘Headache features requiring referral’). Any patients with warning features suggesting secondary headaches should be referred urgently to an appropriate specialist for further assessment[3]
. When referred, patients may receive a CT scan to rule out other diagnoses (see ‘Differential diagnosis of headache disorders’), such as subarachnoid haemorrhage, brain tumours or cerebral venous sinus thrombosis. The neurological symptoms associated with auras can mimic a stroke or a transient ischaemic attack (TIA). However, strokes and TIAs are usually sudden and an isolated manifestation, whereas migraine attacks will often start slowly, increasing in symptoms and intensity over minutes to hours. Strokes and TIAs should be excluded during diagnosis of migraine, particularly in older patients. A brain scan assists in excluding strokes and TIAs[1],[4]
.
| Headache features requiring referral |
|---|
| Source: British Association for the Study of Headaches[1] |
Warning features of headaches: New or unexpected headache Thunderclap headache (intense headache with abrupt or ‘explosive’ onset) Headache with atypical aura (duration >1 hour, or including motor weakness) Aura occurring for the first time during the use of combined oral contraceptives New onset headache in a patient >50 years or <10 years Persistent morning headache with nausea Progressive headache, worsening over weeks or longer Headache associated with postural change New onset headache in a patient with a history of cancer or HIV |
There are no specific diagnostic tests for migraines and diagnosis is based on patient history. Accuracy of diagnosis is improved by specialist assessment and review (see ‘Diagnostic criteria for migraine without aura’)[1]
.
Patients presenting with a suspected migraine should be asked to keep a diary of the attack pattern and frequency in order to aid diagnosis[1]
.
Prevention
Many patients associate their attacks with certain lifestyle triggers (see ‘Strategies for preventing trigger factors’)[1],[3]
. It is important to detect triggers by keeping a diary to establish a true contributing factor. Lifestyle changes should be encouraged in order to avoid triggers where possible, although the evidence to support the benefit of lifestyle advice is limited
[14]
.
Dietary sensitivities (e.g. to spicy foods or some alcoholic drinks) affect around 20% of migraine sufferers. A suspected trigger food is identified if the migraine occurs within six hours of consumption; if the effect is then reasonably reproducible; and if withdrawal leads to improvement of the attack.
Some patients experience a migraine upon relaxation, which gives rise to the common weekend migraine. Stress, a common predisposing factor, may induce a migraine (e.g. lack of sleep, missed meals and muscle tension)[1]
.
| Strategies for preventing trigger factors | |
|---|---|
| Trigger factors | Management |
Diet (e.g. spicy foods, certain alcoholic drinks and some cheeses) | Avoid any trigger foods detected as contributing to attacks. |
Change in habit (e.g. missing meals; sleep [too much or too little]; long distance travel) | Avoid changes in lifestyle and encourage regular meals. |
Hormone changes (menstruation) | Frovatriptan 2.5mg once a day or naratriptan 1mg twice a day, taken two days before day one of the menstrual cycle and continued for four to five days. |
Strenuous exercise or routine physical activity | Regular light exercise helps to promote a healthy lifestyle and well-being. |
Light: flashing light and bright light | Avoid sudden exposure to flashing lights (for example flash photography); use sunglasses where necessary to avoid bright lights. |
Muscle tension | Physiotherapy, acupuncture, heat and cold packs. |
Behaviour is a component of many headache triggers. Behavioural therapies are often used for prevention of headaches and can help towards coping with certain trigger factors. If stress or anxiety is a known contributing factor, stress management (e.g. relaxation therapy, stress reduction, coping strategies and cognitive behavioural therapy) should be considered as first-line treatment. Resolving underlying issues such as stress can help to promote the effectiveness of other treatments. Behavioural therapies are also good adjunctive treatment alongside drug options[1],[13]
.
Ph
ysical therapy can be used in acute treatment and also prevention of migraine, especially where they are associated with muscle tension, neck or head injury. Such therapies include physiotherapy, acupuncture, heat or cold packs and transcutaneous electrical nerve stimulation (TE
NS)[3],[13]
.
Acute treatment
The aim of ac
ute tre
atment is to control symptoms and improve quality of life. On first diagnosis, patients should begin with simple analgesia. However, if first-line options f
ail to control symptoms, then management sh
ould progress to 5HT
1 receptor agonists for symptom control of further attacks (see ‘Acute treatment of migraines’)[1],[3],[15]
.
