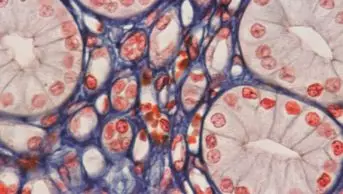
Mehau Kulyk / Science Photo Library
Vasculitis is a disparate collection of rare diseases characterised by the inflammation of blood-vessel walls. It can cause damage to a range of different organs and tissues, leading to a wide variety of clinical manifestations according to the part of the vascular tree affected. It can be primary and autoimmune in nature or secondary to infection, medicines or malignancy.
The most prevalent autoimmune vasculitis is the sub-group associated with antineutrophil cytoplasmic antibodies (ANCAs), which predominantly affects small and medium-sized blood vessels in the body. Although rare, ANCA-associated vasculitis must be diagnosed and treated early as otherwise it can progress rapidly to organ failure and death. Patients may present with a diverse range of symptoms, from acute presentation with rapidly progressive kidney disease and pulmonary haemorrhage, to more indolent nasal or hearing problems.
ANCAs are pathogenic antibodies that bind to enzymes on the surface of neutrophils, activating them and causing them to attach to blood-vessel walls and release cytolytic enzymes. These enzymes cause inflammation and damage to the blood-vessel wall. Levels of ANCA in the body can be a helpful indicator of disease activity, but must be interpreted in relation to the clinical situation, so treatment should not be started on the basis of ANCA titres alone[1]
.
ANCA-associated vasculitis (AAV) is more common in patients of Caucasian ethnicity and older adults. It has a peak age of onset of 65–74 years and an annual incidence of 20 cases per million population[2]
. The cause of AAV is unknown, but it is thought there is a genetic predisposition followed by environmental triggers (e.g. viral illness) which ‘primes’ neutrophils. There have also been reports of drug-induced AAV associated with hydralazine, propylthiouracil and penicillamine.
Types of ANCA-associated vasculitis
There are three syndromes in AAV, all of which are characterised by necrotising inflammation of blood vessels[3]
:
- Microscopic polyangiitis (MPA) usually affects arterioles in the kidneys (causing glomerulonephritis) and the lungs (causing alveolitis and pulmonary haemorrhage). Inflammation is confined to the blood vessels.
- Granulomatosis with polyangiitis (GPA; formerly Wegener’s granulomatosis) has much in common with MPA. It also affects the kidneys and lungs, but is characterised by extravascular necrotising granulomatous inflammation in the upper and lower airways and other organs.
- Eosinophilic granulomatosis with polyangiitis (EGPA; formerly Churg-Strauss syndrome) is an eosinophil-rich necrotising inflammation that affects the airways associated with asthma; nasal polyps are common. When EGPA is associated with ANCAs it can cause glomerulonephritis. The heart, gut and nerves are also commonly affected.
Patients with AAV can experience generalised symptoms of inflammation, such as fever, malaise, weight loss, and muscle and joint pain; these non-specific symptoms often lead to delayed diagnosis. Skin may be affected by dermal venulitis, which causes a purpuric rash on the lower extremities.
The kidneys are often affected — in 90% of patients with microscopic polyangiitis (MPA), 80% of patients with granulomatosis with polyangiitis (GPA), and 45% of patients with eosinophilic granulomatosis with polyangiitis (EGPA)[4]
— causing rapidly progressing glomerulonephritis. Almost any system may be affected by AAV, but the most frequent, alongside kidney and lung, include the eyes, gut and peripheral nervous system. Disease activity can be formally assessed using the Birmingham Vasculitis Activity Score (BVAS).
Pulmonary involvement commonly manifests as necrotising granulomatous inflammation in GPA. Upper respiratory symptoms are extremely common in GPA (affecting 90% of patients) and EGPA (70% of patients), and include subglottic stenosis (narrowing of the airway), sinusitis and rhinitis. Necrotising granulomatous inflammation in GPA and EGPA can cause destruction of bone and a characterising ‘saddle nose’ deformity.
Aggressive treatment has resulted in remission rates of 90%. The main challenges of care are managing chronic damage from the disease and treatment toxicity. The risk of treatment-related morbidity increases with time and can include cardiovascular disease, diabetes, osteoporosis and malignancy[5]
[6]
.
Mortality is highest during the first year after diagnosis, during which infection is the main cause of mortality. Cardiovascular disease and cancers become more prevalent after the first year[7]
. Between 20% and 40% of patients with AAV are dialysis-dependent within three to five years. High serum creatinine at the time of diagnosis usually leads to poorer outcomes[8]
. For many patients, fatigue reduces quality of life significantly[9]
.
