
clubtable / Wikimedia Commons
A limited number of mechanisms can cause a diseased state in the eye; these can be categorised as disorders of the eyeball or of the eyelids. However, common symptoms to look for include alteration in visual acuity, redness, pain, discharge and photophobia. Figures 1 and 2 show diagrammatic representations of the eye.
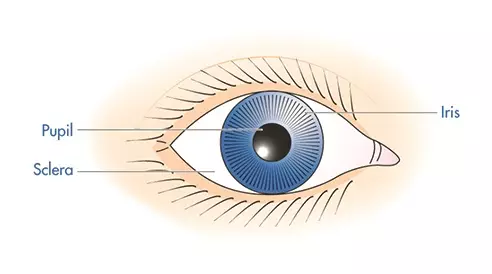
Figure 1: Anterior view of the eye
Source: Pharmaceutical Press
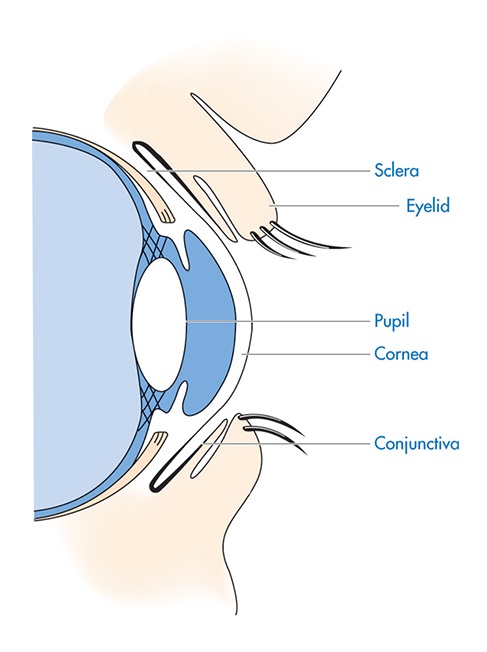
Figure 2: Horizontal cross-section of the anterior eye
Source: Pharmaceutical Press
Three situations that are relatively easy to recognise, usually present no immediate danger, and, in most cases, can be treated symptomatically in the first instance, are:
- Painless red eye;
- Disorder of tear formation;
- Inflammation of the eyelids.
Painless red eye
Conjunctivitis is the most common cause of red eye and is an inflammation of the conjunctiva of the anterior eye. The conjunctiva is a thin vascular membrane that covers the anterior surface of the eyeball and folds back on itself to form the lining of the eyelid. In wearers of contact lenses, conjunctivitis can be caused by a scratched cornea, a reaction to a lens solution, a poorly fitting lens or corneal drying.
Conjunctivitis commonly affects both eyes, although one may be affected more than the other. If both eyes are affected, and in the absence of any warning signs or symptoms, the conjunctivitis will probably have either an allergic or an infective cause.
In both allergic and infective conjunctivitis, the white (sclera) of the eye is red, and this redness extends to the inner surface of the eyelids (Figure 3). Pulling down the lower lid will reveal a red and oedematous conjunctiva covering its inner surface, while pale pink is seen in a normal eye. The sufferer will usually complain of an itchiness or grittiness on the surface of the eye.
The commonest cause of allergic conjunctivitis is hay fever and is often seen in young people, in whom any allergic predispositions are more evident. Hay fever is more commonly seen in women than men, and is often caused by eye cosmetics, although soaps, cleansers and powders applied to the face can also provoke a reaction. In allergic conjunctivitis, there is usually a clear watery discharge in addition to an itchy or gritty sensation on the surface of the eye.
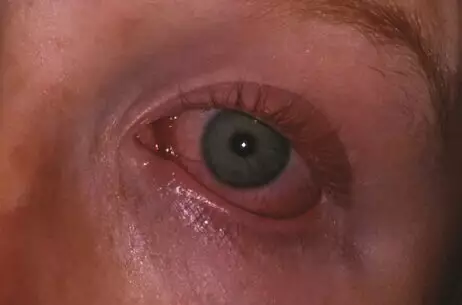
Figure 3: Conjunctivitis
Source: Cdale0112 / Wikimedia Commons
Conjunctivitis is the most common cause of red eye and is an inflammation of the conjunctiva of the anterior eye.