Simple analgesia can be used as monotherapy or as a combination (paracetamol plus a non-steroidal anti-inflammatory drug [NSAID]), and is considered the treatment of choice for its cost-effectiveness and safety profile compared with second-line treatments[1]
. Currently, there are no studies to compare the relative efficacy of different NSAIDs[15]
. Therefore, if one NSAID is ineffective another may be trialled. Fast-releasing formulations, such as dispersible tablets or liquids, help to provide quicker absorption and therefore faster relief[1]
.
NSAIDs should only be used following a risk/benefit assessment in patients with bronchial asthma, renal and hepatic impairment, previous gastrointestinal ulcers, hypertension and congestive heart failure. Patients who have a risk of gastrointestinal damage may require regular protection (i.e. proton pump inhibitors). Where nausea and vomiting is an issue for patients, alternative formulations or anti-emetics should be recommended[1],[3]
.
| Acute treatment of migraines | |
|---|---|
| First-line treatment: simple analgesia | |
First choice | |
Second choice | Non-steroidal anti-inflammatory drugs (NSAIDs) |
5HT1 receptor agonists
cause vasoconstriction and block pain pathways in the brainstem[15]
.
They are c
ontraindicated in patients with ischaemic heart disease, previous myocardial infarction, coronary va
sospasm or uncontrolled or severe hypertension[2],[21]
. 5HT
1 receptor agonists have good evidenc
e to support the treatment of acute migraine attacks. They provide significant pain relief within two hours of administration and improve
a patient’s quality of life[3]
.
5HT
1 receptor agonists should be taken at the onset of migraines when pain is mild[22]
.
A single large dose is proven to be more effective than repetitive small doses[15]
;
however, 30% of patients fail to respond to any particular medicine in the class, which can be because of decreased absorption, poor compliance or individual biological variability[1]
.
Therefore, each 5HT
1 receptor agonist should be tried in at least three attacks before it is rejected for lack of efficacy[1]
.
Different doses or formulations shou
ld also be co
nsidered[1]
.
If a second dose of a 5HT
1 receptor agonist is required, it must be taken at least two hours after the first dose. Evidence is limited in the efficacy of a second dose for the same attack[21]
.
Regular use of 5HT
1 receptor agonists can increase the risk of overuse headaches and should be reviewed regularly[15]
.
| Second-line treatment: 5HT1 receptor agonists | |
|---|---|
First choice | Sumatriptan 50mg tablet[23]
|
Second choice | Almotriptan 12.5mg tablet or eletriptan 40–80mg tablet or rizatriptan 10mg tablet (also available as orodispersible tablets and wafers)[24]
|
Third choice | Zolmitriptan 2.5–5mg tablet (also available as orodispersible tablet and nasal spray)[25] |
Fourth choice | |
Migraine-associated gastric stasis
is a co
mmon symptom in migraine sufferers whereby gastric motion is inhibited, causing nausea and vomiting and reducing the absorption of medica
tion from the gastrointestinal tract[27]
.
Patients should be adv
ised to take medication as soon as an attack starts, as this is when absorption is least inhibited by gastric s
tasis.
Anti-emetics
should be used i
n patients with nausea and vomiting associated with migraine. Randomised placebo-controlled trials have shown prochlorperazine 3mg buccal tablets or metoclopramide 10mg tablets are the anti-emetics of choice for nausea and vomiting in migr
aine[29],[30]
. Domperidone can also be used, although the UK
Medicines and Healthcare products Regulatory Agency (MHRA) has advised that care must be taken because of the cardiac risks associate
d with its use[31]
.
Combination products containing an a
nti-emetic and analgesic are available on prescription (e.g. aspirin 900mg and metoclopramide 10mg; paracetamol 500mg and metoclopramide
5mg), and there is good evidence to support their use[3]
.
Metoclopramide 10mg is also useful as a prokinetic to help promote gastric emptying and manage gastric stasis[3],[15]
.
During an emergency
, for example an un
usually severe attack where normal acute migraine management has failed to provide relief, patients may require more aggressive approaches to treatment. Injectable 5HT
1-receptor agonists (sumatriptan 6mg subcutaneous injection), analgesia (diclofenac 75mg intramuscularly) and anti-emetics (chlorpromazine 25–50mg intravenously, metoclopramide 10–20mg intravenously, prochlorperazine 12.5mg intravenously) can
be used.
Opioids must not be used for treatment of migraine as they can delay recovery and can cause medicines overuse headaches.
R
ehydration with intravenous saline should be considered for patients experiencing a migraine in ho
spital[1],[15]
.
Prophylaxis
The management option of choice in
patien
ts with chronic migraines is prophylaxis. It can also be considered in patients with acute migraines in whom acute treatment options are contraindicated, ineffective, overused, or cause severe adverse effects.