There is no cure for AAV, so the aim of treatment is to achieve and maintain remission (defined as absence of disease activity). According to the British Society for Rheumatology (BSR) and the European League Against Rheumatism (EULAR), there are five essential principles of treatment[10]
:
- Rapid diagnosis;
- Rapid initiation of treatment;
- Early induction of remission to prevent organ damage;
- Maintenance of remission with the aim of eventual treatment withdrawal;
- Prevention of drug toxicity.
Aggressive treatment of AAV (induction therapy) at diagnosis can improve relapse-free survival and minimise long-term damage. The BSR recommends that all newly diagnosed patients considered to have potentially life-threatening disease should be assessed for disease activity with a view to starting induction therapy with cyclophosphamide or rituximab[10]
. Treatment decisions should be made by a specialist.
Close monitoring for adverse effects is required for all vasculitis treatments. As there is a high risk of infection, careful consideration must be given to screening for infections (including tuberculosis) before starting immunosuppressive therapy. Patients should also be advised to have influenza and pneumococcal vaccinations. After therapy has started, urea and electrolytes, full blood count and liver function tests should be checked regularly, usually every one to two weeks initially, although this is dependent on type and intensity of therapy.
All patients receiving induction therapies should be given the oral antibiotic co-trimoxazole as prophylaxis against Pneumocystis jirovecii pneumonia (dapsone, atovaquone or nebulised pentamidine can be used if contraindicated), and the antifungal fluconazole should be considered to minimise the risk of oral and invasive candidiasis.
Prophylaxis against steroid-induced osteoporosis should also be offered according to national guidelines.
Induction therapies
Corticosteroids are used to reduce the initial inflammatory response associated with severe disease in all types of AAV. Patients with rapidly progressing disease will usually be given a course of pulsed methylprednisolone (500mg to 1g daily for three days) when waiting for further blood tests or a kidney biopsy to be performed. This is followed by a course of oral prednisolone (1mg/kg/day, capped at 80mg) in combination with cyclophosphamide or rituximab. The dose of prednisolone is then tapered slowly over several months to a maintenance dose of <10mg a day. Ideally, patients should stop taking prednisolone completely, but this is not usually advisable in the first 12 months because of the risk of relapse.
Cyclophosphamide is an alkylating agent. It alkylates guanidine nucleotides, thereby blocking cell division. The exact mechanism of cyclophosphamide in vasculitis is poorly understood, but it is thought to have cytotoxic effects on neutrophils and lymphocytes[11]
.
Cyclophosphamide induces remission in around 90% of patients with AAV[6]
, but it can cause significant toxicity, including infertility, bone-marrow suppression and haemorrhagic cystitis. The risk of infertility and cancer is cumulative with each dose, and a patient’s lifetime exposure to cyclophosphamide should be capped at a maximum of 25g[10]
. Pharmacists should be sure that previous exposure to cyclophosphamide is within acceptable limits when clinically checking prescriptions.
Restricting course length and administering the drug intravenously in intermittent pulses can limit exposure to cyclophosphamide and minimise toxicity. A meta-analysis of studies investigating the value of intravenous pulse therapy in vasculitis showed it to be more effective than daily oral therapy while causing less infection and leucopenia[12]
.
Current BSR guidelines are based on the CYCLOPS trial protocol for cyclophosphamide: 15mg/kg intravenously in pulses (adjusted for renal impairment and age), starting with one dose every two weeks for three doses; then one dose every three weeks for three to six months[10]
. The CYCLOPS trial found no difference in time to remission with intravenous pulsed cyclophosphamide compared with continuous oral therapy[11]
. A longer-term follow-up of this study (median follow-up 4.3 years) found an increased relapse rate in the intravenous pulse therapy arm, but no difference in renal function between groups. The benefits of using a lower cumulative dose mean most units will have continued to adopt protocols involving intravenous pulse therapy.
Patients should be counselled on the possibility of infertility prior to the administration of cyclophosphamide. If feasible, patients should be offered the opportunity to use a sperm bank and oocyte cryopreservation (for men and pre-menopausal women, respectively).
