Nicolle R Fuller / Science Photo Library
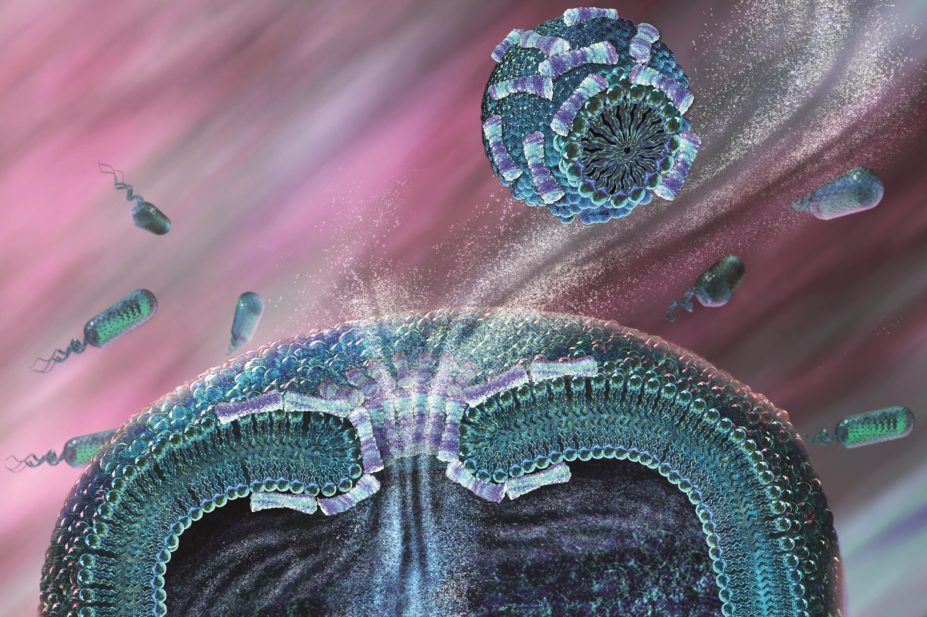
An antimicrobial agent is defined as a substance that inhibits the growth of microorganisms[1]
. Antimicrobial agents act by targeting specific sites in a wide range of organisms, including bacteria, viruses, fungal, protozoa and helminths; antibiotics are a subcategory of this large group and have the ability to kill or inhibit the growth of bacteria[1]
. Originally, antibiotics were substances produced by microorganisms that selectively inhibit the growth of another[1]
; however, many of these drugs are manufactured synthetically and achieve comparable outcomes.
Antimicrobial therapy was integrated into medicine in the 1930s, and these agents have made procedures such as arthroplasties and transplants possible[1]
,[2]
. With few new antibiotic agents currently in trials or development, the increase of antimicrobial resistance represents a major global health problem[3]
,[4]
,[5]
. Inappropriate use of antimicrobials and broad-spectrum antibiotics contributes to the selection pressure for the emergence of resistant pathogens[3]
,[6]
,[7]
.
The UK government has recognised that antimicrobial resistance is a significant health issue and in 2013 produced a five-year strategy to slow its development and spread[8]
.
Healthcare professionals should be aware of the basic principles of antimicrobial treatment[1]
and the need to reduce inappropriate prescribing of antibiotics in order to retain effectiveness of the drugs currently available[3]
,[4]
,[5]
,[6]
,[7]
,[8]
. This article mainly focuses on antibiotics, however, the principles relevant to this class of antimicrobial agent can be applied to others. The mode of action of antibiotics and resistance mechanisms, whether intrinsic or acquired, is outside the scope of this article and is covered elsewhere[9]
.
Misuse and overuse of antibiotics
Published studies from the UK and the United States estimate that around 30% of patients receive antibiotics while in hospital[10]
,[11]
,[12]
.
Since their introduction, antimicrobials have been misused and inappropriately prescribed, resulting in the selection of resistant organisms. Examples include[13]
:
- Prescribing antibiotics without clear evidence of bacterial infection;
- Prolonged empiric antimicrobial treatment without clear evidence of infection;
- Treatment of a positive culture in the absence of disease – patients can be colonised with an organism without having clinical symptoms of an infection (e.g. asymptomatic bacteriuria or identification of coagulase negative Staphylococci in blood cultures[14]
,[15]
); - Failure to de-escalate patients to a narrow spectrum agent once the causative organism has been identified. Often this does not occur as prescribers are resistant to change because the patient has improved on the current antibiotics;
- Prolonged prophylactic therapy, which is unnecessary and promotes the evolution of resistant organisms. However, prophylactic antibiotics are useful and recommended for certain procedures to prevent post-operative infections[16]
.
Judicious prescribing will reduce the selective pressure on bacteria and slow the emergence of resistance. Several national initiatives have been proposed to combat antimicrobial resistance and promote appropriate prescribing, which include:
- The dissemination of a recent national patient safety alert[17]
by NHS England, highlighting the challenge of antimicrobial resistance; - Guidance from the National Institute for Health and Care Excellence (NICE), England’s health technology assessment body[18]
; - Toolkits for primary care (TARGET; Treat Antibiotics Responsibly, Guidance, Education, Tools)[19]
and secondary care (Public Health England’s ‘Start smart – then focus’)[20]
.
For further information on national and international initiatives, please see ‘Box 1: National and international initiatives’.
Box 1: National and international initiatives
Antimicrobial resistance is a healthcare priority, which is being addressed both nationally and internationally through various routes. These include:
TARGET
Treat Antibiotics Responsibly, Guidance, Education, Tools (TARGET) is designed to be used by the whole primary care team within the GP practice or out-of-hours setting, but it is also relevant to mental healthcare settings. The toolkit aims to help influence prescribers’ and patients’ attitudes, beliefs and perceived barriers to optimal antibiotic prescribing[19]
.