In infective conjunctivitis, there is usually a discharge that may be purulent in bacterial conjunctivitis but clear and watery in viral conjunctivitis. The exact percentage of infections that are bacterial or viral is not clear, and it has been estimated that somewhere between 33% and 78% of infective conjunctivitis cases are bacterial in origin. The most common bacterial cause is Staphylococcus aureus. A discharge of pus that collects in the inner corner of the eye or that prevents easy opening of the eyelids on awakening is a sign of bacterial conjunctivitis. This may be unilateral but usually affects both eyes. It can be clinically difficult to distinguish between bacterial and viral conjunctivitis, because, although the symptoms and signs are described differently in textbooks, there is often confusion clinically.
A unilateral red eye is more likely to be related to a condition within the eye, such as iritis or glaucoma. Iritis is an inflammation of the iris. Associated structures, such as the ciliary body, are often involved (iridocyclitis). The condition may be caused by infection or allergy, or may be the result of systemic disease. Symptoms include pain within the eye, photophobia, visual impairment, and hazy, small, irregularly shaped and unreactive pupils. Iritis may progress to cause cataracts (if the lens is involved) or glaucoma (if the angle at the edge of the ciliary body is eliminated). There is a danger of permanent visual loss unless diagnosis and treatment take place at an early stage.
In such cases, the redness typically occurs more around the centre of the eye, close to the iris, and is largely absent from inside the lids, compared with the more peripheral redness of an allergy or infection. However, it is often difficult to distinguish the conditions on this basis.
A subconjunctival haemorrhage (caused by a burst blood vessel) appears as a red spot or may cover the white of the eye (Figure 4). Although the condition can provoke anxiety in the sufferer, it is harmless and will heal spontaneously without treatment within a few weeks if no accompanying symptoms are present.

Figure 4: Subconjunctival haemorrhage
Source: James Heilman / Wikimedia Commons
A subconjunctival haemorrhage (caused by a burst blood vessel) appears as a red spot or may cover the white of the eye.
Disorders of tear formation
People who complain of dry eyes may require artificial tears (as eye drops). This condition is seen as a complication of certain disorders, such as rheumatoid arthritis (Sjögren’s syndrome), and in oestrogen deficiency, as occurs in menopausal women. It is wise to refer people with dry eyes to eliminate corneal ulceration or any other pathology.
Inflammation of eyelids
Inflammation of the margin of one eyelid is likely to be caused by a small abscess or stye, which is an infection of a hair follicle gland at the base of an eyelash (Figure 5). The infection can cause redness and irritation around the affected area with possible progression to pain and swelling of the eyelid. Styes are common and often recurrent; the inflammation will be localised at first but may spread to involve the rest of the eyelid, which will become tender and painful. After one or two days the stye will usually come to a head and may burst, or may simply shrink and resolve. Those that do not resolve may require surgical excision.

Figure 5: Stye on the upper eyelid
Source: Asarelah / Wikimedia Commons
Inflammation of the margin of one eyelid is likely to be caused by a small abscess or stye, which is an infection of a hair follicle gland at the base of an eyelash.
Redness and irritation of the eyelid margins (affecting one or both eyes), often with scales adhering to the base of the eyelashes, occurs in blepharitis (Figure 6). Blepharitis is caused by inflammation of the glands of the margin of the eyelid, most noticeably the eyelash roots. The condition is commonly associated with seborrhoeic dermatitis or dandruff, or it may be allergic; in this case, concurrent conjunctivitis may also be noticed. More rarely, the complaint may be caused by infection. Some eyelashes may be either absent or distorted, sometimes pointing inwards and irritating the surface of the eye. If the cause is infective, pus may be seen discharging from the base of the lashes.

Figure 6: Blepharitis, an inflammation of the eyelid
Source: clubtable / Wikimedia Commons
Blepharitis is caused by inflammation of the glands of the margin of the eyelid, most noticeably the eyelash roots.
Displacement of the eyelids may be seen, particularly in elderly people. In such cases, the margins of the eyelids do not come together when the eyes are closed. Spasm or atony of the orbital muscles causes the lids either to invert, known as entropion (Figure 7), or to evert, known as ectropion (Figure 8). In the former, the lid margins and lashes point inwards and irritate the eye, whereas in the latter the lower lid falls away from the eye, offering it insufficient protection and lubrication.
