
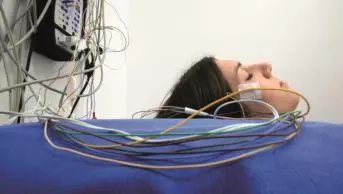
Amelie-Benoist / BSIP / Science Photo Library
Summary
Selecting active treatments for sleep disorders mostly occurs in the absence of significant controlled data from trials or evidence-based protocols. Drug treatments used in clinical practice to improve sleep-wake disturbances are frequently recommended empirically, almost always in the absence of a formal licence from regulatory authorities. Nevertheless, given the numerous deleterious effects of a disordered sleep-wake cycle on a patient’s ability to function normally, even small improvements following therapeutic intervention are welcome.
Non-pharmacological and pharmacological options are often employed for the the treatment of primary insomnia. Non-pharmacological treatments rely on fostering good ‘sleep hygiene’. For patients with moderate or severe insomnia not responsive to simple sleep hygiene advice, a more structured approach is used and cognitive behaviour therapy tailored to treat insomnia (CBT-I) is the best proven therapy, although its availability varies greatly between health systems. Some insomnia patients will respond to a combination of CBT-I and drug therapy although there is no evidence to support or refute this. Drug treatment for insomnia is controversial, especially when symptoms are chronic and the National Institute for Care and Health Excellence (NICE) suggests that the use of hypnotic agents for more than four weeks is inadvisable. Benzodiazepines, the so-called “Z drugs”, and melatonin are frequently used in clinical practice in insomnia. Antidepressants or other psychoactive drugs can also be used as surrogate hypnotic agents.
When obstructive sleep apnoea has been diagnosed and is severe enough to impact on daytime alertness, the first-line therapy is continuous positive airway pressure. In narcolepsy, first-line therapy is modafinil, however a considerable proportion of narcoleptic patients will not achieve adequate control of excessive daytime sleepiness with modafinil alone and an alternative psychostimulant, such as dexamphetamine or methylphenidate, is usually added. Although not formally licenced for conditions other than narcolepsy, modafinil, with or without additional amphetamine-like agents, is used in practice for conditions such as idiopathic hypersomnolence.
Selecting active treatments for sleep disorders mostly occurs in the absence of significant controlled data from trials or evidence-based protocols. Drug treatments used in clinical practice to improve sleep-wake disturbances are frequently recommended empirically, almost always in the absence of a formal licence from regulatory authorities. Nevertheless, given the numerous deleterious effects of a disordered sleep-wake cycle on a patient’s ability to function normally, even small improvements following therapeutic intervention are welcome.
This article will focus primarily on the treatment of insomnia, sleep-related breathing disorders and central disorders of hypersomnolence.
Insomnia
One third of patients visiting their GP will report that their sleep pattern is disturbed if directly asked, a figure that rises to two thirds if the primary complaint relates to mental health[1]
. Insomnia is therefore an extremely common complaint. Persistent insomnia often appears as a predominant and potentially disabling factor that dominates any medical consultation and merits direct attention. Prior to diagnosing primary insomnia, other secondary causes of insomnia should be sought and treated where possible.
Non-pharmacological treatment for primary insomnia initially relies on fostering good ‘sleep hygiene’, although relatively few patients and doctors alike have a full understanding of this term and the factors involved[2]
. Optimisation of the sleeping environment and improving routines, behaviours or attitudes conductive to good sleep are crucial (see ‘Maladaptive behaviours that can be adjusted to improve sleep quality or ‘sleep hygiene’’). No universal approach for optimising the sleeping environment exists and individual preferences should be explored. For example, the sensory deprivation associated with complete darkness or ear plugs may suit some, but others may find they then focus on internal noises such as breathing, which is counterproductive to sleep onset. Appropriate temperature and light levels in the bedroom should also be explored. Excluding televisions and computers from the sleeping environment is also advisable.
Maladaptive behaviours that can be adjusted to improve sleep quality or ‘sleep hygiene’
- Engaging in stimulating mental activities up to the point of attempted sleep onset;
- Using the bedroom for activities other than sleep, including watching or listening to media;
- Inconsistent sleep-wake schedule through the week and weekend;
- Excessive checking of the clock through the night;
- Consuming foods either shortly before bed or through the night, particularly if acid reflux present;
- Inappropriate caffeine intake (note: some people are particularly sensitive to low dose caffeine);
- Using alcohol habitually as an aid to sleep onset;
- Inadequate physical activity or exercise during the day, particularly if no exposure to natural light;
- Intense exercise within two hours of attempted sleep.
