Dana-Farber Harvard Cancer Center / National Cancer Institute / Science Photo Library
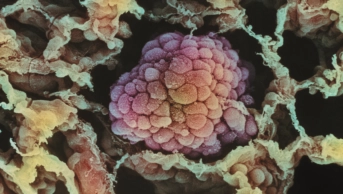
Multiple myeloma is a haematological cancer characterised by the overproduction of abnormal plasma cells in the bone marrow. The proliferation of the plasma cell clones and associated production of abnormal immunoglobulin (most commonly IgG) lead to a variety of clinical effects, including hypercalcaemia, skeletal damage, renal impairment, impaired haematopoiesis and increased susceptibility to infection (see ‘Box 1: presenting clinical features of multiple myeloma’)[1]
.
Box 1: Presenting clinical features of multiple myeloma
- Bone disease presenting as pain, pathological fractures;
- Renal impairment;
- Anaemia;
- Hypercalcaemia;
- Recurrent or persistent bacterial infection (often pneumococcal);
- Hyperviscosity.
Source: Bird JM, Owen RG, D’Sa S et al. Guidelines for the diagnosis and management of multiple myeloma 2014. London: 2014[1]
Multiple myeloma accounts for around 2% of all new cases of cancer in the UK with an annual age-adjusted incidence of 9.5 per 100,000 people[2]
. Incidence rates have increased by 14% in the past decade[2]
. The disease is slightly more common in men than in women and has a two-fold higher incidence in African–Americans compared with Caucasians[2]
, although the reasons for these ethnic differences are currently unknown. The incidence increases markedly with age: the median age at presentation is around 70 years[1]
, with only 15% of patients being <60 years old at diagnosis[1]
.
Even though the cause of multiple myeloma is not known, a number of risk factors (e.g. obesity, family history, autoimmune conditions, exposure to ionising radiation) have been associated with small increases in the risk of developing the disease[2]
. It is generally accepted that multiple myeloma almost always arises from an asymptomatic pre-malignant condition called monoclonal gammopathy of uncertain significance (MGUS)[2]
. However, what causes MGUS and what triggers its progression to multiple myeloma (the risk of progression for a patient with MGUS is around 1% per year) is not well understood.
Although it is currently regarded as being incurable in the majority of patients, the outlook for patients with a diagnosis of multiple myeloma has improved markedly in the past 40 years, with a quadrupling in survival rates over that time period[2]
. Five-year survival rates are now close to 50%, with a third of patients surviving for ten years or more[2]
. However, the natural history of myeloma remains very variable and this probably reflects the genetic heterogeneity of the disease. Risk stratification and developing more personalised treatments based on genetic-risk profiling are likely to become key aspects of clinical management in the future.
The significant advances in both treatment and supportive therapies for multiple myeloma that have contributed to improved outcomes will be the main focus of this article.
Treatment of newly diagnosed multiple myeloma
When deciding on a treatment plan for a newly diagnosed patient, the most important question to address is whether they are suitable for an autologous stem cell transplant (SCT). The cut-off age for such a procedure is usually between 60 and 70 years, although older patients with good performance status can be considered; the decision to proceed should be based on fitness, co-morbidities and patient preference[1],
[3]
. Organ dysfunction (e.g. significant renal impairment) is not a barrier to transplantation but may require modifications of chemotherapy doses.
The introduction of novel agents (e.g. thalidomide, bortezomib and lenalidomide) has produced significant survival benefits across all patient groups, but there is still considerable uncertainty about the optimal combination and sequence of therapies[1]
and, where possible, patients should be entered into clinical trials that are aiming to answer these questions. The choice of novel agent is primarily influenced by current guidance from the National Institute for Health and Care Excellence (NICE), England’s health technology assessment body[3]
. However, where there is more than one option available for a given patient, it is important for healthcare professionals to have an understanding of the toxicity profiles of these drugs, (see ‘table 1: side effect profile of commonly used agents in multiple myeloma’) as this can help guide treatment decisions.