In both conditions there is an overflow of tears. In ectropion, the lower lid may become chronically infected and scarred. In entropion the lashes may fall out and infection may follow. As with ectropion, if it is seen relatively early on, a minor surgical procedure can correct the displacement. If left untreated it may lead to corneal ulceration because of trauma from the inverted lashes and poor lubrication of the tissues. Entropion and ectropion will usually have been present for a long time before someone seeks advice for these conditions and they require no urgent treatment, although referral for a medical opinion may be appropriate if the patient is at all anxious or worried.
A hard pea-like lump appearing under the skin of the lid, most commonly the upper lid, away from the margin, will probably be a meibomian cyst (chalazion). These may also be found in the lower lid, and can be visualised by pulling down the lower lid to reveal a small lump resembling an internal stye under the conjunctiva (Figure 9). This is an infection of one of the meibomian glands, which are located deep in the cartilaginous tissue on the underside of the lids and secrete fluid on to the conjunctiva. Infection of the outlet of a gland results in blockage and inflammation in the same way that a stye forms. The cyst will normally resolve spontaneously without incident and is generally painless, but may recur from time to time in some people. A persistent cyst may require surgery.
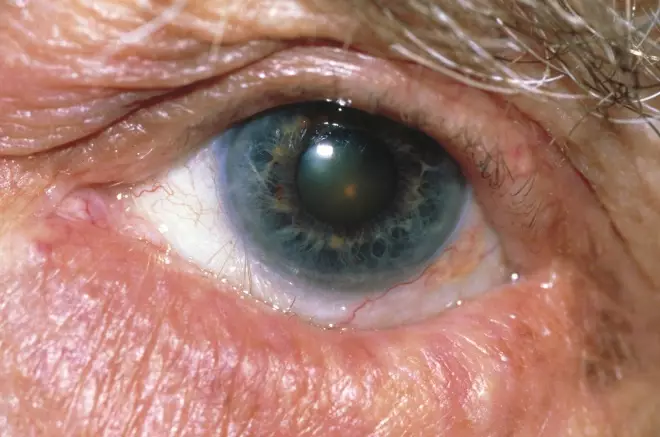
Figure 7: Entropion: the lower eyelid is inverted
Source: Science Photo Library
Spasm or atony of the orbital muscles can cause the lids to invert (entropion).

Figure 9: Meibomian cyst (chalazion)
Source: Science Photo Library
A hard pea-like lump appearing under the skin of the lid, most commonly the upper lid, away from the margin, will probably be a meibomian cyst (chalazion).
Ptosis, which is a drooping upper eyelid (Figure 10), is often a sign of systemic disease, such as myasthenia gravis, and referral is essential. In babies, special measures are needed to rectify the droop to avoid reduced visual input to the brain and blindness. Ptosis is also a sign of Horner’s syndrome, which is caused by a lesion in the cervical sympathetic nerve, often due to trauma, tumours or bleeds.
Accompanying symptoms
Pain
Itchiness, grittiness and soreness on the surface of the eye are common symptoms of minor superficial conditions, such as conjunctivitis. These symptoms should be distinguished from a deep-seated pain arising from within the eye, which indicates possible serious pathology, such as a raised intraocular pressure (glaucoma) or iritis, and requires urgent referral for medical investigation. Similarly, trauma such as flash burns (in welders working with oxyacetylene burners) and corneal injury will cause severe pain. A feeling of grittiness on the surface of one eye only will frequently be caused by a foreign body. It should be relatively easy to distinguish a superficial itching or irritation of the conjunctiva on the eye surface from a more intense pain caused by pathology within the eye itself. Any such pain, which may be accompanied by other symptoms or signs, requires referral for a medical opinion. If severe, referral should be made urgently.

Figure 10: Ptosis, a drooping upper eyelid
Source: Alamy
Ptosis is often a sign of systemic disease, such as myasthenia gravis, and referral is essential.
Nasal symptoms
Conjunctivitis accompanied by nasal symptoms, such as congestion, sneezing and rhinorrhoea, suggests an allergic component to the condition. A sore throat, symptoms of a cold or general malaise may be associated with a viral conjunctivitis, which is usually caused by an adenovirus.
Visual disturbance
Loss of vision is a medical emergency. Disturbance of vision may be caused by the visual component of migraine, in which case it is likely to be recurrent and recognised by the sufferer. The visual disturbances that accompany classic migraine are easily distinguishable from those described here.
In conjunctivitis, vision is not significantly affected because the conjunctiva does not cover the cornea and the underlying pupil, and thus light enters and penetrates the eye in the normal manner. Vision may temporarily be afected if the cornea is obscured by fluid or pus. Loss of visual acuity is often accompanied by pain in the eye, but there are exceptions, such as vascular blockage or haemorrhages in the eye, optic nerve damage, temporal arteritis or retinal detachment, which will not be painful.