‘Start smart – then focus’
An outline of evidence-based antimicrobial stewardship practice for use in secondary care settings, this guidance from Public Health England provides information on strategies to improve antibiotic use within secondary care, as well as suggested audits to improve practice[20]
.
English surveillance programme for antimicrobial utilisation and resistance
The 2015 English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) report[21]
highlighted that the majority of antibiotics in England (74%) are prescribed in general practice. Overall, the total consumption of antibiotics in England (measured as defined daily doses per 1,000 inhabitants per day) increased by 6.5% between 2011 and 2014. Prescribing by dentists decreased by 2.8% but general practice consumption increased by 6.2% and secondary care prescribing for inpatients increased by 11.7%. Essentially, antimicrobial use is rising, which leads to increased resistance, increased frequency of treatment failure, decreased treatment options available and increased costs. It is imperative that the guidance provided is used and antimicrobial stewardship activities are incorporated within healthcare sectors[22]
.
Antimicrobial stewardship
Stewardship is defined as the right antibiotic for the right patient, administered at the right time, at the right dose and via the right route, causing the least harm to the patient and future patients[23]
. The three major goals for antimicrobial stewardship are to optimise therapy for individual patients, prevent overuse, misuse and abuse of antimicrobials, and minimise the development of resistance at patient and community levels[24]
.
National Institute for Health and Care Excellence guidance
The aim of the National Institute for Health and Care Excellence guidance is to “change prescribing practice to help slow the emergence of antimicrobial resistance and ensure that antimicrobials remain an effective treatment for infection” by providing advice on the effective use of antimicrobials in children, young people and adults, not only for healthcare professionals but for commissioners, the social sector and the public. It is divided into four parts, covering: stewardship programmes, prescribing, the introduction of new antibiotics and suggestions on how to change prescribing practice[18]
.
World Health Organization resolution
In May 2014, the World Health Organization (WHO) passed a resolution that reflects global agreement on the huge threat that antimicrobial resistance poses to human health. Many countries have national action plans in place that follow the WHO strategy[25]
. The global action plan seeks to preserve and maintain responsible and accessible use of antimicrobials for all. The main strategic objectives focus on improving the understanding and awareness of antimicrobial resistance, strengthening knowledge via research and surveillance, reducing infection incidence, optimising the use of antimicrobial treatments and countering antimicrobial resistance through sustainable investment[25]
. The UK has a plan in place to slow the development and spread of antimicrobial resistance, which is supported by the ESPAUR[21]
,[25]
.
Empiric versus definitive therapy
Antimicrobial therapy should only be initiated when there is a strong suspicion of an infection[1]
. The patient’s presenting symptoms, as well as imaging and biochemical parameters, should be used to aid diagnosis[1]
,[26]
. Symptoms of infection often include fever, changes in respiratory rate and blood pressure, confusion and tachycardia. Laboratory and radiological tests are important considerations for the assessment of the patient in conjunction with clinical findings[1]
. It should be noted that radiological improvement frequently lags behind clinical improvement and a repeat chest X-ray is not always indicated[2]
. Biochemistry tests include measurement of C-reactive protein (CRP) to determine if inflammation is resolving, and monitoring of the patient’s temperature, white cell and neutrophil count to determine the response to treatment. These should be considered together with clinical symptoms[1]
,[2]
,[26]
.
Empiric therapy for infections can be described as ‘best guess’ therapy because no information is available regarding the causative organism and the likely antimicrobial susceptibility. It is not an exact science and can be better described in mathematical terms as the treatment of an infection with an agent, where there is a high probability that the causative organism is sensitive to that agent[1]
,[13]
,[26]
,[27]
and will depend on national as well as local resistance patterns. For most cases, treatment of an infection is empiric and the most likely microbiological etiology can be inferred from the clinical presentation[13]
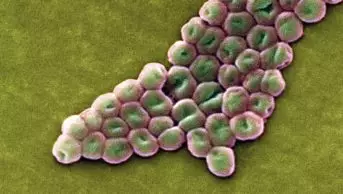
. For example, the common causative organisms in cellulitis are Streptococci and Staphylococci, and therefore appropriate antibiotics can be administered in the absence of a positive culture[28]
.
Clinical presentation acts a guide for most empiric treatment because microbiology test results are not usually available for 48–72 hours after initial therapy. Patients presenting with acute and increasingly severe infections require prompt treatment to decrease morbidity and mortality
[27]. Therapeutic treatment usually involves a broad-spectrum antibiotic (either as a single agent or combination of agents) against the most common likely causative bacteria; therapeutic inadequacies are associated with poor outcomes, including increased morbidity, mortality and increased length of inpatient hospital stay[13]
,[29]
.
Diagnosis should be supported by laboratory investigations, if possible, to establish the causative organism and its susceptibility to antimicrobial agents[27]
. When the organism responsible for the infection is known, targeted treatment with an agent the organism is susceptible to in vitro can commence (known as definitive therapy)[13]
. Focused therapy (i.e. de-escalating or escalating treatment)[13]
, can help reduce adverse drug reactions, optimise treatment, prevent the emergence of resistance and reduce costs[13]
.
The aim of treatment is to eradicate the infection efficiently and achieve good clinical outcomes (a clinical or bacteriologic cure and no relapse) with the least toxicity[27]
,[30]
.