Mild insomnia may respond to the correction of maladaptive routines, such as the avoidance of large meals, stimulant drinks or exercise within two hours of intended sleep onset. Various techniques to actively encourage relaxation at least 30 minutes before bed may also help. Focused breathing exercises developed from yoga and centred on the diaphragm can be particularly beneficial[3]
. A consistent sleep-wake schedule across the week is also recommended. Daytime naps should generally be avoided to optimise the drive to sleep before bed.
For patients with moderate or severe insomnia who are not responsive to simple sleep hygiene advice, current guidelines recommend more structured non-pharmacological approaches as first-line treatment[4]
. Although cognitive behaviour therapy tailored to treat insomnia (CBT-I) is the best proven therapy, its availability varies greatly between health systems. In the UK, where the majority of health provision is funded from public finance, insomnia services have struggled to become established, partly as a result of competition for resources from more established areas of health where clear targets have become defined[5]
. To improve the cost-effectiveness of CBT-I, a ‘stepped care’ approach has been proposed that comprises a hierarchy of five levels of CBT-I with options of referring subjects ‘upstream’ if there is an incomplete therapeutic response[5]
.
Another approach is to provide detailed self-help guides or online packages that deliver a form of CBT-I as an alternative cost-effective treatment. Measures of efficacy have shown mild to moderate objective improvements, but adherence rates are good[6]
. Computerised CBT-I has not yet been compared systematically with face-to-face consultations either individually or in groups.
A typical CBT-I programme of any kind will last six weeks and will cover at least four areas[7]
(see ‘CBT-I programmes’). It is likely that some insomnia patients will respond to a combination of CBT-I and drug therapy, although there is no evidence to support or refute this. Some evidence suggests, however, that CBT-I during hypnotic drug discontinuation can be useful[4]
.
CBT-I programmes
A typical CBT-I programme will cover:
- Relaxation therapy: designed to alleviate intrusive thoughts or somatic tension when trying to sleep and uses visual imagery, together with physical techniques, to control muscle tension largely through breathing exercises[3]
. - Stimulus control therapy: aims to re-establish the bed and bedroom with sleep and is particularly successfully in those with conditioned insomnia, in whom the bedroom causes high levels of cognitive arousal[8]
. A subject is encouraged not to stay in bed for more than 15 minutes when trying to sleep and, instead, to engage in a soporific activity outside the bedroom. Return to bed is appropriate when extreme drowsiness is achieved. - Sleep restriction therapy: aims to curtail the amount of sleep achieved to the time actually spent in bed. To this end, diaries are completed and time in bed is matched with estimated total sleep time so that sleep efficiency inevitably increases. Initially, this leads to significant sleep deprivation and this subsequently drives better sleep efficiency. Gradually, time in bed is increased by around 15–30 minutes a week until a target sleep efficiency of around 80–90% is reached[9]
. - Paradoxical intention: aims to eliminate performance anxiety, which may inhibit sleep onset. Subjects are encouraged to actively adopt a state of quiet wakefulness and not to attempt to sleep. This is thought to improve acceptance of the drowsy, yet wakeful, state and has links with the technique of mindfulness[10]
.
A structured and disciplined approach is essential for optimal results.
Drug treatment for insomnia is controversial, especially when symptoms are chronic. Many patients harbour unrealistic expectations that simple drug therapy will solve the issue. In practice, short-term treatment with hypnotic agents for a week or two in the context of a life event, such as bereavement, can be helpful. If sleep remains abnormal for longer, chronic use of drugs is of questionable benefit and is accompanied by fears of developing tolerance, physical dependence and withdrawal reactions[11]
. Long-term data proving harmful effects or poor outcomes are lacking[12]
, although epidemiological evidence suggests that long-term benzodiazepine use may be a risk factor for developing dementia[13]
. This conclusion has been challenged by case control analyses[14]
and some argue that the underlying reasons for the sleep-related symptoms leading to hypnotic use are more pertinent.
Guidance from the National Institute for Care and Health Excellence (NICE) suggests that the use of hypnotic agents for more than four weeks is inadvisable[15]
. Recent guidelines from the British Association of Psychopharmacology (BAP) propose a less strict approach when using short-acting hypnotics to treat insomnia and advise that there is an ‘exit strategy’ for discontinuation of drug therapy[12]
. In particular, given uncertainties regarding optimum or safe length of any drug treatment, a strategy of periodically trying to taper medication has been advocated with a view to restarting if unsuccessful[16]
. The BAP also advocates that the properties of an individual hypnotic agent should be tailored to the patient’s particular pattern of insomnia[12]
.
