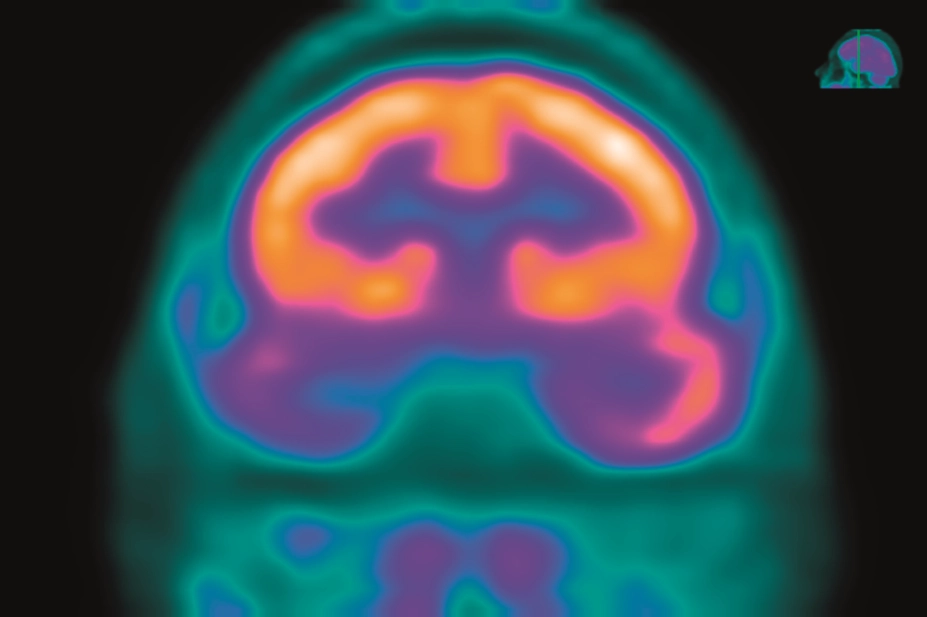
Centre Jean Perrin, ISM / Science Photo Library
Epilepsy is a neurological disorder marked by sudden recurrent episodes of sensory disturbance, loss of consciousness or convulsions, associated with neurones exhibiting abnormally high electrical excitability in the brain. It is a chronic debilitating condition affecting 50 million people worldwide[1]
and around 1% of people in the UK[2]
.
The occurrence of a single seizure does not constitute a diagnosis of epilepsy (see Box 1)[3]
and there is a variety of reasons why individuals may experience a seizure, including genetic mutations, cerebrovascular lesions or trauma, and identifiable organic causes (for more information, see Box 2), but for many the cause is undetermined.
Two-thirds of patients can be successfully treated using pharmacotherapy; however, the remaining third of patients fail to respond adequately to drugs and are designated medically refractory, also known as having chronic, intractable or pharmaco(drug)-resistant epilepsy[4],[5]
.
Refractory epilepsy is defined by the International League Against Epilepsy (ILAE) as “failure of adequate trials of two tolerated, appropriately chosen and used anti-epileptic drug schedules to achieve sustained seizure freedom, defined as less than one seizure per year” (for more information, see Box 1)[5]
. The management of patients with refractory epilepsy should be undertaken by a specialist centre with access to medical, surgical, psychological, social and other support services[6]
,[7]
.
The likelihood of people with refractory epilepsy achieving a seizure-free state with pharmacotherapy is dependent on the number of previous failures; it is less than 5% for more than six previously failed anti-epileptic drug trials[8],[9]
. A high proportion of these patients have focal epilepsy or learning disabilities, and seizure burden may be high, with a frequency of more than once a month in a third of these patients and numerous times a day in the worst cases, often in patients also affected by learning disabilities[7],[10]
.