Bactericidal versus bacteriostatic agents
Antimicrobial agents are often described as bactericidal or bacteriostatic[27]
,[30]
. Bacteriostatic agents prevent the growth of bacteria — that is, they are maintained in the stationary phase of growth (e.g. clindamycin, linezolid and tetracyclines), whereas bactericidal agents kill bacteria (e.g. beta-lactam agents, aminoglycosides and fluoroquinolones[30]
). However, this is overly simplistic; in reality, there are not two pure categories. The in vitro microbiological determination of whether an antibacterial agent is bactericidal or bacteriostatic may be influenced by growth conditions, bacterial density, test duration and the extent of reduction in bacterial numbers[30]
. Therefore, most antibacterials can be better described as being potentially both bactericidal and bacteriostatic. At high concentrations, bacteriostatic agents are often bactericidal against some susceptible organisms[30]
,[31]
. Macrolides are considered to be one of the classic bacteriostatic drug classes, but erythromycin, azithromycin and clarithromycin have shown bactericidal activity in vitro against Streptococcus
pyogenes and Streptococcus
pneumoniae
[32]
,[33]
,[34]
,[35]
. Similarly, chloramphenicol is bactericidal against S. pneumoniae but bacteriostatic against Staphylococcus aureus and group B Streptococcus
[36]
,[37]
,[38]
,[39]
. Clindamycin may be bactericidal in vitro, depending on the organism and growth conditions[40]
,[41]
. In vitro, linezolid has bacteriostatic activity against Staphylococci and Enterococci but bactericidal activity against Streptococci, including S. pneumoniae
[42]
,[43]
.
There are clinical conditions where a bactericidal agent is necessary. In endocarditis, for example, bacteria within cardiac vegetations can reach very high concentrations, and the rates of metabolism and cell division appear to be reduced, resulting in reduced susceptibility to bactericidal agents[30]
. Clinical cure is often achieved but this usually requires prolonged administration of relatively high doses of bactericidal agents. By contrast, studies have described the successful use of bacteriostatic agents for the treatment of infective endocarditis[30]
.
For the treatment of meningitis, it is important to choose a bactericidal agent that penetrates the cerebrospinal fluid to eradicate the infection as rapidly as possible (e.g. ceftriaxone)[44]
. Certain bacteriostatic agents have been used successfully to treat Gram-positive bacterial meningitis[30]
.
Osteomyelitis can be difficult to treat on account of decreased vascular supply and penetration of adequate concentrations of the drug in bone. For this reason, a bactericidal agent may seem a logical choice, however, clindamycin, a bacteriostatic agent, achieves high concentrations in bone and is considered an appropriate agent for the treatment of Gram-positive bacterial osteomyelitis[45]
,[46]
in combination with appropriate adjuvant therapy.
Pharmacokinetics and pharmacodynamics
The current definition of pharmacokinetics is the study of the time course of drug absorption, distribution, metabolism and excretion. Pharmacodynamics refers to the relationship between drug concentration at the site of action and the resulting effect, including the time course, and intensity of therapeutic and adverse effects[1]
,[13]
,[26]
,[27]
.
Certain antibiotics (e.g. beta-lactams and glycopeptides) can be described as time-dependent — the duration of time the drug concentration remains above the minimum inhibitory concentration (MIC) — while others (e.g. aminoglycosides amikacin and gentamicin) can be described as concentration-dependent — the ratio of the maximal drug concentration to the MIC and the ratio of the area under the concentration time curve at 24 hours to the MIC[26]
,[27]
,[30]
.
For antibiotics to be effective, there must be sufficient concentrations of the agent(s) at the site of the infection. This differs according to the type of infection and antibiotic administered. Concentrations of antibiotics rise and fall after administration, and frequency of administration of antibiotic is dependent on several drug and host factors.
Post-antibiotic effect can be defined as the continued inhibition of bacterial growth, beginning when the organisms are exposed to an antibiotic until the bacterial survivors begin to replicate again to a significant degree. Significant post-antibiotic effects are observed with aminoglycosides, macrolides and quinolones against Gram-negative bacteria[26]
,[27]
.
Selecting which antimicrobial agent to prescribe
The choice of agent, or agents, is dependent on many drug and host factors. Patient factors that need to be considered when selecting the most suitable treatment for an infection include[1]
,[13]
,[26]
,[27]
:
- Differential diagnosis/indication;
- The most likely organism(s) causing the infections;
- The patient’s allergy status;
- The severity and duration of the infection;
- Whether the patient is immunocompromised;
- The patient’s renal and hepatic function;
- Whether the patient has had previous antibiotic exposure;
- Genetic factors;
- Local epidemiology;
- Colonisation with resistant organisms;
- The patient’s age and gender;
- If the patient on any other concomitant medication;
- Whether the patient is pregnant or breastfeeding;
- The patient’s vaccination history;
- Whether the patient has been travelling;
- If the patient has any history of drug abuse;
- The presence of any risk factors.
Gathering information, including taking a detailed patient history[47]
, is necessary to ensure that the most suitable agent is prescribed[26]
,[27]
. Any previous microbiology results may inform the healthcare professional of whether the patient is infected with resistant organisms (e.g. methicillin– resistantS. aureus
[MRSA], vancomycin-resistant Enterococci [VRE], an extended spectrum beta-lactamase [ESBL]-producing organism or a carbapenemase-producing Enterobacteriaceae [CPE]). Together with the type of infection and working (until proven) diagnosis, this information should guide the healthcare professional as to which agent(s) to prescribe empirically.