The majority of hypnotic agents, including benzodiazepines and the so-called “Z drugs”, enhance the inhibitory effects of gamma-aminobutyric acid (GABA) at the GABAA receptor to induce sleepiness[12]
. Extremely short-acting agents to aid significant sleep-onset insomnia include zaleplon and zolpidem. Zaleplon is licensed for short-term use (up to two weeks) and has few residual morning side effects given its short half-life (less than one hour). As with all hypnotics, the potential adverse effects on driving or other potentially dangerous pursuits should be emphasised. However, regarding zaleplon, it is worth noting that the US aviation authorities allow pilots to fly six hours after taking the agent[17]
. Zolpidem is a similar agent but it is formally licensed for use for up to four weeks. Both drugs are typically used in doses of 10mg before bed and are not safe to take with alcohol, largely because of risks of respiratory depression. The elderly population may not tolerate these drugs well and care should be taken. Pregnancy data is lacking but regular use is not advised.
Zopliclone, another Z-drug more commonly used in the UK at a dose of 7.5mg, has a slightly longer half-life (four to six hours) and may be the drug of choice if sleep maintenance is also a symptomatic issue. It is licensed for use for up to four weeks and has few significant side effects other than a metallic taste, which can be unpleasant. As with the majority of hypnotic agents, it is relatively contraindicated in those with generalised muscle weakness or significant sleep apnoea.
Relatively short-acting benzodiazepines, such as temazepam, are being used less, largely because of concerns about misuse or dependence[12]
.
Melatonin, usually in a prolonged release formulation, is widely used in practice to aid sleep onset and continuity, but it is only licenced for fairly short-term use in those aged over 55 years[7]
. This restricted licence reflects the available drug trial evidence[18]
and most authorities consider it to be an extremely safe agent free of side effects, albeit with limited efficacy. Caution is recommended when used in subjects with an autoimmune disease, although this concern is debated, especially as the drug has reported antioxidant effects and might actually be helpful in reducing inflammation[19],[20]
. The long-acting preparation currently available in the UK is Circadin (Neurim Pharmaceuticals), most often used at a dose of 2mg once daily, one to two hours before bedtime, for up to 13 weeks.
Although formal data are lacking, in practice it is common in both primary and secondary care settings to prescribe sedating antidepressants or other psychoactive drugs as surrogate hypnotic agents in the absence of any clear mood disorder or psychosis[12]
. Amitriptyline is most commonly used in this setting at a dose of 10–50mg, although trazodone (100–150mg) and mirtazapine (15–30mg) are also prescribed, usually at doses lower than those that produce an antidepressant effect. In cases of primary insomnia, however, it is not advisable to prescribe antidepressants or antipsychotic agents, such as quetiapine, unless there is clear evidence for associated mental health problems[12]
. The risks of harm after overdose are considerably higher than with hypnotic drugs of the “Z class”, for example[12]
.
Neuropathic pain agents, such as pregabalin, may also be prescribed off licence in practice to help sleep continuity, especially if pain or anxiety are factors in fuelling insomnia. A dose of 75–150mg before bed can be helpful given the lack of contraindications and good side effect profile. Pregabalin has the advantage that it enhances the deeper non-rapid eye movement (NREM) stages of sleep, unlike many other psychoactive sedatives, and potentially could produce more refreshing sleep[21]
.
The evidence that over-the-counter preparations, such as antihistamines, help those with significant chronic insomnia is limited[22]
.
Restless legs syndrome
When considering severity, restless legs syndrome (RLS) has a very wide spectrum. In a small number of patients, it occurs on a nightly basis and severely interferes with sleep onset and continuity, fuelling daytime somnolence. It is often appropriate to consider drug therapy once other factors, such as iron deficiency, have been addressed. Most controlled evidence exists for the use of low dose non-ergot dopamine agonists (rotigotine, available as a transdermal patch, and the oral agonists, pramipexole and ropinirole) as effective agents to suppress the restlessness or sensory discomfort in RLS and also possibly the involuntary leg movements that may disrupt sleep (periodic limb movements [PLMs])[23]
.
Rotigotine has few side effects, although a skin reaction or reddening may limit its use. A dose of 1mg taken once daily, increasing every two weeks by 1mg, to a maximum of 3mg is a usual regime. Ropinirole is generally started at 250µg and is increased over several weeks to 2mg or even 4mg before bed. It should be avoided in significant renal or hepatic impairment. Pramipexole is used similarly with a dose range 88–540µg. Caution and dose reduction are recommended in patients with renal impairment.