Double vision accompanied by ptosis and a headache of sudden onset suggests the possibility of an intracranial bleed and requires urgent medical attention.
Bizarre patterns in the field of vision, with haloes seen around bright lights (particularly noticed when coming out of a dark into a lit area, e.g. when leaving a cinema, or driving at night), requires referral, as this is seen in glaucoma and multiple sclerosis (known as optic neuritis in the latter case). In such cases, individuals should be advised to seek medical opinion; the suspicion of multiple sclerosis should be left unstated as the diagnosis may prove to be different and will require careful handling by a clinician.
Tired eyes
Complaints of tired and sore eyes may be associated with conjunctivitis; in the absence of this condition, the patient can be referred to the optometrist to check for eye strain and any defects in visual acuitya referral to the optometrist may be in order to check for eye strain and any defects in visual acuity.
Lacrimation
Lacrimation is associated with interrupted drainage of the tear film, and in babies it requires referral so that the condition can be rectified. In older people, it will be seen in ectropion.
Pupils
It is wise to carry out a simple physical examination of the eyes, especially if a serious condition is suspected. The pupils should be round and equal in size and they should react equally and oppositely to light, such that each will constrict when a light is directed at it. The pupil should remain circular as it constricts; irregularity suggests adhesions owing to iritis. This may be a previously diagnosed condition, and therefore it should not automatically be assumed that this is a recent finding. Any inequality or abnormality of size, shape or reaction will suggest serious pathology within the eye and the need for immediate referral. A hazy or cloudy appearance to the iris or pupil may be caused by inflammatory exudate in the anterior chamber (as in iritis) or corneal oedema (as in glaucoma), and therefore requires medical referral.
Bulging eye
A rare presentation of a bulging eye (proptosis) or of retracted eyelids (upper, lower or both) may be accompanied by symptoms of an overactive thyroid, such as sweating, hot skin, flushing, tremor of the hands or fingers, weight loss despite an increasing appetite, a fast heart rate and a state of physical overactivity. In a mild form, it is difficult for the untrained observer to detect, but a gap of white sclera between the iris and the affected lid will be seen if the affected eye is, compared with a normal eye. Bulging of one eye, however, raises the possibility of some local pathology behind the eye and both situations require medical appraisal and investigation.
Headache
Headaches accompanying eye symptoms can occur in glaucoma, migraine and temporal arteritis. Understanding the nature of the headache will assist in differentiating these conditions.
| Key points in assessing eye disorder | |
|---|---|
| Site or location | It is important to diffentiate which part of the eye is involved: is it the eyeball, the eyelids or both? It is also important to establish if the symptoms affect both eyes or only one eye. |
| Intensity or severity | It is difficult to assess intensity or severity in eye disorders, but any reported loss of visual acuity, photophobia or pain in the eye should be taken as an important alarm symptom. |
| Type or nature | A painless red eye, disorder of tear formation and inflammation of the eyelids are relatively easy eye disorders to recognise and treat. |
| Duration | Uncomplicated eye disorders should resolve with treatment in a matter of days. If symptoms have been present for a longer period of time, it is worth seeking a review by an optometrist. |
| Onset | Always establish the onset of symptoms and explore any triggers. |
| With (other symptoms) | Consider the presence of other symptoms such as changes in visual acuity, photophobia or pain in the eye. |
| Annoyed or aggravated by | Confirm whether the symptoms are made worse or better by anything, e.g. light levels. |
| Spread or radiation | Symptoms can be restricted to one eye, but can affect the other too. Bacterial conjunctivitis can affect one eye but can also spread to the unaffected eye. |
| Incidence or frequency pattern | If the suffered has experienced symptoms before, establish if there is any pattern, e.g. conjunctivitis can be an allergic response to specific triggers. |
| Relieved by | Always establish if the sufferer has taken any action that has provided any symptomatic relief. |
Management options
If an eye condition does not respond to appropriate simple self-medication within 7 days, then medical advice should be sought. This is because some conditions may become chronic (blepharitis, for example), and some may require treatment with antibiotic (severe infective conjunctivitis, for example).
