
Lawrence Lawry / Science Photo Library
Dentures are prosthetic appliances that replace lost teeth. There are two main types available — complete and partial dentures. A complete, or full, denture is one that replaces all the natural teeth in the upper, lower or both jaws (see Figure 1A). Some patients have a single complete denture opposing natural teeth, or natural teeth together with a partial denture. Partial dentures replace some teeth in a jaw, either the upper, lower or both, in which, typically, several teeth have been lost; they are supported by the remaining natural teeth and gums.
Complete dentures, including the teeth, tend to be all plastic (methyl methacrylate), although they can also be a combination of plastic and metal. Partial dentures, which may replace posterior and/or anterior teeth, typically include metal clasps that fit around natural abutment teeth, providing support to the lateral pressure to help retain the denture (see Figure 1B).
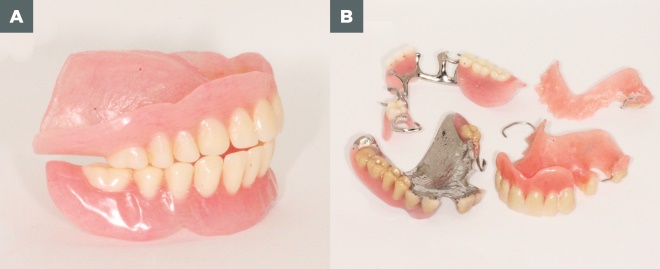
Figure 1: Types of dentures
Source: Courtesy of David R Radford
Two main types of denture appliances are available — complete and partial dentures. Panel A shows a complete, or full denture (one that replaces all the natural teeth in the upper, lower or both jaws). Panel B shows examples of partial dentures, which typically include metal clasps that fit around natural abutment teeth
In the UK, dentures may be provided, and when necessary, refurbished or repaired, by dentists or clinical dental technicians (CDTs).
Whatever their type, dentures are expected to remain stable, be comfortable and look good in function, including eating, drinking, talking and laughing. Given the contributions teeth make to facial appearance and attractiveness, these appliances can be of substantial importance to personal confidence and quality of life. Pharmacists, especially community pharmacists, are ideally placed to provide first-line advice and support for patients experiencing issues with their dentures, and should therefore be aware of the common problems patients experience, along with any products that may be beneficial in relieving these symptoms.
The aim of this article is to provide pharmacists and healthcare professionals with information on cleaning dentures, the common problems associated with wearing them, and to highlight when and where to refer patients.
Denture wearers
With general improvements in oral health, denture wearers in the UK tend to be older individuals and among the less affluent in society, many of whom may be socially deprived[1]
. Complete dentures are increasingly uncommon in the young and working-age population[2]
. At present, less than 6% of the population are edentulous, most of whom are over 65 years of age[1]
. In the 1968 Adult Dental Health Survey, 43% of all adults had 21 or more teeth extracted in a single procedure, prior to being provided with complete dentures[3]
.
Partial dentures are more common; at the turn of the 20th century, 30% of middle-aged and older adults wore them[4]
. No recent data are available on the percentage of the population who wear a partial denture; however, in 2011 they were worn by less than 40% of individuals aged 75 years and older[5]
. Some younger partial-denture wearers who engage in contact sports prefer to wear their dentures instead of using fixed replacements for their lost teeth[6]
.
Denture care
Cleaning
Just as with natural teeth, dentures accumulate food debris and dental plaque (see Figure 2) that should be removed at least once every 24 hours; however, this should preferably be done twice a day, including last thing at night. Failure to clean them may result in halitosis[7]
, the build-up of calculus (tartar) and stain on the surfaces of the denture and, in turn, irritation, if not infection, of the soft tissues on which the denture rests and, in the case of partial dentures, decay and gum disease of abutment or supporting teeth (Figure 2B).
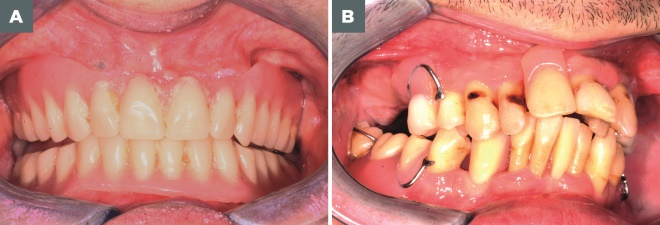
Figure 2: Denture care
Source: Courtesy of David R Radford
As with natural teeth, dentures accumulate food debris and dental plaque (A). Failure to clean them may result in the build-up of calculus (tartar) and stain on the surfaces of the denture and in the case of partial dentures, decay and gum disease of abutment or supporting teeth (B).