Certain drugs should always be prescribed in combination (e.g. rifampicin and fusidic acid) because the use of these drugs individually can result in the emergence of resistant bacteria[1]
,[26]
. When agents exhibit synergistic activity against a microorganism, combination therapy is recommended to extend the antimicrobial spectrum beyond that achieved by the use of a single agent, especially in polymicrobial infections and to prevent the emergence of resistance[13]
. In patients without a penicillin allergy, combination therapy with a beta-lactam agent and an aminoglycoside is common as first-line treatment for certain infections (e.g. sepsis[48]
). For the management of community-acquired pneumonia, the severity of infection and, consequently, choice of agent is dictated by the CURB score in hospitals and CRB score in primary care[49]
. By contrast, the treatment of infective endocarditis requires treatment with high doses of a parenteral antibiotic for a longer duration than normal[50]
. It has also been demonstrated that for infective endocarditis, an aminoglycoside plus benzylpenicillin provides a synergistic response that is favourable, compared with when each drug is prescribed alone[50]
.
However, combination therapy of antimicrobials is not always beneficial and can be antagonistic in vitro. For example, a study by Lepper et al. showed worse clinical outcomes when a penicillin and tetracycline were prescribed in combination compared with either drug being prescribed alone[26]
,[51]
.
Prescribing in special groups
The pharmacokinetics of antimicrobial agents are different in the following groups and, therefore, pose an increased risk of drug toxicity[8]
:
- Paediatric patients;
- Older patients;
- Patients with low/increased body weight;
- Patients with renal/hepatic insufficiency;
- Patients with allergy.
These factors contribute to the decision-making process when determining choice, dose, route, formulation and frequency of drug.
The pharmacokinetics and pharmacodynamics in premature infants, neonates and paediatrics differ to adults because of their relatively immature systems. This again differs in older patients because of multiple comorbidities and age-related renal insufficiency[26]
,[27]
. The use of antibiotics in pregnancy is warranted when the benefits outweigh the risks. Since some antibiotics have a greater potential to pass through the placenta to foetal tissues, antibiotic prescribing in pregnancy should be restricted unless necessary, especially during the first trimester when organogenesis is maximal[27]
. Antibiotics also have the potential to be excreted into breast milk. For most, the concentrations are too small to have an adverse effect on the baby; however, certain drugs (e.g. metronidazole, tetracyclines and erythromycin) are readily excreted into breast milk and are contraindicated[52]
.
Obesity plays a major factor in the dosing of antibiotic agents, affecting both the clearance and volume of distribution of the agent[53]
. Antibiotics can also be described as being hydrophilic (e.g. beta-lactams, glycopeptides and aminoglycosides) or lipophilic (e.g. fluoroquinolones, quinolones and clindamycin). Hydrophilic drugs mainly distribute in the extracellular fluid (not fat), whereas lipophilic drugs distribute into fat[27]
. It can be complicated to calcuate the correct dose for obese patients[27]
because around 30% of adipose tissue is water; therefore, total body weight overestimates renal function in these patients, while the use of ideal body weight underestimates renal function[53]
. Furthermore, obese patients are generally underrepresented in clinical trials and, therefore, data on appropriate dosing and effectiveness are limited in this patient group[54]
,[55]
. Specific advice should be sought from an antimicrobial pharmacist, consultant microbiologist, infectious diseases physician or medicines information department before commencing treatment in obese patients.
Many antibiotics are either renally or hepatically cleared, which poses a problem in patients with renal or hepatic impairments. Dose reduction should be exercised in patients with renal insufficiency[13]
,[27]
. However, for drugs that have a narrow therapeutic index, treatment should be adjusted according to clinical response and serum drug concentrations. For patients with liver disease, hepatically metabolised antibiotics should be used with caution and the dose adjusted if necessary according to the patient’s liver function tests (LFTs). LFTs should be monitored throughout the duration of treatment to ensure the antibiotics are not damaging the patient’s liver.
Route of administration
Antibiotics are administered via a number of routes (e.g. topically, orally, intravenously, intramuscularly, intraperitoneally or nebulised). The bioavailability (the amount of active drug that reaches systemic circulation) of oral formulations varies: some have excellent bioavailability (e.g. the fluoroquinolones[56]
,[57]
,[58]
), while others have little-to-no absorption (e.g. the glycopeptides[59]
). Other antibiotics lie somewhere in between and for some agents their bioavailability is affected by the presence of food, iron or calcium products[60]
. In increasingly severe infections, intravenous preparations are the preferred choice to achieve optimal drug concentrations.
Intravenous to oral switch
Not all patients who are admitted to secondary care because of the severity of their illness are initiated on parenteral antibiotics. Some patients admitted for other reasons (e.g. dehydration, pain control or with no gastro-intestinal dysfunction) are prescribed and administered antibiotics with good oral bioavailability, such as fluoroquinolones[1]
. Patients prescribed intravenous antibiotics should be reviewed after 48 hours and switched to an oral equivalent if they are clinically improving (i.e. they are haemodynamically stable, apyrexial and CRP, white cell and neutrophil count trending towards normal[58]
). Patients should be able to swallow, tolerate oral fluids and a suitable oral agent or equivalent should be available. Prescribing or switching to oral agents has a number of advantages: it facilitates the removal of any in-dwelling catheters/venflons, treatment costs are decreased, there are fewer adverse drug reactions, the patient may be discharged earlier from hospital and they are consequently less likely to develop hospital-acquired infections[58]
,[61]
,[62]
. For some infections (e.g. osteomyelitis, infective endocarditis, line infections and deep seated infections), an oral switch is not recommended[50]
,[63]
.