Antibacterial eye drops and ointments
The agent of choice for infective conjunctivitis is chloramphenicol, although in most cases simple self-care advice is the preferred option as opposed to antibacterial therapy. Chloramphenicol is active against the bacteria commonly implicated in eye infections, such as staphylococci, streptococci and Haemophilus influenzae, and should improve symptoms within 48 hours and completely resolve simple infections within 5 days. Chloramphenicol can be sold to members of the public from pharmacies as eye drops or ointment for the treatment of acute bacterial conjunctivitis in adults and children over 2 years old. The efficacy of eye drops can probably be maximised in the treatment of conjunctivitis by 2-hourly instillation, at least for the first 2 days of treatment. However, most cases of infective conjunctivitis will get better within 1–2 weeks without the use of antibacterial eye drops.
Although it is difficult to distinguish between viral and bacterial conjunctivitis, using antibacterial eye drops in a viral infection is still beneficial. Viral infections will also cause the eye to feel very uncomfortable and therefore the application of an eye drop or ointment will provide some degree of symptomatic relief from this discomfort as well as preventing secondary bacterial infection. It must be noted that chloramphenicol is licensed for supply to the public from pharmacies only for acute bacterial conjunctivitis.
Propamidine is also available in various products that can be sold to members of the public from pharmacies for the treatment of minor eye infections such as conjunctivitis and blepharitis. It has little value in bacterial infections but it has a specific role in the management of the rare, sight-threatening condition Acanthamoeba keratitis. This condition is associated with poor lens cleaning and disinfection, especially with soft lenses, even if they are replaced frequently.
Care should be taken in contact lens wearers that infection has not been caused by the lens itself (as in the case of corneal abrasion or dendritic ulcer) and some may consider it wise to refer such people to their doctor or optometrist before attempting to treat such cases. In any case, lenses must be removed for the whole treatment period with antibacterial drops, because they can cause keratitis (infection of the cornea) to develop as a serious complication. Soft lenses also cause accumulation of preservatives, with resulting irritation, and should not be worn until 24 hours after treatment has finished. Eye ointment containing dibromopropamidine can be used overnight to treat conjunctivitis. It is also suitable as a once- or twice-daily application to the eyelid margins in infective blepharitis and styes, although styes usually resolve spontaneously without the application of antibacterial preparations. However, if there has been a failure to reduce the symptoms of a stye within 7 days or when blepharitis has not responded to appropriate over-the-counter remedies within 7 days, referral for medical opinion would be appropriate because delays may result in the conditions becoming chronic.
Scales or pus adhering to the lid margins can be loosened and lifted by the use of antibacterial eye ointment and by wiping the lid margins with diluted baby shampoo, which is unperfumed and non-irritant.
Simple hygiene measures, such as the use of separate face flannels and towels, may be helpful in preventing the spread of infection to other family members.
Other anti-inflammatory preparations
The cause of allergic conjunctivitis, such as pollen or cosmetics, should be identified and, where possible, removed. Hypoallergenic preparations will still affect some people and the condition will clear only after total avoidance of cosmetics around the eyes. The symptoms are mediated by histamine receptors in the mucosa of the eye. The use of eye drops containing either an antihistamine alone, such as levocabastine, or a combination product such as antazoline together with a vasoconstrictor such as xylometazoline, is effective in providing fast, symptomatic relief in this condition. The vasoconstrictor will address the engorged lymphatic and fine blood vessels in the conjunctiva, which cause the red, swollen appearance of the eyes. If nasal symptoms are also present, as in allergic rhinitis, oral antihistamines should be recommended in addition to eye drops.
Eye drops containing sodium cromoglycate, a mast cell stabiliser, give symptomatic relief of allergic conjunctivitis caused by seasonal allergies. Although sodium cromoglycate eye drops will give symptomatic relief, they must be administered four times a day to maintain their effectiveness. Failure to follow this regimen will result in limited efficacy of this product.
Astringent eye lotions
Eye lotions that contain astringents such as witch hazel are promoted for the treatment of irritation and red eyes. They are best recommended where no specific syndrome exists; for example, in cases where someone complains of ‘tired eyes’ but has no significant conjunctivitis.
Vasoconstrictor substances
Naphazoline is the principal vasoconstrictor drug in over-the-counter eye drops. In conjunctivitis, a sympathomimetic agent such as this will reduce the injection of the conjunctiva with blood by its vasoconstrictive action. This not only serves a cosmetic function but also reduces the irritation caused by the conjunctival hyperaemia and inflammation. It should not be used if other eye disease is present, such as glaucoma.