Pharmacists and healthcare professionals should remind patients that dentures must be removed from the mouth to achieve effective cleaning. There are two main methods to achieve this — brushing and immersion — although there is little evidence as to which is most effective[8]
. It is generally considered, however, that a combination of brushing and immersion may be found to be most satisfactory. Whatever method is selected, it should not involve the use of very hot water or powerful cleaning agents such as bleach, which damage denture plastic, causing loss of surface finish and crazing (the formation of surface cracks on the denture base resin). If dentures develop a build-up of recalcitrant stain and calculus, it is best that they are cleaned professionally.
Brushing
Denture brushes are often very coarse, stiff brushes with large heads. Their use is not recommended. Instead, pharmacists and pharmacy teams should recommend that medium-textured regular toothbrushes, including electric brushes for denture wearers with dexterity problems, are used. Patients should be advised to brush their dentures with soap and water or a cleaning paste — avoiding desensitising and abrasive smokers’ and whitening toothpastes. All surfaces of the denture, particularly the fitting surface, should be brushed. Care should be taken to avoid damaging any clasps or other parts of partial dentures. Brushing and subsequent rinsing under running water should be conducted over a basin partially filled with water, to avoid breakages if the denture is dropped.
Immersion
Following thorough brushing and rinsing, soaking or immersing dentures in a proprietary solution, usually sold ready for use or formed by dissolving a tablet or powder in water, can be effective. In these cases, the manufacturer’s directions for use must be followed correctly. Immersing them can enhance hygiene and provide additional mouth freshness. Partial dentures with metallic components (see Figure 1B) may not be suitable for immersion cleaning, as certain metal alloys used in partial denture construction may be corroded by cleaning agents. Pharmacists should check with patients the type of appliance they have before making recommendations on proprietary denture cleaners.
Although often difficult to do when out and about, patients’ dentures and mouths should be rinsed after meals. This flushes away food debris, especially debris that may become trapped between the fitting surface of the denture and the underlying soft tissues. This can make a substantial difference to mouth and denture freshness, and oral comfort, and help limit the negative effects of denture wearing (e.g. tissue irritation and trauma, inflammation and infection and, in the case of partial dentures, an increased risk of abutment teeth developing dental caries and periodontal disease).
Replacing dentures
Dentures suffer wear and tear during use and the mouth, including any remaining teeth, undergoes many physiological and pathological changes over time. Therefore, these appliances should be replaced, or at least refurbished, every few years (up to five years). Pharmacists and other healthcare professionals should recommend that denture wearers, including edentulous patients, see their dentist on a yearly basis for an oral health assessment or routine check-up. Dentures, especially complete ones, can become like old slippers in that there is not a specific problem, but look increasingly unsightly and become inefficient over time, resulting in an unnecessary reduction in quality of life.
Pattern of wearing
Pharmacists and healthcare professionals should advise patients to leave their dentures out overnight, but also that they should be kept moist to avoid dehydration, which may damage them. This does not necessitate placing them in a glass of water on the bedside table; appliances may be kept overnight in a denture box or other receptacle, as long as they are carefully cleaned before being stored and not allowed to dry out. If denture wearers are embarrassed, or suffer any difficulties; for example, temporomandibular joint discomfort by removing their dentures overnight, typically they will come to no harm if they have well-fitting dentures and are performing denture cleaning and maintaining oral hygiene to a consistent high standard.
Fixatives and liners
Denture fixatives (adhesives) and liners, sometime referred to as ‘cushions’, and related products may be referred to collectively as denture comfort products. The evidence base for the use and problems associated with these products is limited; the data are old and of little, if any, relevance to present-day fixatives and liners.
Fixatives
Denture fixatives are intended to enhance the retention and stability of dentures. While well-fitting appliances should be sufficiently retentive and stable, wearers may use a fixative to increase confidence in their denture. Clinical experience indicates that users of denture fixatives have dentures that no longer fit their mouth and lack retention and stability. With ongoing resorption and remodelling of edentulous jaws, the frequency and extent of use of denture adhesives may increase, with patients in such circumstances possibly returning to the pharmacy complaining that the adhesive is not working as intended. Alternatively, such patients may turn to other denture ‘comfort’ products.
