
Shutterstock.com
Patients should be encouraged to self-care for a range of acute pain conditions. However, given the variety of over-the-counter (OTC) analgesics available, appropriate selection can be confusing.
In each patient consultation, including those where the patient asks for a product by name, the pharmacy team member must ensure they have all the relevant information and are making recommendations based on patient presentation and preference, alongside the latest evidence and guidance.
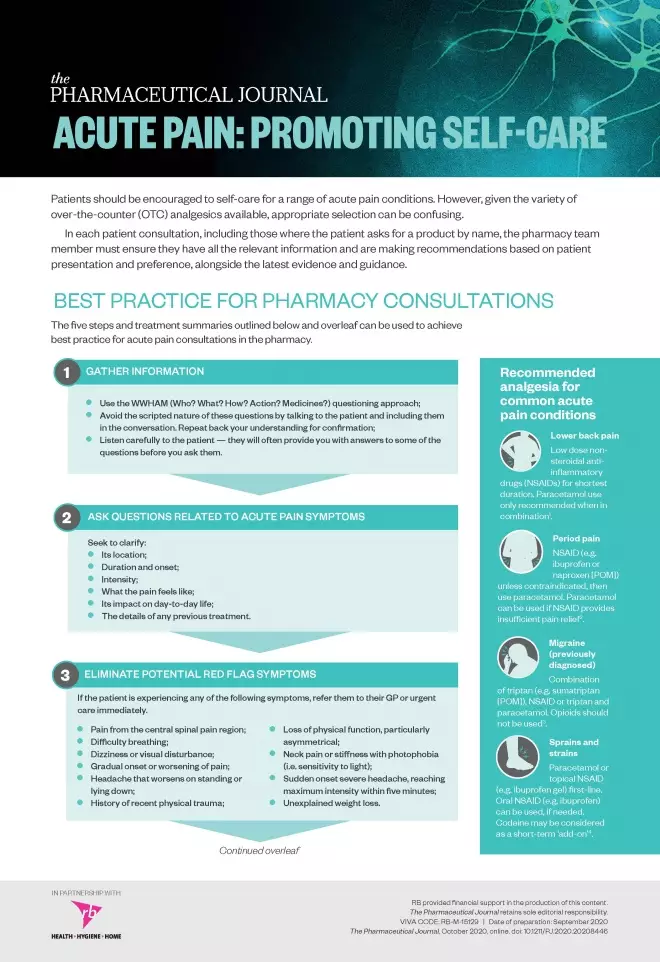
Best practice for pharmacy consultations
The five steps and treatment summaries outlined below and in the learning resource (available to download
here
) can be used to achieve best practice for acute pain consultations in the pharmacy.
Acute pain: promoting self-care, page 1
Acute pain: promoting self-care, page 2
1. Gather information
- Use the WWHAM (Who? What? How? Action? Medicines?) questioning approach;
- Avoid the scripted nature of these questions by talking to the patient and including them in the conversation. Repeat back your understanding for confirmation;
- Listen carefully to the patient — they will often provide you with answers to some of the questions before you ask them.
2. Ask questions related to acute pain symptoms
Seek to clarify:
- Its location;
- Duration and onset;
- Intensity;
- What the pain feels like;
- Its impact on day-to-day life;
- The details of any previous treatment.
3. Eliminate potential red flag symptoms
If the patient is experiencing any of the following symptoms, refer them to their GP or urgent care immediately.
- Pain from the central spinal pain region;
- Difficulty breathing;
- Dizziness or visual disturbance;
- Gradual onset or worsening of pain;
- Headache that worsens on standing or lying down;
- History of recent physical trauma;
- Loss of physical function, particularly asymmetrical;
- Neck pain or stiffness with photophobia (i.e. sensitivity to light);
- Sudden onset severe headache, reaching maximum intensity within five minutes;
- Unexplained weight loss.