Other measures
A stye may be drawn to a point to facilitate the exudation of pus by applying a hot compress to the lid. This can be done by soaking a clean towel or flannel in hot water and placing it on the closed lid for several minutes each day.
Where blepharitis is associated with seborrhoeic dermatitis or dandruff, treatment of the skin condition may be undertaken at the same time as local treatment of the eyelids.
Where a blockage of the nasolacrimal duct is suspected (as with excessive lacrimation), an attempt can be made to resolve the problem by applying pressure with one finger to the lacrimal sac at the internal corner of the eye and lightly massaging the duct beneath. Failure to release fluid should not be followed by increasing the pressure. If the condition is troublesome, especially in children, an appointment should be made to see their GP.
Generally people should be reminded to take commonsense measures to reduce the irritant effects of environmental substances, such as dust, cosmetics, smoke and chlorine in swimming pools, where this is appropriate.
Preservatives such as benzalkonium chloride used in eye drops can damage contact lenses, and therefore wearers are best advised to refrain from wearing lenses during treatment and for 24 hours afterwards, if possible.
Case study
Trigger questions
- What additional information do you need before considering the appropriate management options in this case?
- What issues concern you about this case?
- Are any alarm symptoms being exhibited that require more urgent treatment or referral?
Case
A young man complains of a gritty, red right eye which he has had ‘on and off’ for a number of weeks. He explains that the eye is not painful and that he has tried using some eye drops belonging to a friend, but these have not been effective.
Pharmacist opinion
It would be important to establish initially that this man is not experiencing any other symptoms such as alteration in visual acuity, photophobia or pain. By simply looking at the affected eye it will be obvious if there is redness, inflammation and possible discharge. If no discharge is present, then it would be prudent to inquire about this point to ensure that the absence of any discharge is not because it has been cleaned up. In examining the right eye, it should be compared to the man’s left eye to establish whether this is a condition affecting just one eye (unilateral) or both eyes (bilateral).
In examining the eye, it is important to establish which part of the eye is red. By pulling down the lower eye lid it will be possible to establish whether both the sclera and the conjunctiva are red. If this is the case, the likely explanation, assuming the absence of any warning signs, is that he is suffering from conjunctivitis. The description of a gritty feeling in the eye would also support this explanation, assuming that it is not being caused by a foreign body.
It is difficult based on the case described to establish whether this is an allergic or infective conjunctivitis, as typically these present in a similar fashion. The one feature that can help indicate whether there is an allergic or infective cause would be the nature of any discharge. A clear, watery discharge would be associated more with an allergic cause, although this can also be the case in viral conjunctivitis, whereas a purulent discharge is more commonly seen in bacterial conjunctivitis.
The description in this case of the symptoms being experienced as ‘on and off’ for a few weeks is also worthy of consideration. This may suggest that an allergic cause is more likely as the condition has not resolved and is persisting. It would not be uncommon if there was an allergic cause to the conjunctivitis for other signs and symptoms of allergy to be present, e.g. sneezing and/or rhinorrhoea. Equally, these symptoms could also be present if the man was suffering from a cold, considering the ability of infections of the nasal mucosa to extend through the nasolacrimal duct.
It would also be important to establish what eye drops he has been using that belong to his friend, and, importantly, for how long these have been open. The potential that this man may be re-infecting his eye with these eyedrops needs to be borne in mind and investigated thoroughly.
An important consideration in anyone complaining of an eye disorder is whether they are contact lens wearers. The use of contact lenses can cause a number of eye conditions but also some products can have a detrimental effect on the contact lenses themselves. For further information regarding drug treatment and contact lenses see the
British National Formulary
, Chapter 11: Eye.
In this case it would be important to establish whether this man wears contact lenses because, given the duration of his symptoms, he would be best advised to seek the advice of an optician or optometrist.
Acanthamoeba keratitis is a sight-threatening eye condition that is associated with ineffective contact lens cleaning and disinfection and requires specialist medical treatment.
Assuming that there are no alarm symptoms that require investigation in this man, it would be appropriate to advise the use of chloramphenicol if bacterial conjunctivitis is suspected, or if an allergic cause is suspected then a product containing an antihistamine or mast cell stabiliser.