When used in Parkinson’s disease, the risk of impulse control disorders induced by dopamine agonists is a serious problem[24]
. Although the risks are almost certainly smaller when these drugs are used for RLS, reports of compulsive behaviours have been published and any abnormal behaviours should be explored and monitored[25]
.
Although RLS may be particularly severe during pregnancy, in general dopamine agonists should be avoided even though clinical evidence for harm is lacking.
Care needs to be taken to avoid dose escalation with dopamine agonists as augmentation is likely. This describes the situation where symptoms paradoxically occur earlier in the day and affect other body parts, including the arms following an increase in dose of a dopamine agonist[26]
.
In patients only partially or non-responsive to dopaminergic agents, second-line treatments include neuropathic pain agents, such as gabapentin or pregabalin, for which there is limited drug trial evidence[27]
. In the absence of any controlled evidence, intermittent use of opioids, such as codeine or similar agents including tramadol, can also be a useful strategy for severe RLS[28]
. Although not licenced for use in RLS or PLMs, there is some evidence that clonazepam before bed (0.5–2mg) will suppress excessive leg movement and improve sleep continuity in a relatively non-specific way[29]
.
Sleep apnoea
When obstructive sleep apnoea (OSA) has been diagnosed and is severe enough to impact on daytime alertness, the first-line therapy is continuous positive airway pressure (CPAP), in which air is delivered to the upper airways at 10cmH2 0, via a mask[30]
and acts to splint the airways and abolish snoring. CPAP masks can be poorly tolerated and a variety of shapes and types are now available, often with humidifiers. Encouragement from a multidisciplinary team with frequent follow-up assessments greatly helps compliance.
Surgical removal of pharyngeal tissue is now rarely considered a useful strategy, although a limited palatoplasty using laser treatment can be helpful in socially disruptive snoring. Similarly, if snoring and subsequent apnoeas are thought to be secondary to nasal pathology, surgery is often curative as is tonsillectomy in severely affected children[31]
. Mandibular advancement devices are increasingly used in mild OSA, although their use requires good dentition[32]
.
Hypersomnolence
The most disabling symptom of narcolepsy is the inability to stay appropriately alert for more than a few hours and a significant majority of patients benefit from wake-promoting drug therapy[33]
. Lifestyle adjustments are often helpful; many patients are encouraged to plan a fairly short nap, usually in the afternoon. Most patients with narcolepsy are often refreshed by short sleep episodes, unlike most other sleep disorders causing hypersomnolence. Anecdotal evidence exists that narcolepsy sufferers are more prone to post-prandial sleepiness, especially after meals rich in carbohydrate[34]
. Some patients report that dietary manipulation, such as consuming small meals high in protein several times a day, helps their hypersomnolence.
The number of stimulant drugs available for treating excessive sleepiness in narcolepsy is relatively small (see ‘Compounds used to treat excessive daytime sleepiness in narcolepsy’). Caffeine, whether taken as a food supplement or in drink form, can be useful, usually as an add-on therapy, and should not be overlooked. However, modafinil has emerged over the past 15 years as a first-line treatment and is typically started at a dose of 100mg morning and lunchtime, with a view to doubling the dose after a few weeks if necessary[35]
. Modafinil’s mode of action is still debated but a dopaminergic mechanism is likely in the absence of direct synaptic effects on dopamine receptors. It is generally well tolerated with minor gastrointestinal side effects or headache as the only common problems. Mood disorder or personality change is occasionally encountered and can limit usefulness. Sympathomimetic side effects are usually trivial, but blood pressure monitoring is advisable and care is needed in the elderly with cardiac pathology or hypertension. It is usually contraindicated in severe uncontrolled hypertension or if there are significant cardiac arrhythmias.