Box 1: International League Against Epilepsy definitions of epilepsy
- Seizure: a transient occurrence of signs and/or symptoms owing to abnormal excessive or synchronous neuronal activity in the brain;
- Epilepsy: a disorder of the brain characterised by any of the following conditions:
- At least two unprovoked (or reflex) seizures occurring more than 24 hours apart;
- One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next ten years;
- Diagnosis of an epilepsy syndrome;
- Reflex epilepsy: predisposition for seizures triggered by photic, auditory or tactile stimuli;
- Drug-resistant epilepsy: failure of adequate trials of two tolerated, appropriately chosen and used anti-epileptic drug schedules (whether as monotherapy or in combination) to achieve sustained seizure freedom;
- Seizure freedom: 12 months without the occurrence of a seizure;
- Therapeutic effect: three times the longest previous inter-seizure interval;
- Resolved epilepsy: seizure freedom for ten years, at least the past five years of which without anti-seizure medication, or passed the age of an age-dependent epilepsy syndrome.
Source: Fisher RS, Acevedo C, Arzimanoglou A et al. ILAE Official Report: a practical clinical definition of epilepsy. Epilepsia 2014;55:475–482. doi: 10.1111/epi.12550
Types of epilepsy and epilepsy syndromes
Epilepsy can broadly be divided into generalised or focal. A third category, focal to bilateral tonic-clonic[3]
, occurs when an abnormal focal electrical discharge crosses the mid-line of the brain to involve the opposite cerebral hemisphere. Generalised seizures can be subdivided into tonic-clonic, absence, tonic, atonic, clonic or myoclonic (see Box 3).
Focal epilepsy can be subdivided according to whether awareness is lost or retained. It most commonly manifests as motor seizures, but can also manifest as sensory, psychic and even autonomic symptoms (see Box 3). Focal epilepsy is more likely to be refractory to drug therapy, with a prevalence of 35% compared with 20% of generalised epilepsies[7]
.
The most common focal type is temporal lobe epilepsy (TLE), in which there is altered perception and a clouding of consciousness, often with a strong emotional component, such as fear, irritability or aggression. In cases that are associated with hippocampal sclerosis, patients often respond better to surgical intervention than to drug therapy[11],[12]
.
Box 2: Potential causes of seizures that may be responsible for their suboptimal treatment
- Cerebrovascular lesions: stroke, hypoxia or cortical vein thrombosis;
- Drug-related: alcohol, recreational drugs, quinolones, tramadol;
- Space-occupying lesions: brain tumours, haemangioma, cerebral abscess;
- Trauma: head injury, traumatic birth, cerebral palsy;
- Infection/inflammation: meningitis, encephalitis, neurocysticercosis, malaria, autoimmune encephalitis;
- Organic: Bright’s disease (nephritis), phenylketonuria metabolic disturbance, hypoglycaemia, eclampsia.
Epilepsy syndromes comprise clusters of signs and symptoms occurring together that, depending on the type, may either resolve or evolve over time. Many have genetic links[11]
and learning disability is a common comorbidity.
West syndrome is a form of encephalopathy presenting within the first year of life where infantile spasms contribute to intellectual impairment. Early treatment with vigabatrin and hormonal therapy (oral prednisolone or tetracosactide depot)[6],[13]
can reduce the risk of progression to Lennox–Gastaut syndrome (LGS). It is important to note that vigabatrin can be associated with irreversible visual field defects; therefore, most centres restrict its use to this one condition. LGS involves multiple daily seizures, intellectual impairment and behavioural disorders and, being particularly refractory to treatment, carries a poor prognosis. The National Institute for Health and Care Excellence (NICE), England’s healthcare assessment body, recommends sodium valproate or lamotrigine for LGS, followed by rufinamide or topiramate if first-line therapy fails[6]
(see later cautions on valproate use).
Dravet syndrome is a severe genetic form of epilepsy presenting as febrile seizures in the first year of life. There is a misconception that this is triggered by childhood vaccinations, however, this association is coincidental. The underlying defect is a sodium channel gene mutation that results in myoclonic or focal epilepsy, intellectual disability and ataxia[14]
. The mainstay of treatment is a combination of sodium valproate, clobazam and stiripentol. However, patients may find this combination difficult to tolerate owing to excessive drowsiness, and stiripentol may cause behavioural problems.
