Du Cane Medical Imaging Ltd / Science Photo Library
In this article you will learn:
- The most common risk factors for falls
- Medicines that can contribute to risk of falls
- How to reduce a patient’s risk of falls
Around 14% of the UK population are aged 65 years and older, and this is projected to rise to 22% by 2030[1]
. Around one in three people aged over 65 years falls at least once a year. This increases to around 50% of people older than 75 years[2]
.
Older adults who fall are up to three times more likely to fall again within a year[2]
. Falls are 30% more common in people living in residential homes than in the community[3]
, and there are 3–14 falls per 1,000 bed days in acute hospital and community mental health units[4]
. As older patients recover more slowly, falls often result in long hospital stays where patients can become vulnerable to complications or infections.
The NHS receives around 750,000 calls from older adults who have fallen each year, with each ambulance call-out estimated to cost around £115[5]
. Overall, falls are estimated to cost the NHS more than £2.3bn per year[6]
.
Falls also have a significant human cost. In addition to pain and distress, after a fall the patient may feel a loss of dignity and have a reduced quality of life and independence. Falls also affect the patient’s family and carers, and can result in time off work or additional care requirements.
Risk factors
There are many distinct causes for falls in older people[7]
. These can be classified as either intrinsic (person-specific) or extrinsic (environmental). Falls often result from a combination of risk factors, and a patient’s fall risk rises as they grow older and gain additional comorbidities.
In the UK, falls in patients aged over 60 years are more common in women and people living in areas of social deprivation[8]
. A recent review from the United States found that people of white ethnicity were more likely to experience a fall than those of Chinese, African American, American Hispanic and Asian-born American ethnicity[9]
.
Gait and balance impairment are consistently identified as one of the strongest risk factors for falls. Body-orientating reflexes, muscle strength and tone, and stepping height all usually decline with age, and older people often have stiffer and less coordinated gaits, with poorer posture control, compared with younger people. Gait problems can also be caused by comorbidities affecting the nervous, muscular, skeletal, circulatory, and respiratory systems, or from simple loss of muscle tone and endurance due to a period of inactivity. This means older people tend to be unable to avoid falls by shifting their weight at the hip, and instead of taking one smooth step often take several smaller, unsteady steps.
Cognitive impairment can increase a patient’s risk of falling. This relationship is more pronounced in older patients with neurological comorbidities such as Alzheimer’s disease, Parkinson’s disease or a history of stroke.
Visual impairment is another important risk factor[7] ,[10]
. Problems with visual acuity, contrast sensitivity or visual field, caused by conditions such as a cataract, glaucoma and macular degeneration can all contribute to misjudgement of distance and misinterpretation of spatial information. Older people who use bifocal and multi-focal glasses are also at increased risk of falls[11]
.
Dizziness is a risk factor that can be caused by many different clinical conditions, but is due to vestibular disorders in around 45% of patients[12]
. Possible causes of dizziness-related falls in older people include benign paroxysmal positional vertigo, migraine, Ménière’s disease or a long period of inactivity.
Chronic diseases can often increase risk of falls, usually by causing one of the problems listed above. For example, patients with neurological diseases such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis or stroke experience falls more frequently, which are mainly attributed to changes in their gait pattern[7]
.
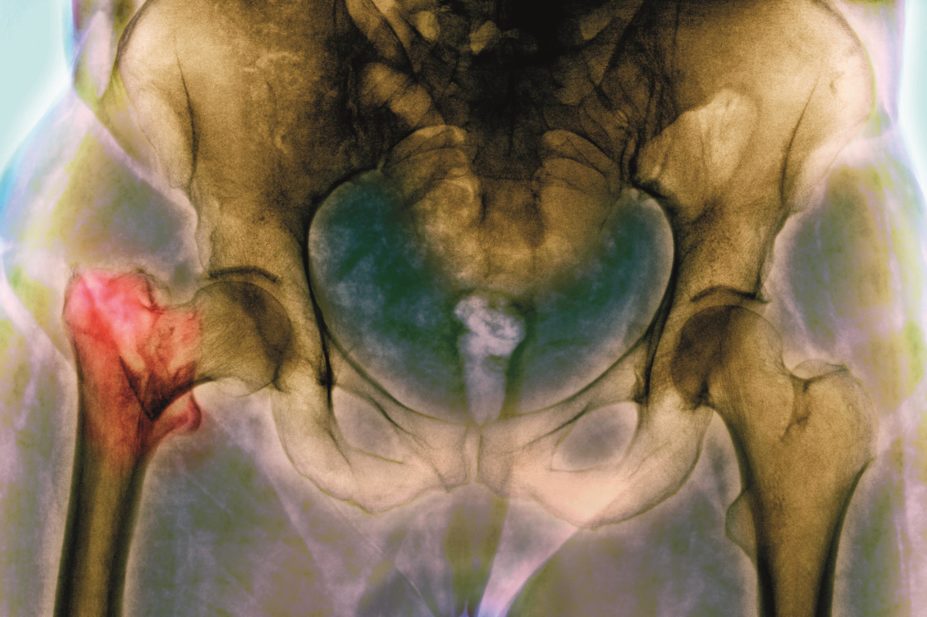
Arthritis and rheumatic disease is the most common group of chronic conditions in people aged over 65 years in the UK[1]
. Patients with these conditions have up to a five-fold increase in risk of falls, probably due to gait impairment and muscle weakness.