| Compounds used to treat excessive daytime sleepiness in narcolepsy | |||
|---|---|---|---|
*Notes on level of evidence: I. Randomised, well-designed trials with low alpha and beta error, or meta-analyses of randomised controlled trials with homogeneity of results II. Randomised trials with high alpha and beta error, methodological problems or high quality cohort studies III. Non-randomised or case-control studies IV. Case-control or cohort studies with methodological problems, or case series V. Expert opinions, or studies based on physiology or bench research | |||
| Compound | Proposed mechanism of action | Usual total daily dose | Level of evidence* |
| Dexamphetamine | Increased monoamine release (especially dopamine) by reverse efflux of dopamine via dopamine transporter; also inhibition of monoamine storage via vesicular monoamine transporter. | 5–60mg | III, V |
| Methylphenidate | Blocks monoamine uptake (dopamine>noradrenaline). | 20–60mg | II, V |
| Modafinil | Probably selective dopamine reuptake inhibition | 100–400mg | I, II |
| Selegiline | Monoamine oxidase inhibitor type B; drug is metabolised to amphetamine. | 10–40mg | III |
| Pitolisant | Inverse agonist at histamine type 3 receptors. | 10–30mg | II |
| Sodium oxybate | Consolidates good quality nocturnal sleep by gamma-aminobutyric acid type B receptor agonism. | 3–9g | I, IV |
A considerable proportion of narcoleptic patients will not achieve adequate control of excessive daytime sleepiness with modafinil alone and it is often useful to add an alternative psychostimulant, such as dexamphetamine or methylphenidate. These drugs have very similar modes of action (see ‘Compounds used to treat excessive daytime sleepiness in narcolepsy’) and can usually be used flexibly. At low doses, tolerability is not usually a problem, although weight loss caused by appetite suppression needs to be monitored. As with modafinil, these drugs are contraindicated in significant cardiovascular disease including arrhythmia. Of interest, the potential for abuse appears low in narcoleptic patient populations[35]
.
A number of unlicensed medications are used in practice to improve wakefulness. Selegiline was originally developed for Parkinson’s disease and has a complex metabolic pathway that results in several amphetamine derivatives[36]
. Daily doses of 20–40mg can be a useful strategy in improving daytime alertness, particularly in the elderly or if conventional medication is not tolerated. Pitolisant, a new drug developed for narcolepsy, is an inverse histamine (H3) receptor agonist, which is likely to gain a formal licence for treating sleepiness in narcolepsy in 2016[37]
. Trial data are limited to date[38]
but the drug is likely to be a useful addition, especially given its novel mode of action.
In theory, improving the characteristically fragmented nocturnal sleep in narcolepsy might be expected to improve daytime wakefulness. However, the only drug with evidence-based data to support this approach is sodium oxybate, which was originally licenced for treating cataplexy (see ‘Cataplexy’)[39]
.
Cataplexy
Although rare, cataplexy can be the most disabling symptom in narcolepsy and around 30% of patients with narcoleptic syndromes receive specific drug treatment for it. In general, cataplexy is less severe during full alertness and wake-promoting therapy can be helpful. In patients experiencing either severe and/or daily episodes, other regular therapy is warranted. Venlafaxine and clomipramine are commonly used at daily doses lower than when used for their antidepressant effects (typically, 75–150mg and 20–75mg, respectively)[35]
. Both drugs should be used cautiously if there is risk of cardiac arrhythmia and avoided if possible in pregnancy. Side effects tend to be gastrointestinal in nature but are rarely limiting.
Both clomipramine and venlafaxine create a neurochemical environment in the brain that generally inhibits the onset of REM sleep and therefore helps to prevent elements of REM sleep, such as paralysis or cataplexy, intruding into the wakeful state.
Other classes of antidepressant, including selective serotonin reuptake inhibitors (SSRIs), appear to have mild positive effects in treating cataplexy[40]
.
When using a regular drug treatment of an antidepressant class for cataplexy, patients should be encouraged to be compliant and regular with their dosing, as major problems with severe rebound cataplexy can occur with abrupt discontinuation[41]
.
Sodium oxybate appears to be the most effective drug for cataplexy, abolishing up to 85% of episodes in severely affected patients[42]
. The use of sodium oxybate is controversial, partly on account of its misuse in the community as gamma-hydroxybutyrate (GHB), but mostly because of its considerable expense. However, it is effective in treating most of the symptoms of narcolepsy when given in divided doses overnight in liquid form (total doses 3–9g). Because of its potential effects on respiratory depression, benzodiazepines and alcohol should be avoided and care should be taken if there are associated breathing problems including sleep apnoea. Although short-acting, it strongly promotes deep NREM sleep and helps sleep continuity with minimal ‘hangover’ effects. By improving nocturnal sleep, it enhances daytime wakefulness in many patients. Its positive effects in suppressing cataplexy occur through an obscure mechanism that often takes several weeks to materialise[42]
.
Other central hypersomnias
Although not formally licenced for conditions other than narcolepsy, modafinil, with or without additional amphetamine-like agents, is used in practice for conditions such as idiopathic hypersomnolence (IH). Experimental evidence suggests that flumazenil given via the oral route may benefit some patients with IH, a finding of interest given the demonstration of an endogenous benzodiazepine-like substance in the cerebrospinal fluid of some patients[43]
.