| Table 1: Side effect profile of commonly used agents in multiple myeloma[1], [4] | |||
|---|---|---|---|
| Thalidomide | Bortezomib | Lenalidomide | |
| Neutropenia | No | No | Yes |
| Thrombocytopenia | No | Yes | Yes |
| Neuropathy | Yes | Yes | No |
| Constipation | Yes | Low risk | Low risk |
| Diarrhoea | No | Yes | Yes |
| Somnolence | Yes | No | No |
| Thrombotic risk | Yes | No | Yes |
Patients ineligible for autologous SCT
Around two-thirds of newly diagnosed multiple myeloma patients are not suitable for a SCT and, historically, the combination of oral melphalan and prednisolone (MP) was regarded as the standard of care in this patient population[5]
. However, large randomised trials have demonstrated that the MPT schedule (MP with 100–200mg/day thalidomide) improves overall survival[6],
[7]
. Similarly, an attenuated dose combination of cyclophosphamide, thalidomide and dexamethasone (CTDa) demonstrated superior response rates to MP in the Medical Research Council (MRC) Myeloma IX study[8]
.
Thalidomide in combination with an alkylating agent and corticosteroid may be considered to be the induction regimen of choice in older patients; thalidomide is both licensed and approved by NICE in this setting[9]
. In patients who cannot tolerate or have contraindications to thalidomide, NICE recommends a bortezomib-containing combination, usually VMP (bortezomib, melphalan and prednisolone). This regimen, classically involving twice-weekly bortezomib, demonstrated superiority over MP in the VISTA study[10]
, although it was associated with relatively high rates of myelosuppression and neuropathy. However, more recent studies have suggested that giving bortezomib once a week reduces the incidence of significant toxicities without loss of efficacy[11]
. There has also been a shift in recent years to administering bortezomib via the subcutaneous (SC) route as this has been shown to be clinically equivalent to intravenous (IV) administration but has fewer side effects, particularly peripheral neuropathy[12]
.
First-line lenalidomide, in combination with dexamethasone (Rd), may be superior to MPT in terms of both progression-free and overall survival[13]
and, although commonly used in other healthcare systems[14],
[15]
it is not currently NICE approved for this indication in the UK. For all the regimens discussed above, it is important to tailor doses and schedules to the fitness and frailty of the patient. One widely used approach is to use a scoring system that categorises patients into three groups (fit, unfit and frail), with different drug doses then being used within each group[14]
.
Patients eligible for autologous SCT
In the past decade, there has been a transition from regimens such as VAD (vincristine, doxorubicin and dexamethasone) that were historically considered the mainstay of induction therapy in younger patients[1]
and towards treatment schedules containing at least one novel agent because they are associated with improved response rates. For example, in the MRC Myeloma IX study, CTD (cyclophosphamide, thalidomide and dexamethasone) was superior to cyclophosphamide plus VAD (CVAD) in terms of both overall response rate (82.5% versus 71%) and complete response (CR) rate (13% versus 8%)[16]
. Other highly active regimens in this setting include bortezomib plus dexamethasone (VD)[17]
; bortezomib, thalidomide and dexamethasone (VTD)[18]
; and lenalidomide, bortezomib and dexamethasone (VRD)[19]
. The recently closed MRC Myeloma XI study was investigating whether induction regimens containing lenalidomide or lenalidomide and carfilzomib could improve on the responses seen with CTD. Current NICE guidance recommends bortezomib-based induction chemotherapy (VTD or VD)[3]
before an autologous SCT and this would, therefore, be considered standard care outside of clinical trials.
SCT
Although not given with curative intent, autologous SCT offers an improvement in survival in the region of 12 months when compared with conventional chemotherapy[20],
[21]
. The gold-standard conditioning agent for the past three decades has been IV melphalan[22]
, although there is interest in trying to improve efficacy by adding a second drug such as busulfan or bortezomib[14]
. Melphalan is given at a dose of 200mg/m2 but the dose should be reduced to 140mg/m2 in older or less fit patients, and in those with renal impairment (glomerular filtration rate <30ml/min)[1]
.