This and other forms of myoclonic epilepsy, such as juvenile myoclonic epilepsy, may be exacerbated by drugs that act on voltage-gated sodium channels (e.g. carbamazepine), which should be avoided. NICE recommends sodium valproate as the drug of choice, with levetiracetam or topiramate as alternatives, or as adjunctive therapy[6]
.
Reasons for suboptimal treatment of seizures
Before a diagnosis of refractory epilepsy can be made, it is necessary to rule out treatable underlying causes (see Box 2), and differential diagnoses, such as cardiac syncope, migraine, cerebral ischaemia or psychogenic non-epileptic (dissociative) seizures[10],[15],[16]
. Diagnosis of the latter requires video-telemetry; this is because the symptoms can be difficult to reliably distinguish from epilepsy, as non-epileptic seizures also involve uncontrolled motor activity of all four limbs, often with prominent pelvic movements or back-arching[17]
.
The next step is to consider whether an appropriate first-line drug has been chosen, or a sub-therapeutic dosage[18]
. Carbamazepine, for instance, induces its own enzymatic metabolism such that the dosage must be adjusted during the first few months to achieve the same effect. The possibility of poor adherence to treatment should also be explored. It is important to involve the patient and family if appropriate in the decision-making process, providing adequate information on likely benefits and side effects to facilitate adherence[11]
.
Box 3: Types of epilepsy
Generalised
- Tonic-clonic: rigidity, muscle contraction and relaxation;
- Absence: brief vacant episodes, automatisms;
- Tonic: rigidity, fall backwards;
- Atonic: sudden loss of muscle tone, fall forwards;
- Clonic: muscle contraction-relaxation;
- Myoclonic: abrupt short, sharp muscle jerks.
Focal
- Temporal lobe: altered perception, clouding of consciousness, fear, irritability, automatisms;
- Frontal: personality changes, behavioural changes, hypermotor movements, posturing;
- Sensory: numbness, tingling, visual/auditory hallucinations;
- Psychic: nonsense speech, inability to think clearly.
A literature review by Laxer et al. suggests that refractory epilepsy is more likely to occur in those with a high frequency of seizures or neurological deficit at disease onset, or with a structural cause[18]
. Several hypotheses have been proposed, involving pathological changes of neurons, glia, receptors or transporter proteins[8]
.
Psychological factors, such as stress, sleep deprivation, anxiety or anger, can contribute to poor seizure control and, in addition to pathological conditions, they may reduce the seizure threshold; for instance fever, infection, electrolyte imbalance, hypoglycaemia or hormonal changes. Female patients may find that their seizure frequency increases during menses, and catamenial epilepsy is a form of epilepsy where seizure occurrence is closely associated with the menstrual cycle[19]
. Patients with catamenial epilepsy may respond well to treatment with the carbonic anhydrase inhibitor, acetazolamide, with hormonal therapy or short courses of clobazam[19]
.
Lifestyle factors (e.g. alcohol or recreational drugs) can not only reduce the seizure threshold[11]
, but may also contribute to missed doses of anticonvulsant medication. Certain drugs (e.g. quinolones and tramadol) are known to reduce the seizure threshold and should be avoided if possible in people with epilepsy.
The introduction of anti-epileptic drugs (AEDs) with cytochrome-P450 enzyme-inducing properties (e.g. phenytoin, barbiturates, carbamazepine or topiramate) can reduce the activity of other components of the therapy, such as sodium valproate, lamotrigine or tiagabine. However, the additional activity of any newly initiated drug usually compensates for this. Consideration should be given to the effects of other enzyme-inducing drugs, including natural products. St. John’s wort is a common culprit, as patients are not aware that it constitutes a drug and may omit to mention they are taking it. Pharmacists should therefore aim to collect this information during routine history taking.
Classes of anti-epileptic drugs by mechanism of action
No single mode of action is predominant in any AED, and in some it is largely unknown. However, several modes of action are recognised as being more relevant than others.