Cardiovascular disease is the second most common group of chronic conditions in patients aged over 65 years in the UK[1]
, and older people with cardiac conditions who fall have greater mortality rates than those with no cardiovascular condition[13]
. Atrial fibrillation has been identified as an independent risk factor for non-accidental falls in older people. This may be due to decreased carbon dioxide, co-existing sinus node disease and impaired baroreflex in these patients. There is a small association between older people with hypertension and poor balance and gait.
Postural hypotension, which can cause patients to lose consciousness and fall, is more common in older people and is estimated to affect up to 30% of those aged over 65 years, up to 60% of Parkinson’s disease sufferers and up to 70% of nursing home residents[14]
.
Other long-term conditions associated with falls include depression, diabetes and urinary incontinence[7]
.
Medicines can often increase the risk of falls (see ‘Medicines most commonly associated with falls in older people’).
| Class | Examples |
|---|---|
Antihypertensives | ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, hydralazine, methyldopa |
Diuretics | bendroflumethiazide, furosemide, co-amilofruse |
Beta-blockers | propranolol, timolol |
Antidepressants | sertraline, trazodone, dosulepin, amitriptyline |
Benzodiazepines | diazepam, temazepam, chlordiazepoxide |
Antipsychotics | chlorpromazine, flupentixol, haloperidol, olanzapine, quetiapine, risperidone |
Other sedatives and hypnotics | sleeping aids (e.g. zopiclone, nitrazepam), sedating antihistamines (e.g. diphenhydramine, promethazine) |
Opioids | morphine, buprenorphine, diamorphine, fentanyl, methadone, oxycodone, tramadol, codeine |
NSAIDs | diclofenac, ibuprofen |
Psychotropic drugs are often linked with an increased risk of falls. This includes antidepressants, drugs to treat bipolar disorder or dementia, anxiolytics and hypnotics, antipsychotics and benzodiazepines[15]
.
Patients who use insulin have been shown to be at increased risk of falls[7]
. Oral anti-diabetic medicines are not directly linked to falls, although fractures are more common after a fall in patients with diabetes, particularly in those taking thiazolidinediones.
Several cardiovascular medicines are also associated with a higher risk of falls. This includes digoxin, type 1A antiarrythmics (for example, quinidine), diuretics and angiotensin converting enzyme (ACE) inhibitors[7]
. Thiazide diuretic use is an independent risk factor for falls, and the risk of a fall is greatest in the first three weeks after starting treatment[16]
. Older patients are at increased risk of falls the day after any diuretic has been changed or the dose has increased.
Antiepileptic medicines are associated with an increased risk of falls not related to seizures. Postmenopausal women are particularly at risk of falls when taking antiepileptic medicines[7]
.
Environmental factors play an important role in contributing to fall risk in the home or immediate home surroundings, as well as in hospitals[6] ,[7]
. It is important to ensure that aspects of the home or hospital environment that could raise patients’ risk of falling are systematically reviewed and addressed[6]
.
Inappropriate or ill-fitting footwear, or walking barefoot, can affect a patient’s postural stability and is associated with accidental falls[7]
.
Falls assessment
The purpose of a falls assessment is to identify those at risk of falling so that effective interventions, tailored to the patients’ needs, can be offered[6]
.
A number of assessment tools have been developed for use in specific settings such as for community residents, care homes or hospitals but they vary in detail and administration[3] ,[6]
. None have been used or validated across Europe, and it is not possible to state which tool is the most useful. Multifactorial assessments for community or care home-residing older adults commonly include a medical, medication review, functional, daily living activities, psychosocial and environmental hazards[6]
.
Falls prediction tools, such as STRATIFY and Morse, are used in hospitals to attempt to identify older inpatients at risk of falling during their hospital stay. However, falls prediction tools are not recommended by NICE because they are rarely validated across relevant settings and do not consistently discriminate between fallers and non-fallers in that specific population[6]
. This renders their validity and reliability uncertain, and they can be misleading and harmful. It is therefore better to focus on interventions that are available and ensure they can be provided to patients who will benefit from them.
Risk reduction
It is difficult to make definitive recommendations on how to reduce a patient’s risk of falls. Three key studies have been highlighted by NICE[6]
as examples of good practice. These all used a multifactorial approach, which included detailed assessment of the fall by a physician and occupational therapist or physiotherapist, assessment (and necessary modification) of the patient’s home, a medicines review, an exercise programme and patient advice.