To build on the increased dose intensity afforded by autologous SCT, a number of studies have investigated the role of sequential or tandem autologous transplantation[23]
. However, in the UK, the most commonly used strategy is to collect sufficient stem cells for two procedures but delay the second transplant until the patient has actually relapsed[1]
. Evidence to support this approach comes from the recent National Cancer Research Institute (NCRI) Myeloma X study that demonstrated a 15-month survival advantage (median survival of 67 months versus 52 months) for a second autologous SCT, compared with consolidation chemotherapy with weekly cyclophosphamide, in patients who had received bortezomib-based re-induction therapy at first relapse[24]
. Recent NICE guidance recommends that a second autologous SCT is offered to patients who had a response to their first transplant of at least two years and is considered in patients with a shorter response duration (12–24 months) after their first transplant[3]
.
Currently, the only potentially curative option available to patients with multiple myeloma is allogeneic SCT. Conventional myeloablative conditioning would only be considered in the 2% of patients who are younger than 40 years at diagnosis but even then it is associated with a very high transplant-related mortality (TRM) in the region of 30–50%[25]
. Although the use of reduced-intensity conditioning (RIC) schedules may have the potential for a lower TRM (in the region of 10–20%), a recent meta-analysis[26]
demonstrated no survival advantage with an autologous followed by an allogeneic transplant when compared with the tandem autograft approach discussed previously. Consequently, allogeneic SCT is generally only offered in clinical trials but may be considered outside of a trial in younger patients with very high-risk disease[14]
.
The role of maintenance therapy
Given the clear benefits of novel agents in both newly diagnosed and relapsed myeloma, interest has grown in using them to maintain responses after autologous SCT. Thalidomide has demonstrated a modest survival benefit in this setting[27],
[28]
but concerns have been raised regarding the toxicity of long-term usage (particularly with doses >150mg/day) with one study reporting a rate of peripheral neuropathy of 75% in patients receiving the drug for >12 months[29]
. Encouraging data have recently emerged for both lenalidomide and bortezomib[30],
[31]
. For example, a meta-analysis presented at the 2016 American Society of Clinical Oncology (ASCO) conference analysed data from three large studies and demonstrated a significant improvement in overall survival at seven years with maintenance lenalidomide (10mg/day continuously or on days 1–21 of a 28-day cycle) compared with placebo (62% versus 50%, P =0.001)[31]
. More recently, data from the UK Myeloma XI study were presented at the 2016 American Society of Hematology (ASH) annual meeting, demonstrating a significant improvement in progression-free survival from 19 months with no maintenance to 37 months in patients receiving lenalidomide 10mg daily on days 1–21 of a 28-day cycle[32]
. There was an excess incidence of secondary primary malignancies in the lenalidomide group, as had been reported previously[31]
, but it is felt that this small risk is far outweighed by the survival benefits associated with lenalidomide. In the UK, although lenalidomide has recently received a license extension for maintenance therapy, none of the above agents are currently NICE-approved in this setting.
Management of relapsed disease
Almost all patients with myeloma will eventually relapse at some point after their initial therapy. A number of factors (e.g. previous therapy, duration of first remission, performance status of patient and any previous drug-induced toxicities)[14]
can help guide treatment choices at this point. Current NICE guidance recommends bortezomib at first relapse, with the option of a second autologous SCT for eligible patients who respond to re-induction therapy and who had a response duration of at least 12 months after their first transplant[3]
. Lenalidomide (plus dexamethasone) is recommended at second relapse, based on the results of the MM009 and MM010 studies that demonstrated a 6.4 months survival advantage for the combination over dexamethasone alone[33]
. Lenalidomide is given at a dose of 25mg/daily for 21 days of a 28-day cycle, although dose reductions are mandatory in the setting of renal impairment. Dexamethasone is commonly given at a dose of 40mg once weekly, because this schedule may be superior to the higher dose schedule used in the above studies[34]
. However, less fit patients may only be able to tolerate doses in the region of 10–20mg weekly (as discussed earlier)[14]
.