Optometrist opinion
From such brief symptoms, it is difficult to accurately assess the condition; the ‘on and off’ frequency of his gritty red right eye may be caused by an allergic conjunctivitis, where exposure to the allergen could be seen to vary. Infective conjunctivitis is also a possibility with its intermittence either owing to reinfection through cross-infection from sharing his friend’s eye drops or from poor compliance if the drops used were indeed appropriate, but not used at the correct dosage or time period. An intermittently red/gritty eye can also be caused by reduced lubrication from a poor quality tear film leading to a dry eye: this can present unilaterally or bilaterally and often varies in frequency, worsening in dry conditions (central heating/air conditioning) and in periods of concentration such as VDU use, where staring at the screen slows down blinking, allowing evaporation of the tear film to take place. The presence of a foreign body is less likely as this more commonly generates persistent rather than intermittent sensation.
Further questions need to be asked in order to rule out alternative diagnoses. Has vision been affected? Is there any photophobia present? Have there been periods of pain rather the current reported grittiness or indeed any discharge noted over the period of the incident? Knowing the name and frequency of the drops used would also help explain their lack of effectiveness. It is also important to establish if the man is a contact lens wearer, as infection associated with lens wear can prove to be more problematic. Contact lenses and their care products have the potential to generate red uncomfortable eyes if improperly used or if tolerance to either has reduced. In the case of contact lens wearers it is best to refer them on to an optometrist.
Optometry practice provides an ideal setting for an eye examination; vision can be accurately assessed and a variety of instruments are available to aid in the examination of the different structures of the eye. In this case, slit-lamp biomicroscopy would provide a well-illuminated and magnified view of the eye. This allows for detailed observation of the anterior segment of the eye, with the location of redness/inflammation and presence of any discharge easily being observed. Further, the cornea can be assessed for the presence of any infiltrates and/or epithelial defects caused by infection, ulceration, abrasion or exposure from drying. This would allow for a more specific diagnosis and appropriate treatment plan.
General practitioner opinion
These symptoms might suggest viral conjunctivitis. Supportive features would include other viral symptoms, e.g. sore throat, coryza. The intermittent nature of these symptoms would point to a possible allergic element. Further questioning may reveal a specific allergen, usually pollen, but the condition may be work related. A history of hay fever or atopy would further support a diagnosis of an allergic conjunctivitis. Identifying the drops that were ineffective would be helpful in coming to a diagnosis. Any visual disturbance, more significant pain or photophobia might suggest other causes and would need referral.
Viral conjunctivitis is self-limiting and does not require treatment. Allergic conjunctivitis can be successfully treated with antihistamines, although local topical treatment is also available and may be more acceptable.
| Key points for eye disorders | |
|---|---|
| Conditions | Management |
| Bacterial conjunctivitis is characterised by a redness of the sclera and conjunctiva of the eye along with a gritty sensation and purulent discharge. | Chloramphenicol eye drops or ointment for 5 days. |
| Allergic conjunctivitis is characterised by a redness of the sclera and conjunctiva of the eye along with a gritty sensation. | Sodium cromoglycate gives symptomatic relief from seasonal allergies. Eyedrops that contain naphazoline or levocabastine (either alone or in combination):
|
| Subconjunctival haemorrhage is caused by a burst blood vessel. | Heals spontaneously within a few weeks and requires no treatment unless there are accompanying symptoms. |
| Blepharitis is characterised by a redness and inflammation of the margins of the eyelids. | Dibromopropamidine eye ointment applied to the eyelid margins. |
| Styes are characterised by a localised inflammation of the eyelid. | Dibromopropamidine eye ointment can be used in the treatment of styes, but they usually resolve spontaneously. |
When to refer an eye disorder:
- Pain in the eye (in contrast to superficial itchiness, grittiness or soreness);
- Disturbance in vision;
- Suspected infection in contact lens wearer;
- Pupils appear abnormal or uneven;
- Pupils have abnormal or uneven reaction to light;
- Upper eyelid drooping (ptosis);
- Recurrent lump under upper eyelid;
- Recurrent subconjunctival haemorrhage;
- Babies under 3 months old or babies with a squint;
- Existing eye disease;
- Bulging of eyes (proptosis);
- Dry eyes (unless previously seen by a doctor);
- Any associated headache;
- Systemically unwell;
- Specific genitourinary symptoms suggesting the possibility of chlamydial infection;
- Recent long-haul travel in someone whose symptoms are not resolving.
- This article was adapted from
Minor Illness or Major Disease?
, published by Pharmaceutical Press.
You might also be interested in…

Identification and management of common eye disorders

Glaucoma: an overview