Drugs acting on sodium channels
Many AEDs act by inhibiting the fast sodium current responsible for the fast upstroke of the action potential. The mechanism involves stabilising the inactive state of the voltage-gated sodium channel, thereby delaying the onset of the next action potential. This mode of action is common to most of the older anticonvulsants (e.g. phenytoin, carbamazepine and its analogues), as well as many of the newer ones (e.g. lamotrigine, lacosamide, zonisamide and rufinamide). For most AEDs, their effect is achieved by prolonging the fast inactivation phase, with the exception of lacosamide, which prolongs the slow inactivation phase involved in maintaining the resting membrane potential, giving it a slower onset of action but more prolonged activity[20],[21]
.
Carbamazepine, oxcarbazepine and eslicarbazepine are structurally related and are known to cause serious skin reactions, such as toxic epidermal necrolysis (TEN). Patients of Far Eastern origin should undergo genetic testing for HLA-B*1502 polymorphism prior to starting treatment with one of these drugs[22],[23],[24]
. Newer agents, including oxcarbazepine and eslicarbazepine, are often used in patients intolerant to therapeutic doses of carbamazepine. For instance, if a patient on carbamazepine is able to effectively control their epilepsy, but develops symptoms of hyponatraemia, often manifesting as fatigue, headache or muscle weakness, it may be worth considering switching to eslicarbazapine[25]
.
Inhibition of calcium currents contributes to the activity of certain AEDs, either reducing availability of the excitatory neurotransmitter glutamate, by inhibiting calcium-mediated vesicle release, or attenuating repetitive firing and spread of depolarisation. Ethosuximide is a selective calcium channel blocker specifically used for the treatment of absence seizures[20]
.
GABAergic drugs
Potentiation of the main inhibitory neurotransmitter in the brain, gamma-aminobutyric acid (GABA), is another target for anti-epileptic therapeutics. The drugs in this class include gabapentin, pregabalin, tiagabine and vigabatrin. Of these, only gabapentin is licensed for monotherapy, although rarely used as such, with the others being licensed as adjunctive therapy for partial-onset seizures with or without secondary generalisation. Despite these drugs having limited efficacy as anticonvulsants, pregabalin may be of value in anxious patients, being also licensed for generalised anxiety disorder, as a reduction in anxiety can contribute to improved seizure control. Vigabatrin is rarely used owing to irreversible visual field defects but still has a place in West syndrome, for which it has a monotherapy license, provided regular ophthalmology examinations are performed[26]
. Another drug in this class, retigabine, has recently been withdrawn following a reduction in use owing to serious adverse effects (i.e. blue pigmentation of the skin and eyes)[27],[28]
.
Barbiturates and benzodiazepines also exert their activity via modulation of GABA pathways. Barbiturates prolong the duration of GABA receptor opening and are effective anticonvulsants. However, phenobarbital has largely fallen out of use in the Western world owing to excessive drowsiness and long-term adverse effects (e.g. osteoporosis), which is in common with the other older AEDs[29]
. Benzodiazepines double the affinity of GABA for its receptors, which can be effective in the short term, but the development of tolerance makes them of limited use, except for the termination of status epilepticus or of cluster seizures[30]
. Buccal midazolam and rectal diazepam are licensed for this status. Clobazam, having the lowest propensity for sedation and tolerance in this class, is commonly used as rescue therapy for cluster seizures. Given at a dose of 10mg once or twice a day for three to five days, it can limit the duration of a cluster. Clonazepam is licensed for the treatment of epilepsy, either as monotherapy or as an adjunct, but is usually reserved as a last resort.
Others
Levetiracetam and a new drug in the same class, brivaracetam, reduce the amount of neurotransmitter released into the synaptic cleft by binding to synaptic vesicle glycoprotein 2A, thought to be involved in the docking and fusion of calcium-mediated vesicle release. These drugs confer an advantage over older anticonvulsants in that they are subject to little hepatic biotransformation, and thus unlikely to interact with other drugs. Side effects are uncommon but idiosyncratic, and sometimes include irritability or aggressive behaviour[31]
. Levetiracetam represented a breakthrough in AED therapy when it was launched and is currently one of the most widely prescribed AEDs. It is recommended by NICE as an alternative first-line option, and cost limitations no longer apply[6]
. The latest addition, brivaracetam, is as yet licensed in the UK only as adjunctive therapy for focal seizures[32]
. Having been launched around two years ago, it is too early to tell whether it will cause similar side effects. Brivaracetam may be used in combination with levetiracetam but the benefits are likely to be less than for other AED combinations[33]
. Phase IV studies monitoring its use are underway.