Mesna is used to prevent haemorrhagic cystitis caused by acrolein, a metabolite of cyclophosphamide. Mesna binds to acrolein to form a non-toxic compound6 and is administered in three doses before and then two and six hours after intravenous cyclophosphamide. The dose of mesna administered is a percentage of the cyclophosphamide dose: 20% if given intravenously or 40% if given orally. Mesna is usually well tolerated but can cause nausea and, rarely, allergic reactions in patients allergic to thiol compounds.
Rituximab is a genetically engineered chimaeric (mouse–human) monoclonal antibody that depletes B lymphocytes, thereby reducing the production of antibodies. It was originally licensed for the treatment of non-Hodgkin’s lymphoma but has been used off-label for autoimmune diseases for many years and was licensed for induction of remission in GPA and MPA (see ‘Types of ANCA-associated vasculitis’) in 2013 by the European Medicines Agency for use in the European Union.
The RAVE and RITUXVAS trials found that rituximab was non-inferior to cyclophosphamide, and there were no significant differences in side effect profiles. The BSR suggests that rituximab is preferable in situations where the use of cyclophosphamide is undesirable[10]
.
The National Institute for Health and Care Excellence (NICE) recommends rituximab for the following situations[13]
:
- When further cyclophosphamide treatment would exceed the maximum cumulative dose permitted (25g total lifetime dose);
- If cyclophosphamide is contraindicated or not tolerated;
- If a patient wishes to preserve his or her fertility to have children;
- When the disease has remained active or has progressed, despite a course of cyclophosphamide lasting between three and six months;
- If the patient has a history of uroepithelial malignancy.
In January 2015, NHS England updated its commissioning advice to allow the use of rituximab in patients who experience a relapse, to reflect that rituximab has been shown to be more effective than cyclophosphamide in patients with relapsing disease.
The licensed dose of rituximab for AAV is 375mg/m2 by intravenous infusion weekly for four weeks. Although not licensed for AAV, a two 1g dose regimen taken two weeks apart has been shown to deplete B cells for the same length of time, and may be more convenient for patients attending day case units for administration.
Infusion reactions are common and patients should be given chlorphenamine, paracetamol and corticosteroids before treatment. The recommended initial rate for infusion is 50mg/hour, increasing every 30 minutes in increments of 50mg/hour to a maximum of 400mg/hour. Subsequent doses can be infused at an initial rate of 100mg/hour, and increased by 100mg/hour increments at 30-minute intervals, again to a maximum of 400mg/hour.
Mild reactions, such as headache or itching, usually respond to interrupting the infusion or reducing the infusion rate. Reactions such as anaphylaxis, which are severe enough to warrant permanent discontinuation of treatment, are rare. Patients should be prescribed antihistamines and additional corticosteroids as required, so nursing staff should be able to administer these urgently if required.
All patients starting rituximab therapy should be issued with a patient alert card that contains information about the risk of progressive multifocal leukoencephalopathy (PML), which is a rare, progressive demyelinating disease of the central nervous system and can cause death or severe disability. PML has been reported in six patients with AAV, none of whom were treated with rituximab[14]
. However, PML has been reported in patients treated with rituximab for other autoimmune disorders. Patients who have received rituximab are advised to report any symptoms of memory loss, vision loss, difficulty walking or trouble thinking.
A course of rituximab costs between £4,000 and £6,000. Although this may seem expensive, for patients with severe kidney disease this cost is easily offset by the potential for avoiding dialysis.
Rituximab has been associated with reactivation of hepatitis B, and patients should be screened for the virus before treatment begins[15]
.