NICE have recently approved the combination of panobinostat (an oral histone deacetylase inhibitor) in combination with bortezomib and dexamethasone in patients who have received at least two previous lines of treatment including bortezomib and an immunomodulatory agent[35]
. Although the pivotal trial (PANORAMA 1) demonstrated a significant improvement in progression-free survival (12 months versus 8.1 months), the recently published overall survival analysis failed to show a statistically significant improvement in median survival (40.3 months versus 35.8 months, P =0.54)[36]
. Panobinostat is associated with a high incidence of grade 3 diarrhoea (25% in PANORAMA 1) and some clinicians would advise using lower dose schedules to improve tolerability[37]
. The immunomodulatory drug pomalidomide has demonstrated encouraging activity (a median survival advantage of five months when compared with high-dose dexamethasone alone) in patients who have failed treatment with both bortezomib and lenalidomide[38],
[39]
. It was recently approved by NICE as a fourth-line option in these patients[40]
.
New drugs for multiple myeloma
A number of promising new agents for multiple myeloma have recently been approved by the European Medicines Agency, the agency that evaluates medicinal products for use in Europe, or are likely to be approved in the next few months (‘Table 2: recent treatment advances for multiple myeloma’). Although none are currently approved by NICE, there is an expectation that some of them may soon enter routine clinical practice in the UK.
| Table 2: Recent treatment advances for multiple myeloma | ||||
|---|---|---|---|---|
| Drug | Class | Administration | European Medicines Agency approval | References |
| Carfilzomib | Proteosome inhibitor | Intravenous | Yes | [41], [42] |
| Daratumumab | Monoclonal antibody | Intravenous | Yes | [43], [44], [45] |
| Elotuzumab | Monoclonal antibody | Intravenous | Yes | [46] |
| Ixazomib | Proteosome inhibitor | Oral | Yes | [47] |
Supportive therapies for multiple myeloma
Comprehensive UK guidelines for supportive care in multiple myeloma were published in 2011[48]
and the recent NICE myeloma guidelines[3]
include a section on preventing and managing various complications of the disease. Only some of the key areas can be briefly discussed in the following section, therefore, the reader is encouraged to refer to the NICE guidelines for more in-depth guidance and coverage of topics such as management of renal failure, pain control, fatigue and end-of-life care.
Thromboprophylaxis
Although a cancer diagnosis is associated with an increased risk of thromboembolic events, patients with multiple myeloma are at a particularly high risk of venous thromboembolism (VTE) (around 9%)[48]
because of a number of disease-specific factors such as elevated immunoglobulin levels and an increase in blood viscosity. This risk is increased further (to 15–25%) in those patients who receive immunomodulatory drugs in combination with a corticosteroid or cytotoxic drug, particularly in the first-line setting[49]
. Patients can be stratified into risk groups according to the number of thrombotic risk factors present (e.g. obesity, immobility, previous VTE). Therapeutic warfarin (target international normalised ratio 2–3) or low molecular weight heparin (LMWH) are recommended by NICE[3]
, although there are currently no randomised trial data to determine which of these two options is preferable. Importantly, there is no evidence to support the use of fixed, low-dose warfarin schedules in this setting[50]
. In those patients for whom LMWH or warfarin are deemed unsuitable or who have achieved an optimal response to their immunomodulatory drug and are classified as low risk, low-dose aspirin can be considered[3]
.
Anti-infectives
Multiple myeloma patients are at increased risk of infection[1]
: this is related to the disease and its effect on the immune response, as well as the use of high-dose corticosteroids as a treatment modality. Although patients are susceptible to infections, such as Streptococcus pneumoniae and Haemophillus influenzae, broad-spectrum antibiotic prophylaxis is not currently recommended[2]
but a large UK trial is currently investigating the benefits of prophylactic levofloxacin (the TEAMM study). Immunoglobulin replacement is an option for patients who have recurrent infections and who are found to be hypogammaglobulinaemic[3]
(recommended dose 0.2–0.4mg/kg every 3–4 weeks).