Rarely, narcolepsy-like levels of sleepiness may occur after brain surgery involving regions near the hypothalamus and drug treatment to improve wakefulness is appropriate. More commonly, after head trauma or other global insults such as meningitis, severe daytime sleepiness may persist as a significant isolated symptom[44]
. On the grounds that these subjects have a secondary form of narcolepsy, often with presumed damage to the hypothalamus or its output pathways, treatment protocols for narcolepsy are used with modafinil as a first-line agent.
In a number of neurological conditions, severe daytime sleepiness may occur as a relatively isolated and largely unexplained phenomenon. These include Parkinson’s disease, myotonic dystrophy and inflammatory diseases such as multiple sclerosis[35]
. Modafinil is often used empirically to promote wakefulness, given its relatively benign safety profile. The drug is much less efficacious if the symptom is predominantly fatigue as opposed to frank hypersomnolence[45]
.
Parasomnias
Most children with frequent parasomnias arising from non-rapid eye movement (NREM) sleep find that the problem improves with age, however, it is not uncommon for adults exhibiting frequent or particularly disturbing nocturnal disturbances to be referred to sleep clinics for advice on management. Unfortunately, there is little evidence-based data to guide treatment options[12]
.
In general, sleep deprivation acts to provoke NREM parasomnia activity and advice on obtaining sufficient sleep may be helpful. Overnight testing with polysomnography is sometimes useful to identify potentially reversible factors such as severe snoring or excessive limb movements that might potentially be fuelling a parasomnia. If drug treatment is thought appropriate, short courses for a few weeks are usual. If sleepwalking or similar phenomena are particularly more likely when sleeping in hotels, for example, intermittent therapy during risky periods is sometimes advocated. Little evidence is available to help guide drug choice, but most sleep physicians would use clonazepam as a first-line agent (dose 0.25–2mg before bed). Anecdotal evidence suggests that selective serotonin reuptake inhibitors (SSRIs), such as paroxetine, can be helpful. If the parasomnia is particularly agitated, clomipramine (dose around 25mg) is sometimes beneficial. Long-acting melatonin is also occasionally recommended as an agent to improve general sleep continuity.
Rapid eye movement (REM) sleep behaviour disorder (RBD), which most often affects middle-aged or elderly men, is the most common REM sleep parasomnia observed in sleep clinics. In RBD, aggressive dream enactment with vocalisation on a nightly basis happens regularly, with risk of injury to the subjects themselves and their bed partners. Clonazepam has become established as the first-line treatment, again in the absence of detailed or controlled trial data[46]
. Prolonged release melatonin, often at doses higher than used for simple insomnia (2–8mg), is also increasingly used to apparent good effect[47]
. Perhaps paradoxically, drugs that tend to suppress REM sleep, such as venlafaxine or mirtazepine, often worsen RBD, particularly if there is an underlying condition such as Parkinson’s disease[48]
. Such agents should be discontinued if possible.
Paul Reading
is a consultant neurologist at The James Cook University Hospital, South Tees Hospitals NHS Trust.
References
[1] Sateia MJ, Doghramji K, Hauri PJ et al. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep 2000;23(2):243–308. PMID: 10737342
[2] Stepanski EL & Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev 2003;7(3):215–225. doi:10.1053/smrv.2001.0246
[3] Kennedy SL. Yoga as the “next wave” of therapeutic modalities for treatment of insomnia. Int J Yoga Therap 2014;24:125–129. PMID: 25858659
[4] Morin CM, Bootzin RR, Buysse DJ et al. Psychological and behavioural treatment of insomnia: update of the recent evidence (1998-2004). Sleep 2006;29(11):1398–1414. PMID: 17162986
[5] Espie CA. “Stepped care”: a health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep 2009;21(12):1549–1558. PMCID: PMC2786038
[6] Cheng SK & Dizon J. Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis. Psychother Psychosom 2012;81(4):201–216. doi:10.1159/000335379
[7] Perlis M, Aloia M & Kuhn B. Behavioral Treatments for Sleep Disorders. A Comprehensive Primer of Behavioral Sleep Medicine Interventions. London, UK: Academic Press; 2011.