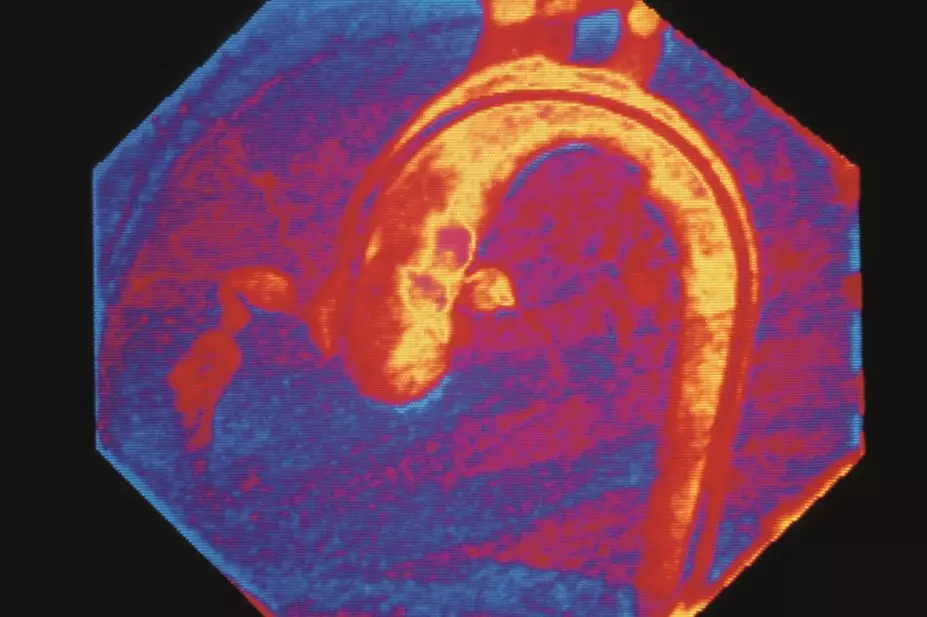
Plasma exchange (PEX) may be appropriate for patients presenting with severe kidney disease or with other life-threatening complications, such as pulmonary haemorrhage. In PEX, the patient’s blood is anticoagulated and passed through a centrifuge or filter to separate plasma from blood cells. The plasma fraction containing large-molecular-weight substances (for example, including inflammatory mediators and antibodies, including pathogenic ANCAs) is discarded, and the red and white blood cells are returned to the patient. Plasma is replaced with the same volume of human albumin solution, as well as clotting factors in the form of fresh frozen plasma (FFP).
The main side effects of PEX include bleeding owing to heparin administration and depletion of clotting factors, and hypocalcaemia, owing to chelation with citrate present in FFP. Hypocalcaemia can be minimised by running a calcium gluconate infusion during the plasma exchange procedure.
Another important consideration is that PEX will also remove medicines including rituximab and cyclophosphamide, so the maximum possible time (ideally seven days) should be allowed between administration of a patient’s medicines and a PEX session[16]
.
The MEPEX study compared PEX with 3,000mg intravenous methylprednisolone in patients with severe kidney disease (serum creatinine >500μmol/l). Both treatment groups were also prescribed oral cyclophosphamide and prednisolone. At three months, 69% of patients using PEX were alive and independent of dialysis, compared with 49% taking methylprednisolone[17]
. Although PEX seemed to show a reduction in progression to end-stage renal failure in the short-term, a follow-up study showed no statistically significant difference in deaths or progression to end-stage renal failure after a median follow-up of four years. There was a high rate of infection in both groups, which may have been related to the aggressive immunosuppression regimen. Infections were also higher in the PEX group, which may be related to the invasive nature of the treatment in addition to gammaglobulin depletion.
It is still unclear whether patients with less severe renal impairment at presentation benefit from plasma exchange, but the PEXIVAS study is currently recruiting and will assess whether lower steroid doses are possible, and whether patients with less severe renal impairment benefit from PEX[18]
.
Maintenance and relapse
Patients who enter remission receive maintenance treatment for at least 12 months. Relapse is common, with 50% of patients relapsing within five years. Although very effective, cyclophosphamide is associated with significant toxicities and is not used for long-term therapy.
Azathioprine can be used as a maintenance option. It should be started at 2mg/kg/day, rounded to the nearest 25mg tablet. The patient should have a weekly full blood count and liver function test for six weeks, then every two weeks until the dose is stable for six weeks, then monthly. Monitoring may be reduced to every three months if the patient is stabilised on a maintenance dose.
Azathioprine is contraindicated in patients taking allopurinol, a xanthine oxidase inhibitor, as the interaction causes accumulation of 6-mercaptopurine and bone-marrow toxicity.
The role of azathioprine has been reinforced by the IMPROVE study. This aimed to show mycophenolate mofetil was superior to azathioprine for maintenance of remission in vasculitis; however, it found relapses were more common in the mycophenolate mofetil group with an unadjusted hazard ratio (HR) of 1.69 (95% confidence interval [CI], 1.06–2.70; P =0.03)[19]
.
Rituximab has also been assessed as a maintenance agent in the MAINRITSAN study[20]
. After induction with cyclophosphamide and prednisolone, patients were randomised to rituximab (two 500mg doses two weeks apart every six months) or azathioprine 2mg/kg/day (reduced to 1.5mg/kg/day at 12 months and 1mg/kg/day at 18 months). After 28 months, there was a reduction in the primary end-point of major relapse in the rituximab group of 5% compared with 29% in the azathioprine group (HR for relapse 6.61; 95% CI, 1.56–27.96; P=0.002). However, it is not possible to determine the efficacy of azathioprine had doses been maintained throughout the study period.