Denture fixatives are more effective under upper dentures because saliva tends to wash away fixatives under lower dentures. Patients with poor denture hygiene may not only be disappointed with the effectiveness of denture adhesives — plaque and other deposits on poorly maintained dentures interferes with the action of the adhesive — but they may also experience high levels of denture-related oral and dental disease because fixatives, some of which can be tenacious, collect food debris and cause plaque accumulation in close proximity to the oral tissues.
Liners
Denture liners are intended to fill gaps between the underlying gum and ill-fitting appliances, typically caused by gum resorption and remodelling[9]
. Liners may be used to provide a ‘cushion’ between the hard-fitting surface of a denture and sensitive, traumatised (ulcerated) or infected denture-bearing soft tissues. Liners are not suitable for use with metal-based dentures or so-called ‘flexible dentures’ made of nylon.
Liners, most of which are marketed for use over extended periods, come in powder–liquid or sheet forms to be applied to the fitting surface of the denture. Even with good directions for use, it is all too easy to make errors in the application of denture liners, possibly resulting in damage to the denture or, more importantly, adverse effects to the denture-bearing tissues and abutment teeth for partial dentures.
If a patient wishes to resolve substantial difficulties with dentures, or is making repeat purchases of denture liners, complaining that they are not very effective, or effective for a short period of time only, then pharmacists and healthcare professionals should refer them to a dentist or CDT.
Lining materials, which tend to be more porous and liable to deterioration in clinical use than denture base materials of plastic or metal, may become stained and add to denture odour and other difficulties. Typically, if patients feel the need to use a liner, pharmacists and pharmacy teams should recommend that they seek professional help.
Common problems associated with denture use
Denture ulcers and stomatitis
Dentures commonly give rise to ulcers and denture-related stomatitis[10]
. Patients complaining of ulcers caused by newly supplied dentures should be advised to revisit their dentist or the CDT who provided the appliance, as these are typically the result a production error that can be corrected. Giving appliances time to ‘bed-in’, with or without the use of some form of mouth ulcer ointment or gel, is not recommended.
Sore spots and ulcers typically have some physical causation, either on the surface of the appliance or related to the way the denture teeth meet in function – the occlusion of the dentures. Pharmacists can advise patients, while arranging or waiting for professional care, to leave the appliance out as much as possible and to use a mouth ulcer medication or gel to manage acute symptoms.
Patients who have ulcers and other oral lesions caused, or thought to be caused, by dentures that have been successfully worn for some time, should be referred to their dentist. Patients with ulcers that have persisted for more than two weeks should be referred to a dentist for urgent assessment to preclude the possibility of oral cancer.
Denture-related stomatitis, the presence of red inflamed tissue, is normally associated with upper dentures and is limited to the denture-bearing area (see Figure 3). Typically, denture-related stomatitis (chronic atrophic candidiasis) is caused by poor oral hygiene, which may be exacerbated by an ill-fitting appliance[9]
. Patients with this condition should be referred to a dentist. Management may include the prescription of an antifungal if the presence of Candida albicans is suspected.

Source: Courtesy of David R Radford
Denture-related stomatitis, the presence of red inflamed tissue, is normally associated with upper dentures and is limited to the denture-bearing area.
Rarely, acutely inflamed tissues under a new denture may be the result of an allergic reaction to the appliance’s base material. Alternatively, acutely inflamed tissue under an appliance may be an adverse reaction to residual denture cleaner, adhesive or other material applied to the denture. In such circumstances, a referral to a dentist is indicated. In the short term, pharmacists and healthcare professionals should advise the patient to leave the appliance out as much as possible and, if not already doing so, take extra time and care to clean the appliance before and after placement in the mouth — brushing with just soap and water, avoiding any cleaning agent which may be the cause of the tissue reaction.
In all cases, denture wearers should be discouraged from attempting to adjust an appliance themselves, as inappropriate modifications may necessitate remaking the denture.
Denture odour and denture halitosis
Typically the result of poor denture and oral hygiene, denture odour and halitosis may be associated with a combination of tobacco use, excessive consumption of certain foods and beverages, mouth breathing and dry mouth[7]
. Occasionally, halitosis is wrongly attributed to these appliances, being associated with ear nose and throat, gastroenterological, or bronchial and pulmonary pathologies, or with systemic diseases (e.g. diabetes), metabolic or hormonal change, and hepatic or renal insufficiency[7]
. If patients ask for advice on the management of denture odour or denture halitosis, pharmacists and healthcare professionals should think first about promoting basic denture and oral hygiene practices.