Duration of therapy
The duration of treatment is controversial because there are few published studies regarding this and many of the recommendations are based on expert opinion[13]
,[44]
,[45],
[46],
[50]
. The optimal duration of therapy is one that is short enough to treat the infection without the peripheral effects (e.g. adverse drug reactions and resistance[1]
). Treatment should continue for as long as necessary until all microorganisms are eliminated, or the infection has been sufficiently controlled for the host defenses to eradicate it. Cessation of antibiotics should be supported by clinical, microbiological and biochemistry parameters[1]
,[13]
,[26]
,[27]
,[64]
. Most infections require treatment of between five and seven days and, depending on the patient’s response and difficult-to-treat infections, an extended course may be required to achieve microbiological eradication[65]
. There are exemptions that warrant long-term treatment (e.g. endocarditis, osteomyelitis and Mycobacterium tuberculosis) to prevent recurrence or worsening of the infection[27]
,[50]
,[66]
, or short-term treatment (e.g. uncomplicated urinary tract infection in females) when a three-day course of antibiotics is sufficient[67]
.
Therapeutic drug monitoring
Serum concentration should be monitored for drugs with a narrow therapeutic index to ensure treatment failure does not occur because of low levels, or toxicity does not occur because of high levels[1]
,[13]
,[26]
,[27]
. Most antimicrobial agents have a wide therapeutic index and, therefore, in most scenarios, standard doses can be used[1]
. Vancomycin and aminoglycosides are common antibiotics that have a narrow therapeutic window and, therefore, therapeutic drug monitoring is indicated[68]
,[69]
,[70]
.
Adverse drug reactions
Obtaining a history and assessing the patient may prevent inadvertent administration of an agent that the patient may react to[1]
,[71]
. All drugs have the potential to cause an adverse drug reaction[72]
but not all patients experience them. Around one in five patients experience very minor intolerant reactions (e.g. gastrointestinal disturbances), while others may develop a rash, urticaria, laryngeal oedema, bronchospasm or hypotension[71]
. The beta-lactams are recognised as one of the most frequent causes of adverse drug reactions[71]
. The symptoms that a patient experiences should be managed according to the nature and severity of the reaction. Healthcare professionals involved in prescribing, screening and administering an antibiotic should be aware that the risk of a patient experiencing an adverse drug reaction increases with the number of antibiotic prescriptions[73]
,[74]
.
Failure to respond
Patients do not always respond to antibiotic therapy; there are a number of reasons why this may occur[1]
,[13]
,[26]
,[27]
,[75]
,[76]
,[77]
:
- Source control/adjuvant therapy is required, persistent bacteraemia is often an indication that source control is required before the infection can be completely resolved.
- Source control encompasses a spectrum of interventions with the objective of the physical control of the foci of infection and the restoration of optimal function and quality of life. Source-control measures can be categorised as surgical drainage, debridement (i.e. the physical removal of solid necrotic tissue), device removal or more definitive measures to restore optimal function to the involved area[78],
[79]
;
- Source control encompasses a spectrum of interventions with the objective of the physical control of the foci of infection and the restoration of optimal function and quality of life. Source-control measures can be categorised as surgical drainage, debridement (i.e. the physical removal of solid necrotic tissue), device removal or more definitive measures to restore optimal function to the involved area[78],
- Incorrect choice of antibiotic(s);
- Wrong dose or poor penetration – pharmacokinetic and pharmacodynamic properties.
- A report that a pathogen is susceptible to an antibiotic in the laboratory does not assure treatment success. Inadequate penetration of the infection site is one of the principal factors related to failure of antibacterial therapy[30]
. The active drug needs to reach the bacteria in appropriate body fluids and tissues at concentrations necessary to kill or suppress the pathogen’s growth. The ability of antibacterial agents to cross the blood–brain barrier is an important consideration for the treatment of meningitis;
- A report that a pathogen is susceptible to an antibiotic in the laboratory does not assure treatment success. Inadequate penetration of the infection site is one of the principal factors related to failure of antibacterial therapy[30]
- Causative bacteria becoming resistant to the current agents prescribed;
- Etiology may not be infective;
- Poor compliance (oral prescription);
- Impaired host defense mechanisms;
- Site of infection;
- Underlying disease.
Antimicrobial prophylaxis
The prophylactic use of antibiotics is necessary in some scenarios to prevent or reduce the risk of an infection post-operatively. Some procedures are associated with a high infection rate, for example surgical interventions involving the implantation of a prosthetic material[16]
. The antibiotic(s) prescribed should be effective against the bacteria most likely to cause infection, the antibiotics should be present in the tissues when the initial incision is made and adequate serum concentrations should be maintained during the procedure. Duration of prophylaxis for surgical site infection should not exceed 24 hours in most cases[16]
,[80]
.
Cost of treatment
Selection of the most suitable antimicrobial agent and cost are important considerations when developing empiric guidelines. Acquisition costs for parenteral antibiotics are generally greater than oral formulations[1]
. However, the biggest economic burden is attributed to inpatient hospital stay[1]
. Administration of parenteral antibiotics includes additional costs (e.g. fluids for reconstitution and administration, as well as nursing and administration time). There is also an ecologic impact of the use of these agents on resistant pathogens and several antibiotic stewardship activities are underway to minimise the inappropriate use of these agents, as well as to slow down the rate of resistance[1]
.
Guideline development
In addition to costs, empiric guidelines consider the most likely organism(s) causing the infection, national and local resistant patterns, and patient factors when contemplating choice of drugs. Guidelines should have first-line, second-line and third-line recommendations for empiric treatment of common infections. First-line agents are recommendations for patients with no known allergies. Second-line agents are recommendations for patients who do not have an anaphylactic reaction to penicillin or related agents, and third-line agents are recommendations for patients who have a type 1 reaction to penicillin or related agents[81]
.
Shilpa Jethwa is a specialist pharmacist (antibiotics) at Northwick Park Hospital, London North West Healthcare NHS Trust. Correspndence to:
shilpa.jethwa@nhs.net
Financial and conflicts of interest disclosure:
The author has received fees for an advisory board meeting from MSD. The author has no other relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilised in the production of this manuscript.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Vol 1. 8th ed. Vol : 224–234. Section E: anti-infective therapy: principles of anti-infective therapy. Churchill Livingstone/Elsevier: 2014.