Perampanel is in a class of its own, being the only anticonvulsant to target α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors[34]
. It is a highly selective AMPA antagonist, leading to a reduction in excitatory activity. Whether because of this unique mechanism of action or otherwise, perampanel has proven remarkably effective as adjunctive therapy for a third of patients, ineffective for one third, and effective but intolerable for one third. Adverse effects (e.g. sedation, dizziness and ataxia) can be limited by taking it at bedtime. The long half-life enables once-daily dosing. Other side effects, such as irritability, aggression and behavioural changes, can be severe once a dosage of 6mg is reached, and may prove dose-limiting[34]
.
Drugs with multiple mechanisms of action
Many drugs possess multiple mechanisms of action. For instance, zonisamide inhibits carbonic anhydrase and AMPA receptors, along with sodium channels. While the mechanism of action of valproate is largely unknown, it demonstrates activity against sodium and calcium channels, acts as an N-methyl-D-aspartate receptor antagonist, and potentiates GABA. Despite recent bad press owing to concerns over teratogenicity (e.g. neural tube defects and intellectual impairment), it remains the most effective drug for generalised epilepsies[35]
. Valproate should be avoided in girls and women of childbearing age; however, where there are no suitable alternatives, patients must be fully informed of the risks should they become pregnant, enrolled on the pregnancy prevention programme, and given advice on contraception and details of who to contact. The Medicines and Healthcare products Regulatory Agency has developed a toolkit
[36]
to support healthcare professionals with this.
A recent review by Eadie examined anti-epileptic drug safety in pregnancy in more detail, along with the possible dangers for the pregnant woman and her foetus, and should be consulted for more information on this topic[37]
.
In practice, mechanism of action has less influence on the selection of drugs for refractory epilepsy than the side effect profile. In general, successive AEDs are offered, irrespective of mechanism of action, on a trial basis until the most effective and best tolerated combination is reached.
Strategies for management
First-line treatments
The basis of epilepsy therapy consists of a foundation drug, such as sodium valproate, carbamazepine, lamotrigine or levetiracetam[6]
.
When two successive first-line drugs have failed to achieve seizure freedom, a combination of two may be attempted. If this fails to produce a satisfactory response, adjunctive therapy with one of the following: lacosamide, zonisamide, perampanel, topiramate or brivaracetam, could be tried[6]
. Topiramate tends to be reserved until last, owing to its poor tolerability.
For first-line therapy, both NICE and the Scottish Intercollegiate Guidelines Network recommend sodium valproate for generalised tonic-clonic seizures, carbamazepine or lamotrigine for focal seizures, and sodium valproate or ethosuxamide for absence seizures, with the proviso that if sodium valproate is to be offered to girls or women of child-bearing age, the appropriate advice is given, as detailed above[6],[38]
, and in line with the update to its licence by the MHRA in April 2018.
Each drug should be introduced gradually to reduce side effects, one agent at a time to evaluate effect, and sufficient time at sufficient dosage allowed before deeming ineffective. An ineffective drug should be gradually withdrawn and replaced with another from the first-line group in an overlapping titration, where the first is reduced as the second is increased. Should a patient become seizure-free midway through a titration, then the switch can be halted at that stage. The patient can be advised to resume the titration only in the event of another seizure. For patients who are particularly sensitive to dose changes, the interval between the dose increases can be extended as tolerated. Dosages are often titrated fortnightly, except in the case of eslicarbazapine and perampanel where four weeks is usually allowed between dose increases to limit side effects. Eslicarbazapine is now available as 200mg tablets, at the same acquisition cost on a milligram basis as 800mg tablets, thus facilitating more individual titration regimens.