The main goals of prophylaxis are to reduce the number, severity and duration o
f migraine attacks. The choice of drug should be made based on the patient’s comorbidities and the medicine’s side-effect profile (see ‘Medicine
s used in migraine prophylaxis’).
Preventative drug
s should be titrated slowly to an effective or maximum dose in order to minimise adverse effects. Doses should be trialled for 6–8 weeks after each titration. Migraines can be cyclical and therefore the drug chosen should be reviewed for consideration of withdrawal every 6–12
months
[1],[3],[14]
.
| Medicines used in migraine prophylaxis | ||
|---|---|---|
| * The National Institute for Health and Care Excellence suggests that topiramate and propranolol are first-line choices for prophylaxis in migraine[38] . | ||
| First-line treatment | Beta-blockers (oral treatment) | |
| First choice | Propranolol 40–240mg daily (in divided doses)[14] | |
| Second choice | Metoprolol 50–100mg twice a day or timolol 5–10mg twice a day[31] | |
| Third choice | Atenolol 20–100mg twice a day, or bisoprolol 5–10mg once daily, or nadolol 20–120mg twice a day[14] | |
| Beta-blockers are competitive antagonists of the effects of catecholamines at beta-adrenergic receptor sites, however in relation to migraines, the mode of action is not fully understood[33] . Beta-blockers are contraindicated in patients with asthma, heart failure, peripheral vascular disease, depression, diabetes and low blood pressure[32] . Propranolol increases the concentration of rizatriptan by 70% and therefore the dose of rizatriptan should be reduced appropriately[14] . | ||
| Second-line treatment | Antidepressants (oral treatment) | |
| First choice | Amitriptyline 10–150mg once a day at night[33] | |
| Second choice | Venlafaxine 75–150mg once daily[33] | |
| The migraine prophylaxis mode of action of amitriptyline and venlafaxine is not fully understood but related to inhibiting the neuronal reuptake of noradrenaline and serotonin in the central nervous system[34] . | ||
| Third-line treatment | Anti-epileptics (oral treatment) | |
| First choice | Topiramate 25–100mg twice a day*[33] | |
| The migraine prophylaxis mode of action of topiramate is not fully understood but it is thought to have sodium channel blocking action and cause inhibition of neurotransmitters[35] . Topiramate is contraindicated in patients with severe renal impairment (creatinine clearance <20ml/min) [36] . Doses should be reduced by 25–50% and adjusted according to the response [36] . Topiramate is an enzyme inducer, and therefore it can decrease the effects of the contraceptive pill. Other methods of contraception should be used. It is also contraindicated in pregnancy as it is teratogenic [35] . | ||
| Second choice | Sodium valproate 400–750mg twice a day[33] . | |
| The migraine prophylaxis mode of action of sodium valproate is not fully understood but it is thought to have inhibitory action on gamma amino-butyric acid[37] . It does not affect the efficacy of the contraceptive pill but other methods of contraception should be considered in combination as sodium valproate is contraindicated in pregnancy and breastfeeding[37] . | ||
Menstruation, contraception, pregnancy and the menopause
Menstrual migraines are associated with fluctuations of oestrogen during the menstrual cycle and are usually migraines without aura. Management should follow the same acute migraine treatments stated above. In addition to first-line options, mefenamic acid 500mg four times a day for simple analgesia can be used. For prophylaxis of menstrual migraines, frovatriptan 2.5mg once daily or naratriptan 1mg twice a day taken two days before day one of the menstrual cycle and for a further four to five days thereafter is recommended. Hormone replacement can be used to supplement hormones and there are different formulations available. Combined hormonal contraceptives (CHC) and the progestogen-only oral pill (POC) desogestrel can also be used to help regulate hormone levels throughout cycles by providing continuous hormone control. However, care must be taken as the CHC can cause headaches and this should be considered a contributing factor if headaches continue with use[1],[3]
.
Women s
uffering from migraines, particularly with aura, and using the combined oral contraceptive pill are at an increased risk of ischaemic stroke. Therefore, the decision regarding use of CHC is based on expert opinion and the risks should be discussed with the patient, before initiation of tr
eatment. H
owever, there is no increased risk of thrombotic event
s with POC and this may be the contraceptive of choice[1],[3]
.
In pregnancy,
paracetamol is the first-line analgesic of choice. Aspirin, naproxen and ibuprofen can be used in combination with paracetamol in the first and second trimester. Sumatriptan has been associated with safe use throughout pregnancy, although limited data is available. For prophylaxis, propranolol has the best evidence for safety in pregnancy. Amitriptyline at its lowest effective dose may also be used. Anti-epileptics should not be used
during pregnancy[1],[3]
.