[2] Bruns AH, Oosterheert JJ, El Moussaoui R et al. Pneumonia recovery: discrepancies in perspectives of the radiologist, physician and patient. J Gen Intern Med. 2010;25(3):203–206. doi: 10.1007/s11606-009-1182-7
[3] Gelband H, Miller-Petrie M, Pant S et al. The state of the worlds antibiotics 2015, Center for disease, dynamics, economics and policy 2015. Available at: http://www.cddep.org/publications/state_worlds_antibiotics_2015#sthash.Or1KL7qq.dpbs (accessed August 2016).
[4] Antimicrobial resistance. Global report on surveillance. WHO 2014. Available at: http://www.who.int/drugresistance/documents/surveillancereport/en/ (accessed August 2016).
[5] Jethwa S. Tackling antimicrobial resistance through education. Prescriber 2015;26:35–36. doi: 10.1002/psb.1351
[6] Review on antimicrobial resistance. Tackling drug resistant infections globally: final report and recommendations. 19 May 2016. Chaired by Jim O’Neill. Available at: http://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf (accessed July 2016).
[7] Rice LB. The clinical consequences of antimicrobial resistance. Curr Opin Microbiol 2009; 12:476–481. doi: 10.1016/j.mib.2009.08.001
[8] Department of Health. UK Five Year Antimicrobial Resistance. Strategy 2013 to 2018. September 2013. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/244058/20130902_UK_5_year_AMR_strategy.pdf%20 (accessed July 2016).
[9] Rang and Dale’s Pharmacology, 8th edition. 2015.
[10] Hoffman JM, Shah ND & Vermuelen LC. Projecting future drug expenditures. Am J Health Syst Pharm 2007;64:298–314. doi: 10.2146/ajhp060545
[11] Wise R, Hart T, Cars O et al. Antimicrobial resistance is a major threat to public health. The BMJ 1998;317:609–610. doi: 10.1136/bmj.317.7159.609
[12] John JF & Fishman NO. Programmatic role of the infectious diseases physician in controlling antimicrobial costs in the hospital. CID 1997;24:471–485. doi: 10.1093/clinids/24.3.471
[13] Leekha S, Terrell CL & Edson RS. General Principles of Antimicrobial Therapy. Mayo Clinic Proceedings 2011;86(2):156–167. doi: 10.4065/mcp.2010.0639
[14] Silver SA, Baillie L & Simor AE. Positive urine cultures: A major cause of inappropriate antimicrobial use in hospitals? Can J Infect Dis Medl microbiol. 2009;20(4):107–111. doi: 10.1155/2009/702545
[15] Becker K, Heilmann C & Peters G. Coagulase-Negative Staphylococci. Clin Microbiol Rev 2014;27(4):870–926. doi: 10.1128/CMR.00109-13
[16] Healthcare improvement Scotland. SIGN 104. Antibiotic prophylaxis in surgery. July 2008, updated April 2014. Available at: http://www.sign.ac.uk/pdf/sign104.pdf%20 (accessed August 2016).
[17] Public Health England. Patient safety alert. Addressing antimicrobial resistance through implementation of an antimicrobial stewardship programme. August 2015. NHS/PSA/Re/2015/007 Available at: https://www.england.nhs.uk/wp-content/uploads/2015/08/psa-amr-stewardship-prog.pdf (accessed August 2016).
[18] National Institute for Health and Care Excellence. Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use NG15. 2015. Available at: http://www.nice.org.uk/guidance/ng15%20 (accessed August 2016).
[19] TARGET Antibiotic toolkit. 2012. Available at: http://www.rcgp.org.uk/targetantibiotics/ (accessed August 2016).
[20] Start smart — then focus. Antimicrobial Stewardship Toolkit for English Hospitals. 2015. Available at: https://www.gov.uk/government/publications/antimicrobial-stewardship-start-smart-then-focus (accessed August 2016).
[21] Public Health England. English surveillance programme antimicrobial utilization and resistance (ESPAUR) 2010 to 2014. November 2015. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/362374/ESPAUR_Report_2014__3_.pdf (accessed August 2016).
[22] The Health and Social Care Act 2008: Code of Practice on the prevention and control of infections and related guidance (2008, updated 2015). Available at: https://www.gov.uk/government/publications/the-health-and-social-care-act-2008-code-of-practice-on-the-prevention-and-control-of-infections-and-related-guidance (accessed August 2016).
[23] Nathwani D & Sneddon J. Practical guide to antimicrobial stewardship in hospitals. 2013.
[24] Doron S & Davidson LE. Antimicrobial stewardship. Mayo Clin Proc 2011;86(11):1113–1123. doi: 10.4065/mcp.2011.0358
[25] Sadak M, Cramp E & Ashiru-Oredope D. Antimicrobial Resistance and Stewardship in National Action Plans. Current Treatment Options in Infectious Diseases. 2016;8(2):57–71. doi: 10.1007/s40506-016-0078-4
[26] Greenwood D, editor. Antimicrobial Chemotherapy 4th edition, part IV general principles of usage of antimicrobial agents. Oxford University Press: 2000.
[27] Davey P, Wilcox M, Irving W et al. Antimicrobial Chemotherapy. 7th edition. 2015.
[28] Clinical resource efficiency support team. Guidelines on the management of cellulitis in adults. CREST June 2005. Available at: http://www.acutemed.co.uk/docs/Cellulitis%20guidelines,%20CREST,%2005.pdf (accessed August 2016).