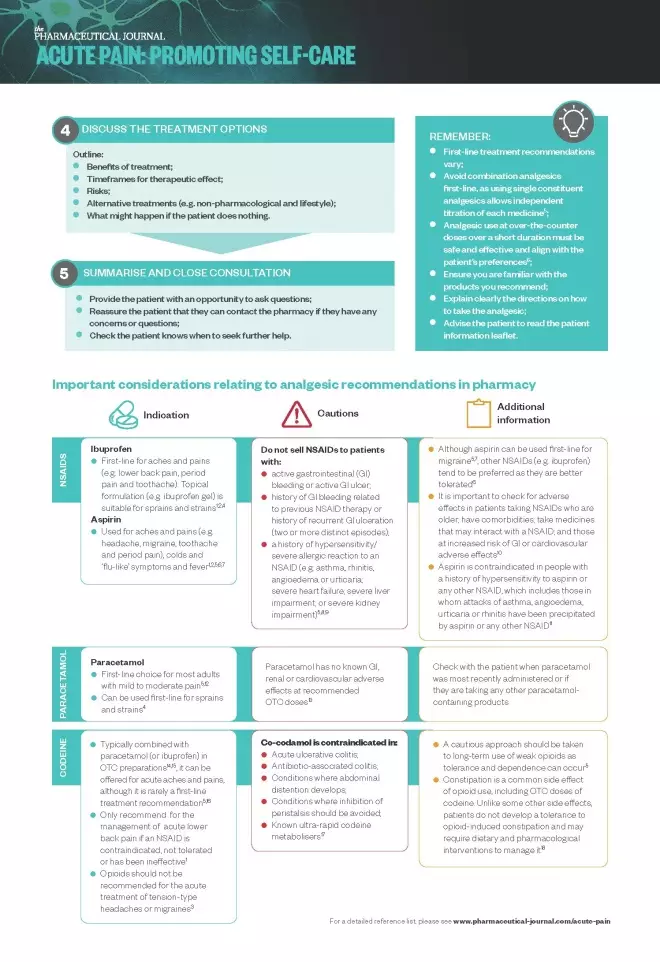
4. Discuss the treatment options
Outline:
- Benefits of treatment;
- Timeframes for therapeutic effect;
- Risks;
- Alternative treatments (e.g. non-pharmacological and lifestyle);
- What might happen if the patient does nothing.
For a summary of the recommended analgesia for common acute pain conditions and important points to remember, see Box.
Box: Recommended analgesia for common acute pain conditions and important points to remember
Recommended analgesia for common acute pain conditions
Lower back pain
- Low dose non-steroidal anti-inflammatory drugs (NSAIDs) for shortest duration. Paracetamol use only recommended when in combination[1]
.
Period pain
- NSAID (e.g. ibuprofen or naproxen [POM]) unless contraindicated, then use paracetamol. Paracetamol can be used if NSAID provides insufficient pain relief[2]
.
Migraine
- Combination of triptan (e.g. sumatriptan [POM]), NSAID or triptan and paracetamol. Opioids should not be used[3]
.
Sprains and strains
- Paracetamol or topical NSAID (e.g. ibuprofen gel) first-line. Oral NSAID (e.g. ibuprofen) can be used, if needed. Codeine may be considered as a short-term ‘add-on’[4]
.
Important points to remember
- First-line treatment recommendations vary;
- Avoid combination analgesics first-line, as using single constituent analgesics allows independent titration of each medicine[5]
; - Analgesic use at over-the-counter doses over a short duration must be safe and effective and align with the patient’s preferences[6]
; - Ensure you are familiar with the products you recommend;
- Explain clearly the directions on how to take the analgesic;
- Advise the patient to read the patient information leaflet.
5. Summarise and close consultation
- Provide the patient with an opportunity to ask questions;
- Reassure the patient that they can contact the pharmacy if they have any concerns or questions;
- Check the patient knows when to seek further help.
Important considerations relating to analgesic recommendations in pharmacy
The table, included on page two of the learning resource, provides more information on the indications, cautions and additional information related to the use of NSAIDs (ibuprofen and aspirin), paracetamol and codeine[1],[2],[4],[5],[6]
[7],[8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18]
.
Download the learning resource here
.