Women at perim
enopause are at risk of developing migraines because of the fluctuations of oestrogen that occur. Hormone replacement therapy (HRT) should be considered to help stabilise hormone fluctuations and reduce migraine severity and frequency. If migraine attacks increase while the woman is on HRT, it should be discontinued[1],[3]
.
- This article was amended on 7 March 2016 to correct an error. Instead of using sumatriptan 6mg intravenously in an emergency, it should have stated sumatriptan 6mg subcutaneous injection.
Chandni Radia and Elizabeth Rawlence are senior clinical pharmacists at Kings College Hospital NHS Foundation Trust. Shelley Jones is clinical pharmacy team leader, neurosciences, Kings College Hospital NHS Foundation Trust.
References
[1] British Association for the Study of Headaches. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache, medication-overuse headache, 3rd edition 2010. Available at: www.bash.org.uk/wp-content/uploads/2012/07/10102-BASH-Guidelines-update-2_v5-1-indd.pdf (accessed June 2015).
[2] Steiner TJ, Scher AI, Stewart WF et al. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia, An International Journal of Headache 2003;23(7):519–527.
[3] Scottish Intercollegiate Guidelines Network (SIGN). Diagnosis and management of headache in adults; A national clinical guideline 2008. Available at: www.sign.ac.uk/pdf/sign107.pdf (accessed June 2015).
[4] Cutrer MF & Bajwa ZH. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults. Topic 3345 (version 25). UpToDate. 2015. Available at: www.uptodate.com/contents/pathophysiology-clinical-manifestations-and-diagnosis-of-migraine-in-adults (accessed June 2015).
[5] World Health Organization. The World Health Report, Mental Health: New Understanding, New Hope 2001. Available at: www.who.int/whr/2001/en/whr01_en.pdf?ua=1 (accessed July 2015).
[6] World Health Organization Media Centre. Headache disorders. Fact sheet No. 277. Oct 2012. Available at: www.who.int/mediacentre/factsheets/fs277/en/ (accessed July 2015).
[7] Goadsby PJ & Sprenger T. Migraine pathogenesis and state of pharmacological treatment options. BMC Medicine 2009;7:17.
[8] American Society of Headaches. Pathophysiology of Migraines . Available at: www.americanheadachesociety.org/assets/1/7/NAP_for_Web_-_Pathophysiology_of_Migraine.pdf (accessed July 2015).
[9] Charles A. Advances in the basic and clinical science of migraine. Ann Neurol 2009;65:491.
[10] Bartsch T & Goadsby PJ. Increased responses in trigeminocervical nociceptive neurons to cervical input after stimulation of the dura mater. Brain 2003;126:1801.
[11] Charles A. Vasodilation out of the picture as a cause of migraine headache. Lancet Neurol 2013;12:419.
[12] Panconesi A. Serotonin and migraine: a reconsideration of the central theory. J Headache Pain 2008;9:267.
[13] Bajwa ZH & Smith JH. Chronic migraine. Topic 3337 (version 20). UpToDate 2015. Available at: www.uptodate.com.libproxy.ucl.ac.uk/contents/chronic-migraine?source=search_result&search=migraine&selectedTitle=5%7E150 (accessed June 2015).
[14] Bajwa ZH & Smith JH. Preventive treatment of migraine in adults. Topic 3345 (version 25). UpToDate 2015. Available at: www.uptodate.com.libproxy.ucl.ac.uk/contents/acute-treatment-of-migraine-in-adults?source=search_result&search=migraine&selectedTitle=1%7E150 (a ccessed June 2015).
[15] Bajwa ZH & Smith JH. Acute treatment of migraine in adults. Topic 3347 (version 36). UpToDate 2015. Available at: www.uptodate.com.libproxy.ucl.ac.uk/contents/preventive-treatment-of-migraine-in-adults?source=search_result&search=migraine&selectedTitle=3%7E150 (accessed June 2015).
[16] Rabbie R, Derry S & Moore RA. Ibuprofen with or without an antiemetic for acute migraine headaches in adults. Cochrane Database of Systematic Reviews, [online] 4 (CD008039) 2013. Available at: www.ncbi.nlm.nih.gov/pubmed/20927770 (a ccessed 1 June 2015).
[17] Kirthi, V, Derry S, Moore RA et al. Aspirin with or without an antiemetic for acute migraine headaches in adults. Cochrane Database of Systematic Reviews [online] 4 (CD008041) 2013. Available at: www.ncbi.nlm.nih.gov/pubmed/20393963 (accessed June 2015).