[29] Tunkel AR, Hartman BJ, Kaplan SL et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004;39(9):1267–1284. doi: 10.1086/425368
[30] Pankey GA & Sabath LD. Clinical relevance of bacteriostatic versus bactericidal mechanisms of action in the treatment of Gram positive bacterial infections. Clin Infect Dis 2004;38(6):864–870. doi: 10.1086/381972
[31] Reese RE & Betts RF. Antibiotic use. In: Reese RE, Betts RF, eds. A practical approach to infectious diseases. 3rd ed. Boston: Little, Brown, and Company. 1991:821–1007.
[32] Fernandes PB, Bailer R, Swanson R et al. In vitro and in vivo evaluation of A-56268 (TE-031), a new macrolide. Antimicrob Agents Chemother 1986;30:865–873. doi: 10.1128/AAC.30.6.865
[33] Haight TH & Finland M. Observations on mode of action of erythromycin. Proc Soc Exper Biol Med 1952;81:188–193. doi: 10.3181/00379727-81-19817
[34] Piscitelli SC, Danziger LH & Rodvold KA. Clarithromycin and azithromycin: new macrolide antibiotics. Clin Pharm 1992;11:137–152.
[35] Retsema J, Girard A, Schelkly Wet al. Spectrum and mode of action of azithromycin (CP-62,993), a new 15-membered-ring macrolide with improved potency against gram-negative organisms. Antimicrob Agents Chemother 1987;31:1939–1947. doi: 10.1128/AAC.31.12.1939
[36] Feder HM Jr, Osier C & Maderazo EG. Chloramphenicol: a review of its use in clinical practice. Rev Infect Dis 1981;3:479–491. doi: 10.1093/clinids/3.3.479
[37] Rahal JJ Jr & Simberkoff MS. Bactericidal and bacteriostatic action of chloramphenicol against meningeal pathogens. Antimicrob Agents Chemother 1979;16:13–18. doi: 10.1128/AAC.16.1.13
[38] Turk DC. A comparison of chloramphenicol and ampicillin as bactericidal agents for Haemophilus influenzae type B. J Med Microbiol 1977;10:127–131. doi: 10.1099/00222615-10-1-127
[39] Weeks JL, Mason EO Jr & Baker CJ. Antagonism of ampicillin and chloramphenicol against meningeal isolates of group B streptococci. Antimicrob Agents Chemother 1981;20:281–285. doi: 10.1128/AAC.20.3.281
[40] Nastro LJ & Finegold SM. Bactericidal activity of ï¬ve antibacterial agents against Bacteroides fragilis. J Infect Dis 1972;126:104–107. doi: 10.1093/infdis/126.1.104
[41] Sande MA & Johnson ML. Antibacterial therapy of experimental endocarditis caused by Staphylococcus aureus. J Infect Dis 1975;131:367–375. doi: 10.1093/infdis/131.4.367
[42] Bostic GD, Perri MB, Thal LA et al. Comparative in vitro bactericidal activity of oxazolidone antibiotics against multidrug-resistant enterococci. Diagn Microbiol Infect Dis 1998;30:109–112. doi: 10.1016/S0732-8893(97)00210-1
[43] Zurenko GE, Yagi BH, Schaadt RD et al. In vitro activities of U100592 and U-100766, novel oxazolidinone antibacterial agents. Antimicrob Agents Chemother 1996;40:839–845. PMCID: PMC163216
[44] Nau R, Sörgel F & Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood–brain barrier for treatment of central nervous system infections. Clin Microbiol Rev 2010;23(4):858–883. doi: 10.1128/CMR.00007-10
[45] Chapman SW & Lin AC. Osteomyelitis and diabetic foot infections. In: Reese RE, Betts RF, eds. A practical approach to infectious diseases. 3rd ed. Boston: Little, Brown, and Company, 1991:464–498.
[46] Mader JT, Landon GC & Calhoun J. Antimicrobial treatment of osteomyelitis. Clin Orthop 1993;295:87–95. doi: 10.1097/00003086-199310000-00013
[47] Nickless G & Davies R. How to take an accurate and detailed medication history. The Pharmaceutical Journal February 2016. Available at:http://www.pharmaceutical-journal.com/learning/learning-article/how-to-take-an-accurate-and-detailed-medication-history/20200476.article (accessed August 2016).
[48] NHS England. International guidelines for the management of severe sepsis and septic shock: 2012. Surviving sepsis campaign. Available at: https://www.england.nhs.uk/2014/09/02/psa-sepsis/ (accessed August 2016).
[49] Lim WS, Baudouin SV, George RC et al. BTS guidelines for the management of community-acquired pneumonia in adults: update 2009. Thorax 2009;64:iii1-iii55. doi: 10.1136/thx.2009.121434
[50] Gould FK, Denning DW, Elliott TSJ et al. Guidelines for the diagnosis and antibiotic treatment of endocarditis in adults: a report of the working party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2012;67(2):269–289. doi: 10.1093/jac/dkr450
[51] Lepper MH & Dowling HF. Treatment of pneumococcic meningitis with penicillin compared with penicillin plus aureomycin: studies including observations on an apparent antagonism between penicillin and aureomycin. Arch Intern Med 1951;88:489–494. doi: 10.1001/archinte.1951.03810100073006
[52] Briggs G & Freeman R. Drugs in pregnancy and lactation. Wolters Kluwer Health. 10th edition 2015.