In patients receiving high-dose corticosteroids, lymphopenia is a common side effect, therefore, co-trimoxazole (960mg three times a week) is widely used as Pneumocystis carinii pneumonia prophylaxis. In addition, patients receiving lenalidomide or bortezomib-based treatment should receive prophylactic aciclovir because of an increased risk of varicella zoster infection.
Bisphosphonates
Bone disease affects up to 90% of multiple myeloma patients[1]
and is associated with a variety of complications, including fractures, spinal cord compression and hypercalcaemia. The bisphosphonates sodium clodronate, zoledronic acid and disodium pamidronate have been shown to reduce skeletal-related events (SREs) in patients with symptomatic multiple myeloma[51]
. Zoledronic acid is currently regarded as the drug of choice[3]
based on the beneficial effect on overall survival demonstrated by monthly zoledronic acid infusions in the MRC Myeloma IX study[52]
. When compared with oral sodium clodronate, zoledronic acid had a greater impact on SREs and significantly increased overall survival (50 months compared with 44.5 months). It was, however, associated with an increased risk of osteonecrosis of the jaw, a rare but potentially serious complication of all bisphosphonates, particularly when given intravenously. Consequently, it is recommended that all patients should be reviewed by a dentist and any necessary dental procedures undertaken before starting treatment with a parenteral bisphosphonate[3]
. Renal function must also be closely monitored in these patients because doses and administration rates may need to be adjusted in the setting of renal impairment.
Management of anaemia
Anaemia is an extremely common complication of myeloma, occurring in 75–85% of patients[48]
. In patients with anaemia associated with renal failure or symptomatic anaemia, consideration can be given to erythropoietin treatment, with the aim of maintaining a haemoglobin level of 110–120g/l[3]
.
Management of peripheral neuropathy
Up to a third of myeloma patients may already have subclinical peripheral neuropathy at diagnosis[48]
and this is often made worse by the use of the novel chemotherapy drugs, thalidomide and bortezomib. Both are associated with rates of peripheral neuropathy in the range of 33–75%[48]
, consequently, close monitoring of patients for early signs of neuropathy is mandatory. In patients who develop neuropathy, dose reduction or even discontinuation of the offending drug is necessary. For example, in patients receiving twice weekly bortezomib, switching to a once weekly schedule is widely recommended[3],
[48]
. Management options for painful neuropathy include gabapentin or pregabalin, either alone or in combination with an opioid[48]
. Vitamin B supplementation (with pyridoxine and cyanocobalamin) is often prescribed but there is limited evidence of clinical benefit, therefore, this approach is not routinely recommended[48]
.
Financial and conflicts of interest disclosure
The author has received advisory board and consultancy honoraria from Celgene, Amgen, Janssen and Takeda, all of whom have myeloma drugs licensed in the UK. No writing assistance was used in the production of this manuscript.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Bird JM, Owen RG, D’Sa S et al. Guidelines for the diagnosis and management of multiple myeloma 2014. London: 2014. Available at: https://academy.myeloma.org.uk/library/guidelines/bcshukmf/ (accessed March 2017)
[2] Cancer Research UK. Myeloma statistics. Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/myeloma (accessed March 2017)