Marc Vincent DipClin, MRPharmS, IPresc is lead pharmacist for adult renal services and Nina Brown MBChB BSc(Hons) is specialty registrar in nephrology, both at Central Manchester Hospitals NHS Foundation Trust.
References
[1] Vincent M. Introduction to Renal Therapeutics. 1st ed. Ashley C, editor. London: Pharmaceutical Press; 2008.
[2] Ntatsaki E, Watts RA & Scott DG. Epidemiology of ANCA-associated vasculitis. Rheum. Dis. Clin. North Am. 2010;36(3):447–461.
[3] Jennette JC, Falk RJ, Bacon PA et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1–11.
[4] Floege J, Johnson RJ & Feehally J. Comprehensive Clinical Nephrology 4th Ed. Elsevier: St Louis 2010.
[5] Robson J, Doll H, Suppiah R et al. Damage in the anca-associated vasculitides: long-term data from the European Vasculitis Study group (EUVAS) therapeutic trials. Ann. Rheum. Dis. 2015;74(1):177–184.
[6] Richmond R, Mcmillan TW & Luqmani RA. Optimisation of cyclophosphamide therapy in systemic vasculitis. Clin. Pharmacokinet. 1998;34(1):79–90.
[7] Flossmann O, Berden A, de Groot K et al. Long-term patient survival in ANCA-associated vasculitis. Ann. Rheum. Dis. 2011;70(3):488–494.
[8] Walsh M, Casian A, Flossmann O et al. Long-term follow-up of patients with severe ANCA-associated vasculitis comparing plasma exchange to intravenous methylprednisolone treatment is unclear. Kidney Int. 2013;84(2):397–402.
[9] Basu N, Jones GT, Fluck N et al. Fatigue: a principal contributor to impaired quality of life in ANCA-associated vasculitis. Rheumatology (Oxford). 2010;49(7):1383–1390.
[10] Ntatsaki E, Carruthers D, Chakravarty K et al. BSR and BHPR guideline for the management of adults with ANCA-associated vasculitis. Rheumatology (Oxford) 2014;1–4. doi: 10.1093/rheumatology/ket445.
[11] Harper L, Morgan MD, Walsh M et al. Pulse versus daily oral cyclophosphamide for induction of remission in ANCA-associated vasculitis: long-term follow-up. Ann. Rheum. Dis. 2012;71(6):955–960.
[12] de Groot K, Adu D & Savage CO. The value of pulse cyclophosphamide in ANCA-associated vasculitis: meta-analysis and critical review. Nephrol. Dial. Transplant. 2001;16(10):2018–2027.
[13] National Institute for Health and Care Excellence. Rituximab in combination with glucocorticoids for treating anti-neutrophil cytoplasmic antibody-associated vasculitis. NICE Technology Appraisal Guidance 308 2014;(March):145–162.
[14] Pugnet G, Pagnoux C, Bézanahary H et al. Progressive multifocal encephalopathy after cyclophosphamide in granulomatosis with polyangiitis (Wegener) patients: case report and review of literature. Clin. Exp. Rheumatol. 31(1 Suppl 75):S62–S64.
[15] Medicines and Healthcare Products Regulatory Agency. Rituximab: screen for hepatitis B virus before treatment. Drug Safety Update. 2013.
[16] Puisset F, White-Koning M, Kamar N et al. Population pharmacokinetics of rituximab with or without plasmapheresis in kidney patients with antibody-mediated disease. Br. J. Clin. Pharmacol. 2013;76(5):734–740.
[17] Jayne DR, Gaskin G, Rasmussen N et al. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J. Am. Soc. Nephrol. 2007;18(7):2180–2188.
[18] Walsh M, Merkel PA, Peh CA et al. Plasma exchange and glucocorticoid dosing in the treatment of anti-neutrophil cytoplasm antibody associated vasculitis (PEXIVAS): protocol for a randomized controlled trial. Trials 2013;14:73.
[19] Hiemstra TF, Walsh M, Mahr A et al. Mycophenolate mofetil vs azathioprine for remission maintenance in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled trial. JAMA 2010;304(21):2381–2388.
[20] Guillevin C, Pagnoux A, Karras C et al. Rituximab versus Azathioprine for Maintenance in ANCA-Associated Vasculitis. N Engl J Med 2010;371:2373–2383.
You might also be interested in…

Dialysis: principles and treatment options

Dialysis: management