When selecting an alternative agent, consideration should be given to the patient’s previous AEDs, doses achieved and reasons for withdrawal, in order to offer an appropriate alternative.
As previously stated, patients with refractory epilepsy are unlikely to achieve seizure freedom with drugs. Therefore, alternative options should be offered. Certain types of epilepsy respond better to surgery than to drug therapy, particularly where there is a unilateral structural lesion, in whom the chances of seizure freedom may be up to 90% (e.g. non-dominant temporal lobe cavernoma)[12],[39],[40]
. Evaluation of suitability for epilepsy surgery involves intensive imaging, electroencephalography and psychological assessment.
Vagus nerve stimulation
When used as an adjunct to drug therapy, vagus nerve stimulation (VNS) can be effective in reducing the seizure frequency in some patients. The procedure usually involves the implantation of a pulse generator, akin to a pacemaker, beneath the skin of the upper thorax, from which an electrode is wound around the left vagus nerve in the neck. Modern devices sense tachycardia induced by impending seizures, triggering vagus stimulation to suppress the seizure. Side effects are minor and can include hoarseness of the voice or discomfort in the neck during stimulation. Nevertheless, many patients are reluctant to undergo this relatively simple procedure.
Prognosis
The consequences of refractory epilepsy extend beyond the physical consequences of the seizures themselves, such as falls and injuries, to affect patients’ quality of life and that of their relatives. Living with the constant uncertainty of unexpected disruptions to everyday life not only causes anxiety, depression and fear of stigmatisation, but also confers restrictions on driving, career options and the ability to get, or hold down, a job. Progressive deterioration in cognition and memory affects all people with epilepsy, caused not only by the seizures, but also by the drugs used to treat them, which for the majority of patients will be life long. In addition, life expectancy is shorter resulting from accidents, drowning or sudden unexpected death in epilepsy[10],
[18]
.
The goal for therapy should always be seizure freedom for patients with drug-resistant epilepsy, although the likelihood of achieving this with drugs alone is low [4],[7],[8]
. Therefore, it is important to manage the expectations of patients and their relatives from the outset, by explaining that a successful outcome may take the form of a reduction in the frequency of seizures, the duration, the severity, or in the recovery period, and by offering other strategies, such as surgery or VNS where appropriate. The ILAE define a therapeutic effect as three times the longest previous inter-seizure interval. In practice, this is determined from the previous 12 months, because a seizure frequency of less than once a year is considered to be seizure freedom[3],[5]
.
Financial and conflicts of interest disclosure:
The author has no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. No writing assistance was used in the production of this manuscript.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] World Health Organization (WHO). Epilepsy. WHO Factsheet, October 2012: number 999; 2014. Available at: www.who.int/mediacentre/factsheets/fs999/en/index.html (accessed May 2018)
[2] Joint Epilepsy Council of the UK and Ireland. Epilepsy prevalence, incidence and other statistics. 2011. Available at: http://www.epilepsyscotland.org.uk/pdf/Joint_Epilepsy_Council_Prevalence_and_Incidence_September_11_(3).pdf (accessed May 2018)
[3] Fisher RS, Acevedo C, Arzimanoglou A et al. ILAE Official Report: a practical clinical definition of epilepsy. Epilepsia 2014;55:475–482. doi: 10.1111/epi.12550