[3] National Institute for Health and Care Excellence. Myeloma: diagnosis and management. NICE guideline [NG35]. Available at: https://www.nice.org.uk/guidance/ng35 (accessed March 2017)
[4] Pawlyn C, Khan M, Muls A et al. Lenalidomide-induced diarrhoea in patients with myeloma is caused by bile acid malabsorption that responds to treatment. Blood 2014;124: 2467–2468. doi: 10.1182/blood-2014-06-583302
[5] Harousseau J & Dreyling M. Multiple myeloma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010; 21 (suppl 5); v155-v157. doi: 10.1093/annonc/mdq178
[6] Facon T, Mary JY, Hulin C et al. Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99-06): a randomised trial. Lancet 2007;370:1209–1218. doi: 10.1016/S0140-6736(07)61537-2
[7] Hulin C, Facon T, Roden P et al. Efficacy of melphalan and prednisone plus thalidomide in patients older than 75 years with newly diagnosed multiple myeloma: IFM 01/01 trial. J Clin Oncol 2009;27:3664–3670. doi: 10.1200/JCO.2008.21.0948
[8] Morgan G, Davies F, Gregory W et al. Cyclophosphamide, thalidomide, and dexamethasone (CTD) as initial therapy for patients with multiple myeloma unsuitable for autologous transplantation. Blood 2011;118:1231–1238. doi: 10.1182/blood-2011-02-338665
[9] National Institute for Health and Care Excellence. Bortezomib and thalidomide for the first line treatment of multiple myeloma. Technology appraisal guidance [TA228]. Available at: https://www.nice.org.uk/guidance/ta228 (accessed March 2017)
[10] San Miguel J, Richardson P, Sonneveld P et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med. 2008;359:906–917. doi: 10.1056/NEJMoa0801479
[11] Mateos M, Oriol A, MartÃnez-López J et al. Bortezomib, melphalan, and prednisone versus bortezomib, thalidomide, and prednisone as induction therapy followed by maintenance treatment with bortezomib and thalidomide versus bortezomib and prednisone in elderly patients with untreated multiple myeloma: a randomised trial. Lancet Oncol 2010;11:934–941. doi: 10.1016/S1470-2045(10)70187-X
[12] Moreau P, Pylypenko H, Grosicki S et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol 2011;12:431–440. doi: 10.1016/S1470-2045(11)70081-X
[13] Benboubker L, Dimopoulos MA, Dispenzieri A et al. Lenalidomide and dexamethasone in transplant-ineligible patients with myeloma. N Engl J Med. 2014; 371: 906–17. doi: 10.1056/NEJMoa1402551
[14] Ludwig H, Sonneveld P, Davies F et al. European perspective on multiple myeloma treatment strategies in 2014. Oncologist 2014;19:829–844. doi: 10.1634/theoncologist.2014-0042
[15] Rajkumar SV & Kumar S. Multiple myeloma: diagnosis and treatment. Mayo Clin Proc 2016;91:101–119. doi: 10.1016/j.mayocp.2015.11.007
[16] Morgan G, Davies F, Gregory W et al. Cyclophamide, thalidomide, and dexamethasone as induction therapy for newly diagnosed multiple myeloma patients destined for autologous stem-cell transplantation: MRC Myeloma IX randomized trial results. Haematologica 2012;97:442–450. doi: 10.3324/haematol.2011.043372
[17] Harousseau J, Attal M, Avet-Loiseau H et al. Bortezomib plus dexamethasone is superior to vincristine plus doxorubicin plus dexamethasone as induction treatment prior to autologous stem-cell transplantation in newly diagnosed multiple myeloma: results of the IFM 2005-01 phase III trial. J Clin Oncol 2010;28:4621–2629. doi: 10.1200/JCO.2009.27.9158
[18] Cavo M, Tacchetti P, Patriarca F et al. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet. 2010;376:2075–2085. doi: 10.1016/S0140-6736(10)61424-9
[19] Richardson PG, Weller E, Lonial S et al. Lenalidomide, bortezomib and dexamethasone combination therapy in patients with newly diagnosed multiple myeloma. Blood 2010;116:679–686. doi: 10.1182/blood-2010-02-268862