[18] Derry S, Rabbie R & Moore RA. Diclofenac with or without an antiemetic for acute migraine headaches in adults. Cochrane Database of Systematic Reviews 2013;4(CD008783):1–43.
[19] Law S, Derry S & Moore RA. Naproxen with or without an antiemetic for acute migraine headaches in adults. Cochrane Database of Systematic Reviews 2013;4(CD009455):1–50.
[20] Myllylä VV, Havanka H, Herrala L et al. Tolfenamic acid rapid release versus sumatriptan in the acute treatment of migraine: comparable effect in a double-blind, randomized, controlled, parallel-group study. Headache 1998;38(6):201–207.
[21] Electronic Medicines Compendium. Sumatriptan 50mg film-coated tablets. Available at: www.medicines.org.uk/emc/medicine/751 (a ccessed July 2015).
[22] Goadsby PJ. The ‘Act when Mild’ (AwM) study: a step forward in our understanding of early treatment in acute migraine. Cephalalgia: An International Journal of Headache. 2008;28(2):36–41.
[23] Derry CJ, Derry S & Moore RA. Sumatriptan (all routes of administration) for acute migraine attacks in adults — overview of Cochrane reviews. Cochrane Database of Systematic Reviews 2014;4(CD009108);1–8.
[24] Ferrari MD, Roon KI, Lipton RB et al. Oral triptans (serotonin 5-HT(1B/1D) agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet 2001;358(9294):1668–1675.
[25] Rapoport AM, Ramadan NM, Adelman JU et al. Optimizing the dose of zolmitriptan (Zomig, 311C90) for the acute treatment of migraine. A multicenter, double-blind, placebo-controlled, dose range-finding study. The Journal of the American Academy of Neurology 1997;49(5):1210–1218.
[26] Mathew NT, Asgharnejad M, Peykamian M et al. Naratriptan is effective and well tolerated in the acute treatment of migraine. Results of a double-blind, placebo-controlled, crossover study. The Naratriptan S2WA3003 Study Group. The Journal of the American Academy of Neurology. 1997;49(6):1485–1490.
[27] Parkman HP. Migraine and Gastroparesis from a Gastroenterologist’s Perspective. The Journal of Head and Face Pain 2013;23(6):4–10.
[28] Tfelt-Hansen P, Henry P, Mulder LJ et al. The effectiveness of combined oral lysine acetylsalicylate and metoclopramide compared with oral sumatriptan for migraine. Lancet 1995;346(8980):923–926.
[29] Sharma S, Prasad A, Nehru R et al. Efficacy and tolerability of prochlorperazine buccal tablets in treatment of acute migraine. Headache 2002;42(9):896–902.
[30] Medicines and Healthcare products Regulatory Agency. Motilium 10 10mg Tablets and Motilium Instants 10mg – changed to prescription-only medicine. MDR 49-08/14. Available at: www.gov.uk/drug-device-alerts/drug-alert-motilium-10-10mg-tablets-and-motilium-instants10mg-changed-to-prescription-only-medicine (accessed July 2015).
[31] Silberstein SD, Holland S, Freitag F et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 2012;78(17):1337–1345.
[32] Martindale: The Complete Drug Reference. Beta-blockers . Available at: www.medicinescomplete.com/mc/martindale/current/6300-v.htm?q=betablockers&t=search&ss=text&p=1#_hit (a ccessed July 2015).
[33] Pringsheim T, Davenport WJ & Becker WJ. Prophylaxis of migraine headache. CMAJ 2010;182(7):E269–E276.
[34] Martindale: The Complete Drug Reference. Amitriptyline. Available at: www.medicinescomplete.com/mc/martindale/current/ms-12293-g.htm?q=tricyclic&t=search&ss=text&p=1#_hit (accessed July 2015).
[35] Electronic Medicines Compendium. Topiramate 50mg film-coated capsules . EMC 2014. Available at: www.medicines.org.uk/emc/medicine/23806 (accessed July 2015).
[36] Ashley C & Currie A. The Renal Handbook: third edition . Oxford: Radcliffe; 2009. Available at: www.renaldrugdatabase.com/ (accessed July 2015).
[37] Electronic Medicines Compendium. Epilim 200 Gastro-resistant tablets . EMC 2014. Available at: www.medicines.org.uk/emc/medicine/23021 (accessed July 2015).
[38] National institute for Health and Care Excellence. Headache in over 12s: diagnosis and management. NICE guidelines: short version. Draft for consultation, August 2015. Available at: www.nice.org.uk/guidance/indevelopment/gid-cgwave0744/consultation/headaches-standing-committee-b-update-addendum-consultation (accessed August 2015).