[4] Kwan P & Sander JW. The natural history of epilepsy: an epidemiological view. J Neurol Neurosurg Psychiatry 2004;75:1376–1381. doi: 10.1136/jnnp.2004.045690
[5] Kwan P, Arzimanoglou A, Berg AT et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010;51:1069–1077. doi: 10.1111/j.1528-1167.2009.02397.x
[6] National Institute for Health and Care Excellence (NICE). Epilepsies: diagnosis and management [CG137]. 2012, updated 2016. Available at: https://www.nice.org.uk/guidance/cg137 (accessed May 2018)
[7] Picot M-C, Baldy-Moulinier M, Daurès J-P et al. The prevalence of epilepsy and pharmacoresistant epilepsy in adults: a population-based study in a Western European country. Epilepsia 2008;49:1230–1238. doi: 10.1111/j.1528-1167.2008.01579.x
[8] Kwan P & Brodie MJ. Early identification of refractory epilepsy. N Engl J Med 2000;342:314–319. doi: 10.1056/NEJM200002033420503
[9] Schiller Y & Najjar Y. Quantifying the response to anti-epileptic drugs: effect of past treatment history. Neurology 2008;70:54–65. doi: 10.1212/01.wnl.0000286959.22040.6e
[10] Rugg-Gunn FJ & Sander JW. Management of chronic epilepsy. BMJ 2012;345:e4576. doi: 10.1136/bmj.e4576
[11] Schuele SU & Lüders HO. Intractable epilepsy: management and therapeutic alternatives. Lancet Neurol 2008;7:514–524. doi: 10.1016/S1474-4422(08)70108-X
[12] Wiebe S, Blume WT, Girvin JP, Eliasziw M, and the Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 2001;345:311–318. doi: 10.1056/NEJM200108023450501
[13] O’Callaghan FJK, Edwards SW, Alber FD et al. Safety and effectiveness of hormonal treatment versus hormonal treatment with vigabatrin for infantile spasms (ICISS): a randomised, multicentre, open-label trial. Lancet Neurol 2017;16:33–42. doi: 10.1016/S1474-4422(16)30294-0
[14] Brunklaus A & Zuberi SM. Dravet syndrome—from epileptic encephalopathy to channelopathy. Epilepsia 2014;55:979–984. doi: 10.1111/epi.12652
[15] Smith D, Defalla BA & Chadwick DW. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. QJM 1999;92:15–23. doi: 10.1093/qjmed/92.1.15
[16] LaFrance WC, Baker GA, Duncan R et al. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach. A report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia 2013;54:2005–2018. doi: 10.1111/epi.12356
[17] Gavvala JR & Schuele SU. New-onset seizure in adults and adolescents: a review. JAMA 2016;316(24):2657–2668. doi: 10.1001/jama.2016.18625
[18] Laxer KD, Trinka E, Hirsch LJ et al. The consequences of refractory epilepsy and its treatment. Epilepsy Behav 2014;37:59–70. doi: 10.1016/j.yebeh.2014.05.031
[19] Verrotti A, D’Egidio C, Agostinelli S et al. Diagnosis and management of catamenial seizures: a review. Int J Womens Health 2012;4:535–541. doi: 10.2147/IJWH.S28872
[20] Meldrum BS. Update on the mechanism of action of anti-epileptic drugs. Epilepsia 1996;37(6):S4–S11. PMID: 8941036
[21] Rogawski MA, Tofighy A, White HS et al. Current understanding of the mechanism of action of the anti-epileptic drug lacosamide. Epilepsy Res 2015;110:189–205. doi: 10.1016/j.eplepsyres.2014.11.021
[22] Novartis Pharmaceuticals UK Ltd. Tegretol Prolonged Release 400mg Tablets (formerly Tegretol retard). Summary of Product Characteristics last updated on eMC 11 January 2018. Available at: https://www.medicines.org.uk/emc/product/7843/smpc#CLINICAL_PRECAUTIONS (accessed May 2018)
[23] Novartis Pharmaceuticals UK Ltd. Trileptal 600 mg film-coated tablets. Summary of Product Characteristics last updated on eMC 13 March 2018. Available at: https://www.medicines.org.uk/emc/product/7852/smpc#CLINICAL_PRECAUTIONS (accessed May 2018)
[24] Eisai Ltd. Zebinix 200 mg tablets. Summary of Product Characteristics last updated on eMC 29 August 2017. Available at: https://www.medicines.org.uk/emc/product/4460/smpc (accessed May 2018)