[20] Attal M et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma: Intergroupe Francais du Myélome. N Engl J Med. 1996;335:91–97. doi: 10.1056/NEJM199607113350204
[21] Child JA et al. High-dose chemotherapy with hematopoietic stem cell rescue for multiple myeloma. N Engl J Med 2003;348:1875–1883. doi: 10.1056/NEJMoa022340
[22] McElwain T & Powles R. High-dose intravenous melphalan for plasma-cell leukaemia and myeloma. Lancet 1983;2(8354):822–824. doi: 10.1016/S0140-6736(83)90739-0
[23] Kumar A, Kharfan-Dabaja M, Glasmacher A et al. Tandem versus single autologous hematopoietic cell transplantation for the treatment of multiple myeloma: a systematic review and meta–analysis. J Natl Cancer Inst 2009;101:100–106. doi: 10.1093/jnci/djn439
[24] Cook G, Ashcroft AJ, Cairns DA et al. The effect of salvage autologous stem-cell transplantation on overall survival in patients with relapsed multiple myeloma (final results from BSBMT/UKMF Myeloma X Relapse [Intensive]): a randomised, open-label, phase 3 trial. Lancet Haematol 2016; 3:340–351. doi: 10.1016/S2352-3026(16)30049-7
[25] Lokhorst H, Einsele H, Vesole D et al. International Myeloma Working Group consensus statement regarding the current status of allogeneic stem cell transplantation for multiple myeloma. J Clin Oncol 2010;28:4521–4530. doi: 10.1200/JCO.2010.29.7929
[26] Kharfan-Dabaja MA, Hamadani M, Reljic T et al. Comparative efficacy of tandem autologous versus autologous followed by allogeneic hematopoietic cell transplantation in patients with newly diagnosed multiple myeloma: A systematic review and meta-analysis of randomized controlled trials. J Hematol Oncol 2013:6:2. doi: 10.1186/1756-8722-6-2
[27] Attal M, Harousseau JL, Leyvraz S et al. Maintenance therapy with thalidomide improves survival in patients with multiple myeloma. Blood. 2006;108:3289–3294. doi: 10.1182/blood-2006-05-022962
[28] Spencer A, Prince HM, Roberts AW et al. Consolidation therapy with low-dose thalidomide and prednisolone prolongs the survival of multiple myeloma patients undergoing a single autologous stem-cell transplantation procedure. J Clin Oncol. 2009;27:1788–1793. doi: 10.1200/JCO.2008.18.8573
[29] Tosi P, Zamagni E, Cellini C et al. Neurological toxicity of long-term (>1 yr) thalidomide therapy in patients with multiple myeloma. Eur J Haematol 2005;74:212–216. doi: 10.1111/j.1600-0609.2004.00382.x
[30] Sonneveld P, Schmidt-Wolf IG, van der Holt B et al. Bortezomib induction and maintenance treatment in patients with newly diagnosed multiple myeloma: results of the randomized phase III HOVON-65/ GMMG-HD4 trial. J Clin Oncol. 2012;30:2946–2955. doi: 10.1200/JCO.2011.39.6820
[31] Attal M, Palumbo A, Holstein SA et al. Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant in multiple myeloma: a meta analysis of overall survival. J Clin Oncol 2016;34:(suppl: abstr 8001).
[32] Jackson GH, Davies FE, Pawlyn C et al. Lenalidomide is a highly effective maintenance therapy in myeloma patients of all ages; results of the Phase III Myeloma XI Study. Blood 2016 128:1143.
[33] Dimopoulos MA, Chen C, Spencer A et al. Long-term follow-up on overall survival from the MM-009 and MM-010 phase III trials of lenalidomide plus dexamethasone in patients with relapsed or refractory multiple myeloma. Leukemia. 2009;23:2147–2152. doi: 10.1038/leu.2009.147
[34] Rajkumar S, Jacobus S, Callander N et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 2010;11:29–37. doi: 10.1016/S1470-2045(09)70284-0
[35] National Institute for Health and Care Excellence. Panobinostat for treating multiple myeloma after at least 2 previous treatments. NICE technology appraisal guidance [TA380]. Available at: https://www.nice.org.uk/guidance/ta380 (accessed March 2017).