[8] McGowan SK & Behar E. A preliminary investigation of stimulus control training for worry: effects on anxiety and insomnia. Behav Modif 2013;37(1):90–112. doi:10.1177/0145445512455661
[9] Falloon K, Elley CR, Fernando A 3rd, et al. Simplified sleep restriction for insomnia in general practice: a randomised controlled trial. Br J Gen Pract 2015;65(637):e508–515. doi:10.3399/bjgp15x686137
[10] Ascher LM & Efran JS. Use of paradoxical intention in a behavioral program for sleep onset insomnia. J Consult Clin Psychol 1978;46(3):547–550. doi:10.1037//0022-006x.46.3.547
[11] Weaver MF. Prescription sedative misuse and abuse. Yale J Biol Med 2015;88(3):247–256. PMCID: PMC4553644
[12] Wilson SJ, Nutt DJ, Alford C et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. J Psychopharmcol 2010;24(11):1577–1601. doi:10.1177/0269881110379307
[13] Billioti de Gage S, Moride Y, Ducruet T et al. Benzodiazepine use and risk of Alzheimer’s disease: case-control study. BMJ 2014;349:g5205. doi:10.1136/bmj.g5205.
[14] Imfield P, Bodmer M, Jick SS et al. Benzodiazepine use and risk of developing Alzheimer’s disease or vascular dementia: a case-control analysis. Drug Saf 2015;38(10):909–919. doi:10.1007/s40264-015-0319-3
[15] National Institute for Health and Care Excellence (NICE). Clinical Knowledge Summary: managing long-term insomnia. Available at: http://cks.nice.org.uk/insomnia#!scenario:1 (accessed September 2015).
[16] Krystal AD. A compendium of placebo-controlled trials of the risks/benefits of pharmacological treatments for insomnia: the empirical basis for U.S. clinical practice. Sleep Med Rev 2009;13(4):265–274. doi:10.1016/j.smrv.2008.08.001
[17] Aviation Medicine Advisory Service (AMAS). Medication database. Available at: www.aviationmedicine.com/medication-database (accessed October 2015).
[18] Ferguson SA, Rajaratnam SM & Dawson D. Melatonin agonists and insomnia. Exp Rev Neurother 2010;10(2):305–318. doi:10.1586/ern.10.1
[19] Lemoine P, Nir T, Laudon M et al. Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. J Sleep Res 2007;16(4):372–380. doi:10.1111/j.1365-2869.2007.00613.x
[20] Lin GJ, Huang SH, Chen SJ et al. Modulation by melatonin of the pathogenesis of inflammatory autoimmune diseases. Int J Mol Sci 2013;14(6):11742–11766. doi:10.3390/ijms140611742
[21] Hindmarch I, Dawson J & Stanley N. A double-blind study in healthy volunteers to assess the effects on sleep of pregabalin compared with alprazolam and placebo. Sleep 2005;28(2):187–193. PMID: 16171242
[22] Morin CM, Koetter U, Bastien C et al. Valerian-hops combination and diphenhydramine for treating insomnia: a randomized placebo-controlled trial. Sleep 2005;28(11):1465–1471. PMID: 16335333
[23] Trenkwalder C, Winkelmann J, Inoue Y et al. Restless legs syndrome – current therapies and management of augmentation. Nat Rev Neurol 2015;11(8):434–445. doi:10.1038/nrneurol.2015.122
[24] Atmaca M. Drug-induced impulse control disorders: a review. Curr Clin Pharmacol 2014;9(1):70–74. doi:10.2174/1574884708666131111202954
[25] Voon V, Schoerling A, Wenzel S et al. Frequency of impulse control behaviours associated with dopaminergic therapy in restless legs syndrome. BMC Neurol 2011;11:117. doi:10.1186/1471-2377-11-117
[26] Garcia-Borreguero D. Dopaminergic augmentation in restless legs syndrome/Willis-Ekbom disease: identification and management. Sleep Med Clin 2015;10(3):287–292. doi:10.1016/j.jsmc.2015.05.020
[27] Garcia-Borreguero D, Kohnen R, Silber MH et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidelines: a report from the International Restles Legs Syndrome Study Group. Sleep Med 2013;14(7):675–684. doi:10.1016/j.sleep.2013.05.016
[28] Lauerma H & Markkula J. Treatment of restless legs syndrome with tramadol: an open study. J Clin Psychiatry 1999;60(4):241–244. doi:10.4088/jcp.v60n0407
[29] Saleto M, Anderer P, Saleto-Zyhlarz G et al. Restless legs syndrome (RLS) and periodic limb movement disorder (PLMD) acute placebo-controlled sleep laboratory studies with clonazepam. Eur Neuropsychopharmacol 2001;11(2):154–161. doi:10.1016/s0924-977x(01)00080-3
[30] National Institute for Health and Care Excellence (NICE). Continuous positive airways pressure for the treatment of obstructive sleep apnoea/hypopnoea syndrome. TA 139. 2008. Available at: https://www.nice.org.uk/guidance/ta139 (accessed September 2015).