Physical exercise or therapy is a key part of reducing a patient’s fall risk. Recent systematic reviews have found a programme of exercise alone, or associated with other interventions such as medicines management or urinary incontinence management, can reduce both the number of falls and risk of falling[6]
. Exercise therapy was beneficial for both community-dwelling older adults and hospital inpatients. Combined balance re-training and muscle strengthening has also been shown to reduce risk of falls. The only single exercise activity found to reduce the risk of falling is Tai Chi[17]
.
There is no evidence that taking vitamin D supplements (with or without calcium) helps reduce the risk of falls in older people. However, limited data suggest vitamin D analogues such as calcitrol and alfacalcidol may be effective[17]
.
Withdrawal of psychotropic medicines significantly reduces the rate of falls[17]
.
Pharmacist-led interventions, such as medicines use reviews, have been shown to improve patient education, and medicines use. However, they have not been shown to reduce rates of falls or risk of falling[18]
. An important barrier to pharmacist-led fall risk reduction programmes appears to be the lack of responsiveness from prescribers to the pharmacist’s advice[19]
.
Supriya Kapas LLB, PhD, MRPharmS, FHEA is specialist clinical pharmacist at the Midlands Centre for Spinal Injuries, The Robert Jones & Agnes Hunt Orthopaedic NHS Foundation Trust.
References
[1] Office for National Statistics. Health and social care [Online]. Available at: http://www.ons.gov.uk/ons/taxonomy/index.html?nscl=Health+and+Social+Care.
[2] Todd C, Skelton D. What are the main risk factors for falls among older people and what are the most effective interventions to prevent these falls? Health Evidence network report. Copenhagen: WHO Regional Office for Europe 2004.
[3] Cameron ID, Gillespie LD, Robertson, MC et al. Interventions for preventing falls in older people in care facilities and hospitals (Cochrane Review). The Cochrane Library. Issue 12. John Wiley & Sons, Ltd. 2012.
[4] Healey F, Scobie S, Oliver D et al. Falls in English and Welsh hospitals: a national observational study based on retrospective analysis of 12 months of patient safety incident reports. Quality and Safety in Health Care. 2008;17:424–430.
[5] Department of Health. Falls and fractures: effective interventions in health and social care. London: Department of Health. 2009.
[6] National Institute for Health and Care Excellence. Falls. Assessment and prevention of falls in older people. Clinical guideline 161. London. National Institute for Health and Care Excellence 2013.
[7] Ambrose AF, Paul G & Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75:51–61.
[8] Gribbin J, Hubbard R, Smith C et al. Incidence and mortality of falls amongst older people in primary care in the United Kingdom. Quarterly J Med 2009;102:477–483.
[9] Han BH, Ferris R & Blaum C. Exploring ethnic and racial differences in falls among older adults. J Community Health. 2014. doi: 10.1007/s10900-014-9852-8.
[10] Salonen L & Kivela SL. Eye diseases and impaired vision as possible risk factors for recurrent falls in the aged: a systematic review. Current Gerontology and Geriatrics Research. 2012:271481.
[11] Lord SR, Dayhew J & Howland A. Multifocal glasses impair edge contrast sensitivity and depth perception and increase the risk of falls in older people.J Am Geriatr Soc 2002;50:1760–1766.
[12] Walther LE, Rogowski M, Schaaf H et al. Falls and dizziness in the elderly. Otolaryngologia Polska 2010;64:354–357.
[13] Carey BJ & Potter JF. Cardiovascular causes of falls. Age Ageing. 2001;30 Suppl 4:19–24.
[14] Freeman R, Wieling W, Axelrod FB et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clinical Autonomic Res. 2011;21:69–72.
[15] Hill KD & Wee R. Psychotropic drug-induced falls in older people: a review of interventions aimed at reducing the problem. Drugs Aging. 2012;29(1):15–30.
[16] Gribbin J, Hubbard R, Gladman JRF et al. Risk of falls associated with antihypertensive medication: population-based case–control study. Age Ageing. 2010;39:592–597.
[17] Oliver D, Healey F & Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med. 2010;26:645–692.
[18] Reilly T, Barile D & Reuben S. Role of the pharmacist on a general medicine acute care for the elderly unit. Am J Geriatr Pharmacother 2012;10:95–100.
[19] McCollum M, Nuffer W, Ellis SL et al. Physician acceptance of pharmacotherapy recommendations made by pharmacy students in a rural pharmacy-based diabetes care and education clinic. Am J Pharm Educ. 2009;73:24
You might also be interested in…
Pharmaceutical care – a model for elderly patients

Medicines shortages and slow approvals put ‘significant burden’ on pharmacists, says report