[36] San-Miguel JF, Hungria VT, Yoon SS et al. Overall survival of patients with relapsed multiple myeloma treated with panobinostat or placebo plus bortezomib and dexamethasone (the PANORAMA 1 trial): a randomised, placebo-controlled, phase 3 trial. Lancet Haematol 2016 Oct 14. pii: S2352-3026(16)30147-8. doi: 10.1016/S2352-3026(16)30147-8
[37] Rajkumar SV. Panobinostat for the treatment of multiple myeloma. Lancet Oncol 2014:15:1178–1179. doi: 10.1016/S1470-2045(14)70443-7
[38] San Miguel J, Weisel K, Moreau P et al. Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory multiple myeloma (MM-003): a randomised, open-label, phase 3 trial. Lancet Oncol 2013;14:1055–1066. doi: 10.1016/S1470-2045(13)70380-2
[39] Dimopoulos MA, Weisel KC, Song KW et al. Cytogenetics and long-term survival of patients with refractory or relapsed and refractory multiple myeloma treated with pomalidomide and low-dose dexamethasone. Haematologica 2015;100:1327–1333. doi: 10.3324/haematol.2014.117077
[40] National Institute for Health and Care Excellence. Pomalidomide for multiple myeloma previously treated with lenalidomide and bortezomib. Technology appraisal guidance [TA427]. Available at: https://www.nice.org.uk/guidance/ta427 (accessed March 2017)
[41] Stewart AK, Rajkumar SV, Dimopoulos MA et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med 2015;372:142–152. doi: 10.1056/NEJMoa1411321
[42] Dimopoulos MA, Moreau P, Palumbo A et al. Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol 2016;17:27–38. doi: 10.1016/S1470-2045(15)00464-7
[43] Lonial S, Weiss BM, Usmani SZ et al. Daratumumab monotherapy in patients with treatment-refractory multiple myeloma (SIRIUS): an open-label, randomised, phase 2 trial. Lancet 2016;387:1551–1560. doi: 10.1016/S0140-6736(15)01120-4
[44] Palumbo A, Chanan-Khan A, Weisel K et al. Daratumumab, Bortezomib and Dexamethasone for Multiple Myeloma. N Engl J Med 2016;375:754–766. doi: 10.1056/NEJMoa1606038
[45] Dimopoulos, MA, Oriol A, Nahi H et al. Daratumumab, Lenalidomide, and Dexamethasone for Multiple Myeloma. N Engl J Med 2016; 375:1319–1133. doi: 10.1056/NEJMoa1607751
[46] Lonial S, Dimopoulos M, Palumbo A et al. Elotuzumab therapy for relapsed of refractory multiple myeloma. N Engl J Med 2015;373:621–631. doi: 10.1056/NEJMoa1505654
[47] Moreau P, Masszi T, Grzasko N et al. Oral ixazomib, lenalidomide and dexamethasone for multiple myeloma. N Engl J Med 2016;374:1621–1634. doi: 10.1056/NEJMoa1516282
[48] Snowden J, Ahmedzai S, Ashcroft J et al. Guidelines for supportive care in multiple myeloma 2011. Br J Haematol 2011;154:76–103. doi: 10.1111/j.1365-2141.2011.08574.x
[49] Zamagni E, Brioli A, Tacchetti P et al. Multiple myeloma, venous thromboembolism and treatment-related risk of thrombosis. Seminars in thrombosis and haemostasis 2011;37:209–219. doi: 10.1055/s-0031-1273085
[50] Zangari M, Barlogie B, Anaisse E et al. Deep vein thrombosis in patients with multiple myeloma treated with thalidomide and chemotherapy: effects of prophylactic and therapeutic anticoagulation. Br J Haematol 2004;126:715–721. doi: 10.1111/j.1365-2141.2004.05078.x
[51] Terpos E, Sezer P, Croucher P et al. The use of bisphosphonates in multiple myeloma: recommendations of an expert panel on behalf of the European Myeloma Network. Ann Oncol 2009;20:1303–1317. doi: 10.1093/annonc/mdn796
[52] Morgan G, Davies F, Gregory W et al. First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet 2010;376:1989–1999. doi: 10.1016/S0140-6736(10)62051-X