[31] Mitchell RB. Adenotonsillectomy for obstructive sleep apnea in children: outcome evaluated by pre- and postoperative polysomnography. Laryngoscope 2007;117(10):1844–1854. doi:10.1097/mlg.0b013e318123ee56
[32] Duran-Cantolla J, Crovetto-Martinez R, Alkhraisat R et al. Efficacy of mandibular advancement device in the treatment of obstructive sleep apnea syndrome: a randomized controlled crossover trial. Med Oral Patol Oral Cir Bucal 2015;e605–e615. doi:10.4317/medoral.20649
[33] Billiard M, Bassetti C, Dauvilliers Y et al. EFNS guidelines on management of narcolepsy. Eur J Neuro l 2006;13(10):1035–1048. doi:10.1111/j.1468-1331.2006.01473.x
[34] Husein AM, Yancy WS Jr, Carwile ST et a l. Diet therapy for narcolepsy. Neurology 2004;62(12):2300–2302. doi:10.1212/wnl.62.12.2300
[35] Mignot EJ. A practical guide to the therapy of narcolepsy and hypersomnia syndromes. Neurotherapeutics 2012;9(4):739–752. doi:10.1007/s13311-012-0150-9
[36] Romberg RW, Needleman SB, Snyder JJ et al. Metamphetamine and amphetamine derived from the metabolism of selegiline. J Forensic Sci 1995;40(6):1100–1102. PMID: 8522918
[37] Inocente C, Arnulf I, Bastuji H et al. Pitolisant, an inverse agonist of the histamine H3 receptor: an alternative stimulant for narcolepsy-cataplexy in teenagers with refractory sleepiness. Clinical Neuropharmacology 2012;35(2):55–60. doi:10.1097/wnf.0b013e318246879d
[38] Dauvilliers Y, Bassetti C, Lammers GJ et al. Pitolisant versus placebo or modafinil in patients with narcolepsy: a double-blind, randomised trial. Lancet Neurol 2013;12(11):1068–1075. doi:10.1016/s1474-4422(13)70225-4
[39] Xyrem International Study Group. A double-blind, plaxcebo-controlled study demonstrated sodium oxybate is effective for the treatment of excessive daytime sleepiness in narcolepsy. J Clin Sleep Med 2005;1(4):391–397. PMID: 17564408
[40] Frey J & Darbonne C. Fluoxetine suppresses human cataplexy: a pilot study. Neurology 1994;44(4):707–709. doi:10.1212/wnl.44.4.707
[41] Wang J & Greenberg H. Status cataplecticus precipitated by abrupt withdrawal of venlafaxine. J Clin Sleep Med 2013;9(7):715–716. doi:10.5664/jcsm.2848
[42] Boscolo-Berto R, Viel G, Montagnese S et al. Narcolepsy and effectiveness of gamm-hydroxybutyrate (GHB): a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev 2012;16(5):431–443. doi:10.1016/j.smrv.2011.09.001
[43] Hulse G, Kelty E, Hood S et al. Novel indications for benzodiazepine antagonist flumazenil in GABA mediated pathological conditions of the central nervous system. Curr Pharm Des 2015;21(23):3325–3342. doi:10.2174/1381612821666150619092720
[44] Sommerauer M, Valko PO, Werth E et al. Excessive sleep need following traumatic brain injury: a case-control study of 36 patients. J Sleep Res 2013;22(6):634–639. doi:10.1111/jsr.12068
[45] Kumar R. Approved and investigational uses of modafinil: an evidence-based review. Drugs 2008;68(13):1803–1839. doi:10.2165/00003495-200868130-00003
[46] Schenck CH, Montplaisir JY, Frauscher B et al. Rapid eye movement sleep behaviour disorder: devising controlled active treatment studies for symptomatic and neuroprotective therapy – a consensus statement from the International Rapid Eye Movement Behavior Disorder Study Group. Sleep Med 2013;14(8):795–806. doi:10.1016/j.sleep.2013.02.016
[47] McGrane IR, Leung JG, St Louis EK et al. Melatonin therapy for REM sleep behaviour disorder: a critical review of evidence. Sleep Med 2015;16(1):19–26. doi:10.1016/j.sleep.2014.09.011
[48] Nash JR, Wilson SJ, Potokar JP et al. Mirtazepine induces REM sleep behaviour disorder (RBD) in parkinsonism. Neurology 2003;61(8):1161. PMID: 14581700
You might also be interested in…

Insomnia disorder: management strategies
Sleep disorders: diagnosis