[53] Al-Dorzi HM, Al Harbi SA & Arabi YM. Antibiotic therapy of pneumonia in the obese patient: dosing and delivery. Curr Opin Infect Dis 2013;27(2):165–173. doi: 10.1097/QCO.0000000000000045
[54] Falagas ME & Karageorgopoulos DE. Adjustment of dosing of antimicrobial agents for bodyweight in adults. The Lancet 2010;375:248–251. doi: 10.1016/S0140-6736(09)60743-1
[55] Janson B & Thursky K. Dosing of antibiotics in obesity. Curr Opin Infect Dis 2012;25(6):634–649. doi: 10.1097/QCO.0b013e328359a4c1
[56] Cunha BA. Oral antibiotic therapy of serious systemic infections. Medical Clinics 2006:(90)6:1197–1222. doi: 10.1016/j.mcna.2006.07.009
[57] Höffken G, Lode H, Prinzing C et al. Pharmacokinetics of ciprofloxacin after oral and parenteral administration. Antimicrob Agents Chemother 1985;27(3):375–379. doi: 10.1128/AAC.27.3.375
[58] Cyriac JM & James E. Switch over from intravenous to oral therapy: a concise overview. J Pharmacol Pharmacother 2014;5(2):83–87. doi: 10.4103/0976-500X.130042
[59] Van Bambeke F. Glycopeptides and glycodepsipeptides in clinical development: a comparative review of their antibacterial spectrum, pharmacokinetics and clinical efficacy. Curr Opin Investig Drugs 2006;7(8):740–749. PMID: 16955686
[60] Winstanley PA & Orme ML. The effects of food on drug bioavailability. Br J Clin Pharmacol. 1989;28(6):621–628. doi: 10.1111/j.1365-2125.1989.tb03554.x
[61] Amodio-Groton M, Madu A, Madu CN et al. Sequential parenteral and oral ciprofloxacin regimen versus parenteral therapy for bacteremia: a pharmacoeconomic analysis. Ann Pharmacother. 1996;30(6):596–602. PMID: 8792944
[62] Oosterheert JJ, Bonten MJM, Buskens E et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicenter randomized trial. The BMJ 2006;333:1193. doi: 10.1136/bmj.38993.560984.BE
[63] Baddour LM, Wilson WR, Bayer AS et al. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association. Circulation 2005;111(23):e394–e434. doi: 10.1161/CIRCULATIONAHA.105.165564
[64] Ferguson J. Antibiotic prescribing: how can emergence of antibiotic resistance be delayed? Austrian prescriber April 2004:27:39–42.
[65] Chastre J, Wolff M, Fagon JY et al. PneumA Trial Group. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA 2003;290(19):2588–2598. doi: 10.1001/jama.290.19.2588
[66] Paul J. What is the optimal duration of antibiotic therapy? The BMJ 2006;332:1358. doi: 10.1136/bmj.332.7554.1358
[67] Milo G, Katchman EA, Paul Met al. Duration of antibacterial treatment for uncomplicated urinary tract infection in women. Cochrane Database Syst Rev. 2005;(2):CD004682. doi: 10.1002/14651858.CD004682.pub2
[68] Barclay ML & Begg EJ. Aminoglycoside toxicity and relation to dose regimen. Adverse Drug React Toxicol Rev 1994;13(4):207–234. PMID: 7734640
[69] Howden BP, Ward PB, Charles PG et al. Treatment outcomes for serious infections caused by methicillin-resistant Staphylococcus aureus with reduced vancomycin susceptibility. Clin Infect Dis 2004;38(4):521–528. doi: 10.1086/381202
[70] Rybak M, Lomaestro B, Rotschafer JC et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm 2009;66(1):82–98. doi: 10.2146/ajhp080434
[71] Jethwa S. Penicillin allergy management. The Pharmaceutical Journal Sept 2015:185-187. Available at: http://www.pharmaceutical-journal.com/learning/learning-article/penicillin-allergy-identification-and-management/20069170.article (accessed August 2016).
[72] Lyons T & Powrie K. Is this rash caused by my medicine? The Pharmaceutical Journal 2013:1–3. Available at: http://www.pharmaceutical-journal.com/learning/learning-article/is-this-rash-caused-by-my-medicine/11118364.article (accessed August 2016).
[73] Madaan A & Li JT. Cephalosporin allergy. Immunol Allergy Clin North Am 2004;24(3):463–476. doi: 10.1016/j.iac.2004.03.009
[74] Ulman K. AANP: certain cephalosporins may be safe for patients with penicillin allergies. Modern medicine 2007. Available at: http://www.medpagetoday.com/meetingcoverage/aanp/6016 (accessed August 2016).
[75] Estes L. Review of pharmacokinetics and pharmacodynamics of antibacterial agents. Mayo Clin Proc 1998;73:1114–1122. doi: 10.4065/73.11.1114
[76] Vogelman B & Craig WA. Kinetics of antibacterial activity. J Pediatr 1986;108:835–840. doi: 10.1016/S0022-3476(86)80754-5
[77] Craig W. Pharmacodynamics of antibacterial agents as a basis for determining dosage regimens. Eur J Clin Microbiol Infect Dis 1993;12(1):S6–8. doi: 10.1007/BF02389870
[78] Marshall JC & al Naqbi A. Principles of source control in the management of sepsis. Crit Care Clin. 2009;25(4):753–768, viii-ix. doi: 10.1016/j.ccc.2009.08.001
[79] Levinson AT, Casserly BP & Levy MM. Reducing mortality in severe sepsis and septic shock. Semin Respir Crit Care Med 2011;32(2):195–205. doi: 10.1055/s-0031-1275532
[80] Bratzler DW & Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis. 2004;38(12):1706–1715. doi: 10.1086/421095
[81] World Health Organization. Step-by-step approach for development and implementation of hospital antibiotic policy and standard treatment guidelines. Available at: http://apps.who.int/medicinedocs/documents/s19184en/s19184en.pdf%20 (accessed July 2016).