[25] Ben-Menachem E, Gabbai AA, Hufnagel A et al. Eslicarbazepine acetate as adjunctive therapy in adult patients with partial epilepsy. Epilepsy Res 2010;89:278–285. doi: 10.1016/j.eplepsyres.2010.01.014
[26] Sanofi. Sabril 500 mg film-coated tablets. Summary of Product Characteristics, last updated on eMC 14 July 2014. Available at: https://www.medicines.org.uk/emc/product/4279/smpc (accessed May 2018)
[27] Medicines and Healthcare Products Regulatory Agency (MHRA), 2017. Letters sent to healthcare professionals in April 2017, including a reminder of the retigabine (Trobalt) withdrawal. Available at: https://www.gov.uk/drug-safety-update/letters-sent-to-healthcare-professionals-in-april-2017-including-a-reminder-of-the-retigabine-trobalt-withdrawal (accessed May 2018)
[28] Medicines and Healthcare Products Regulatory Agency (MHRA), 2014. Retigabine (Trobaltâ–¼): indication restricted to last-line use and new monitoring requirements. Available at: https://www.gov.uk/drug-safety-update/retigabine-trobalt-indication-restricted-to-last-line-use-and-new-monitoring-requirements (accessed May 2018)
[29] Brodie MJ & Kwan P. Current position of phenobarbital in epilepsy and its future. Epilepsia 2012;53(8):40–46. doi: 10.1111/epi.12027
[30] Miller LG, Greenblatt DJ, Barnhill JG et al. Chronic benzodiazepine administration. I. Tolerance is associated with benzodiazepine receptor downregulation and decreased g-aminobutyric acidA receptor function. J Pharmacol Exp Ther 1988;246:170–176. PMID: 2839660
[31] UCB Pharma Limited. Keppra 500 mg film-coated tablets. Summary of Product Characteristics, last updated on eMC 2 January 2017. Available at: https://www.medicines.org.uk/emc/product/2293/smpc (accessed May 2018)
[32] Kwan P, Trinka E, Paesschen WV et al. Adjunctive brivaracetam for uncontrolled focal and generalized epilepsies: results of a phase III, double-blind, randomized, placebo-controlled, flexible-dose trial. Epilepsia 2014;55:38–46. doi: 10.1111/epi.12391
[33] UCB Pharma. Briviact film-coated tablets. Summary of Product Characteristics. Last updated on eMC 3 May 2017. Available at: https://www.medicines.org.uk/emc/product/1963/smpc (accessed May 2018)
[34] Besag FMC & Patsalos PN. Clinical efficacy of perampanel for partial-onset and primary generalized tonic-clonic seizures. Neuropsychiatr Dis Treat 2016;12:1215–1220. doi: 10.2147/NDT.S83842
[35] Marson AG, Al-Kharusi AM, Alwaidh M et al. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet 2007;369:1016–1026. doi: 10.1016/S0140-6736(07)60461-9
[36] Medicines and Healthcare Products Regulatory Agency (MHRA). Valproate use by women and girls. Available at: www.gov.uk/government/publications/toolkit-on-the-risks-of-valproate-medicines-in-female-patients (accessed May 2018)
[37] Eadie M. Antiepileptic drug safety in pregnancy. Clinical Pharmacist 2016;8:24–31. Available at: https://www.pharmaceutical-journal.com/research/review-article/anti-epileptic-drug-safety-in-pregnancy-possible-dangers-for-the-pregnant-woman-and-her-foetus/20200320.article (accessed May 2018)
[38] Scottish Intercollegiate Guidelines Network (SIGN). SIGN 143. Diagnosis and management of epilepsy in adults. Available at: http://www.sign.ac.uk/sign-143-diagnosis-and-management-of-epilepsy-in-adults.html (accessed May 2018)
[39] West S, Nolan SJ, Cotton J et al. Surgery for epilepsy. Cochrane Database Syst Rev 2015;7:CD010541. doi: 10.1002/14651858.CD010541.pub2
[40] de Tisi J, Bell GS, Peacock JL et al. The long-term outcome of adult epilepsy surgery, patterns of seizure remission, and relapse: a cohort study. Lancet 2011;378:1388–1395. doi: 10.1016/S0140-6736(11)60890-8
You might also be interested in…

Epilepsy drugs levetiracetam and zonisamide should not be routinely used first line in the NHS, conclude researchers

No difference in cognitive outcomes in children born to women taking antiseizure medicines