VIVA CODE: RB-M-15129
Date of preparation: September 2020
Safety, mechanism of action and efficacy of over-the-counter pain relief
These video summaries aim to help pharmacists and pharmacy teams make evidence-based product recommendations when consulting with patients about OTC pain relief:
- Safety of over-the-counter pain relief
- Mechanism of action of over-the-counter pain relief
- Efficacy of over-the-counter pain relief
Promotional content from Reckitt
References
[1] National Institute for Health and Care Excellence. NICE guidance [NG59]. lower back pain and sciatica in over 16s: assessment and management. 2016. Available at: https://www.nice.org.uk/guidance/ng59/chapter/Recommendations (accessed October 2020)
[2] National Institute of Health and Care Excellence. Clinical knowledge summaries: dysmenorrhea – primary dysmenorrhea. 2018. Available at: https://cks.nice.org.uk/dysmenorrhoea#!scenario (accessed October 2020)
[3] National Institute of Health and Care Excellence. Headaches in over-12s: diagnosis and management. Clinical guideline [CG150]. 2012. Available at: https://www.nice.org.uk/guidance/cg150/chapter/Recommendations#management-2 (accessed October 2020)
[4] National Institute of Health and Care Excellence. Clinical knowledge summaries: sprains and strains - management. 2020. Available at: https://cks.nice.org.uk/topics/sprains-strains/management/management/ (accessed October 2020)
[5] National Institute for Health and Care Excellence. Clinical knowledge summaries: analgesia — mild-to-moderate pain. 2020. Available at: https://cks.nice.org.uk/topics/analgesia-mild-to-moderate-pain/management/choice-of-analgesic/ (accessed October 2020)
[6] Youssef S. Clinical guidelines and evidence base for acute pain management. Pharm J 2019;online. doi: 10.1211/PJ.2019.20206653
[7] British Association for the Study of Headache. National headache management system for adults. 2019. Available at: https://www.bash.org.uk/guidelines/ (accessed October 2020)
[8] British National Formulary. Ibuprofen: contra-indications. Available at: https://bnf.nice.org.uk/drug/ibuprofen.html#contraIndications (accessed October 2020)
[9] British National Formulary. Naproxen. Available at: https://bnf.nice.org.uk/drug/naproxen.html (accessed October 2020)
[10] National Institute for Health and Care Excellence. Clinical knowledge summaries: NSAIDs - prescribing issues. Available at: https://cks.nice.org.uk/topics/nsaids-prescribing-issues/management/nsaids-%E2%80%93-prescribing-issues/ (accessed October 2020)
[11] British National Formulary. Aspirin: contra-indications. Available at: https://bnf.nice.org.uk/drug/aspirin.html#contraIndications (accessed October 2020)
[12] Prescott LF. Paracetamol: past, present, and future. Am J Ther 2000;7(2):143–147. PMID: 11319582
[13] NHS Inform. Paracetamol. Available at: https://www.nhsinform.scot/tests-and-treatments/medicines-and-medical-aids/types-of-medicine/paracetamol (accessed October 2020)
[14] Euopean Medicines Compendium. Co-codamol 60/1000mg film-coated tablets. Summary of Product Characteristics. Available at: https://www.medicines.org.uk/emc/product/661/smpc (accessed October 2020)
[15] Euopean Medicines Compendium. Nurofen Plus. Summary of Product Characteristics. Available at: https://www.medicines.org.uk/emc/product/5627 (accessed October 2020)
[16] NHS. Medicines: codeine. Available at: https://www.nhs.uk/medicines/codeine/ (accessed October 2020)
[17] British National Formulary. Co-codamol: contra-indications. Available at: https://bnf.nice.org.uk/drug/co-codamol.html#contraIndications (accessed October 2020)
[18] Kumar L, Barker C & Emmanuel A. Opioid-induced constipation: pathphysiology, clinical consequences, and management. Gastroenterol Res Pract 2014;141737. doi: 10.1155/2014/141737
You might also be interested in…
The importance of diverse clinical imagery within health education

Government should consider ways to prevent ‘inappropriate overseas prescribing’ of hormone drugs, review recommends