Loose dentures
If new dentures are loose, pharmacists and pharmacy teams should advise patients to go back to the dentist or CDT who provided the appliance. Dentures that have become loose after several years of use probably need to be professionally relined or replaced. The use of an adhesive may help retain and stabilise and, in the process, enhance the patient’s confidence in the loose denture, while arranging and waiting for professional help.
Persistent angular cheilitis
Persistent angular cheilitis in denture wearers (see Figure 4) is typically associated with poor support of the lips, specifically the upper lip, or a very reduced occlusal vertical dimension — the appliance does not restore face height. With these conditions, saliva seeps from the corners of the mouth, causing the commissures of the lip to become ‘soggy’, encouraging the overgrowth of Staphylococcus aureus
[11]
. This painful, often embarrassing, condition is typically best managed by the replacement of dentures that are no longer fit for purpose. Pharmacists, healthcare professionals and pharmacy teams can look for signs, and question and counsel patients accordingly.

Source: Courtesy of David R Radford
In persistent angular cheilitis, saliva seeps from the corners of the mouth, causing the commissures of the lip to become ‘soggy’, encouraging the overgrowth of Staphylococcus aureus.
Problem patients
The day-to-day comfort and acceptance and, in turn, function of dentures is greatly enhanced by effective, daily cleaning and associated care by the wearer, or (if applicable) their care provider.
Despite expert care, some patients will always have difficulties with these appliances. As may be appreciated from Figure 1, dentures, in the eyes of some patients, are large foreign bodies in a very emotionally charged and sensitive part of the body. Therefore, if a patient is experiencing multiple difficulties with first-time dentures, it may be the inability of the patient to adapt to prostheses and manage a significant disability that increasingly has a social taboo, that is causing the problem.
Patients can often be quite distressed and, in their anxiety, very demanding. In such circumstances, pharmacists and healthcare professionals should advise them to return to the dental care professional who provided the appliance, even if they have lost confidence in that person’s ability to address the problem[12]
.
Patients who resort to the use of adhesives and liners, and products to help manage oral lesions — especially regular users of such products — may greatly benefit from referral to a dentist, with the possibility of substantial improvements in quality of life.
Useful resources
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Department of Health, England. Adult Dental Health Survey 2009: executive summary. Available at: http://content.digital.nhs.uk/catalogue/PUB01086/adul-dent-heal-surv-summ-them-exec-2009-rep2.pdf (accessed January 2018)
[2] Steele JG, Treasure ET, O’Sullivan I et al. Adult Dental Health Survey 2009: transformations in British oral health 1968–2009. Br Dent J 2012;213:523–527. doi: 10.1038/sj.bdj.2012.1067
[3] Gray PG, Todd JE, Slack GL et al. Adult dental health in England and Wales in 1968. London, HMSO 1970. doi: 10.1038/sj.bdj.4802531
[4] Kelly M, Steele JG, Nuttal N et al. Adult Dental Health Survey. Oral health in the United Kingdom 1998; London:The Stationery Office 2000.
[5] Steele J, Treasure E, Fuller F et al. Complexity and maintenance: a report from the Adult Dental Health Survey 2009, London, The Health and Social Care Information Centre.
[6] Singhal A & Gorg R. Sports dentistry: a review. Head Talk 2014;6:40–41. Available at: http://oaji.net/articles/2014/1143-1412843748.pdf (accessed January 2018)
[7] Wilson NHF & Winkel EG. Advising patients on halitosis and oral hygiene. Pharm J 2017;298(7900):online. doi: 10.1211/PJ.2017.20202477
[8] Nikawa H, Hamada T, Yamashiro Het al. A review of in vitro and in vivo methods to evaluate the efficacy of denture cleansers. Int J Prosthodont 1999;12:153–157. PMID: 10371918
[9] Pietrokovski J & Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent 1967;17:21-27. PMID: 5224784
[10] Radford DR, Challacombe SJ & Walter JD. Denture plaque and adherence of Candida albicans to denture-base materials in vivo and in vitro. Crit Rev Oral Biol Med 1999;10:99–116. PMID: 10759429
[11] Coulthwaite L & Verran J. Potential pathogenic aspects of denture plaque. Br J Biomedical Sci 2007;64: 180–189. PMID: 18236742
[12] Davis DM, Fiske J, Scott B et al. The emotional effects of tooth loss: a preliminary quantitative study. Brit Dent J 2000;18:503–507. PMID: 10859849


