JACOPIN/SCIENCE PHOTO LIBRARY)
This content was published in 2011. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Around 20 per cent of women develop a urinary tract infection (UTI) at some time — incidence rises sharply around puberty and remains high thereafter. In contrast, UTI becomes common in men only after the age of 50 years.
Types and terms
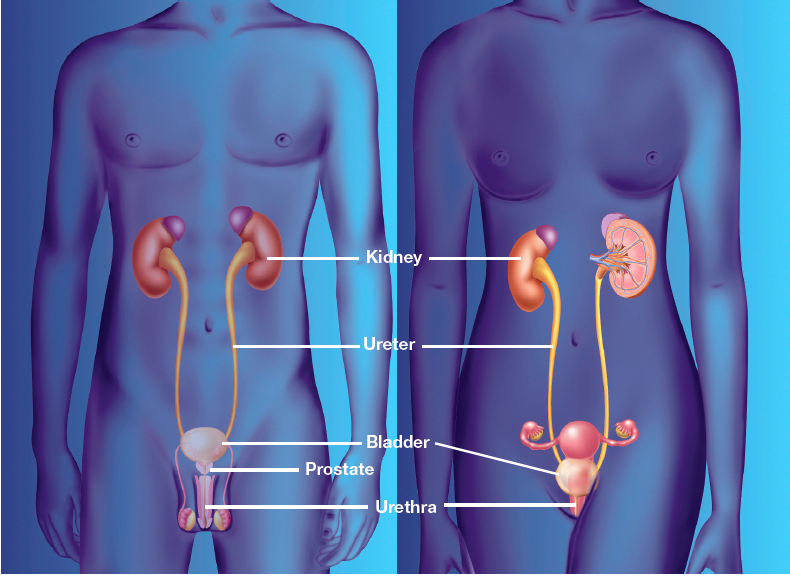
UTIs are best divided into two categories: infections involving only the lower urinary tract (the components of the urinary tract below the ureter, ie, the bladder and urethra) and infections involving both upper and lower tracts.
“Cystitis” is the term applied to bladder inflammation, the commonest cause of which is infection of urine in the bladder.
Upper UTI involves the ureters and kidneys. When the kidneys are involved, the term “acute pyelonephritis” is applied.
Infection in a tract that is anatomically and physiologically normal is termed “uncomplicated” because there are no risk factors that predispose to infection. Anatomical or physiological abnormalities, or both, in the urinary tract (eg, obstruction due to any cause, vesico-ureteric reflux or neurological disorders) predispose to recurrent UTIs, and infection in patients with such abnormalities is deemed “complicated”. Upper UTIs are also sometimes categorised as complicated.
Symptoms and when to refer
The symptoms associated with cystitis are usually pain on urination (dysuria), urgency (inability to delay urination), frequency (urinating small volumes more often) and suprapubic pain. The presence of cloudy or smelly urine or blood in the urine (haematuria) indicates a need to refer the patient to a GP. Urinary frequency accompanied by symptoms of thirst and unexplained weight loss can indicate diabetes and also prompts referral.
If bacteraemia is associated with the infection, the patient is also likely to be systemically unwell, with fever and rigors. Such features are more characteristic of upper UTI, in which case they are associated with loin pain (and tenderness, which a clinician may find on examination) and vomiting.
However, none of these features is solely indicative of UTI — and similar presentations can be seen in other urinary tract disorders such as urethritis, calculi and herpetic lesions.
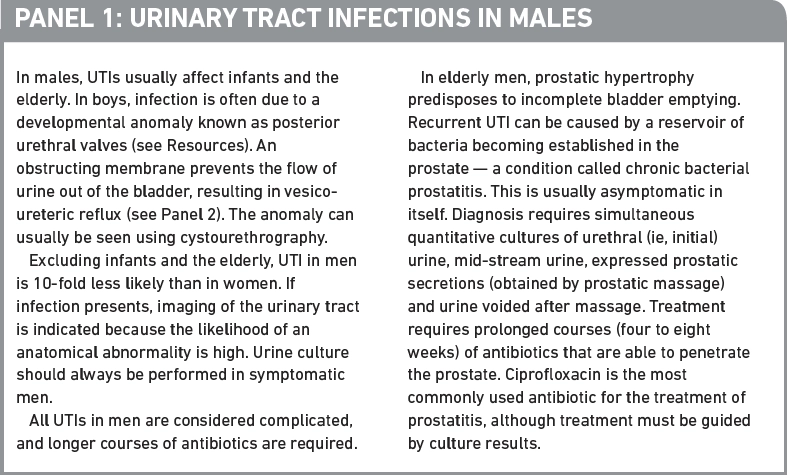
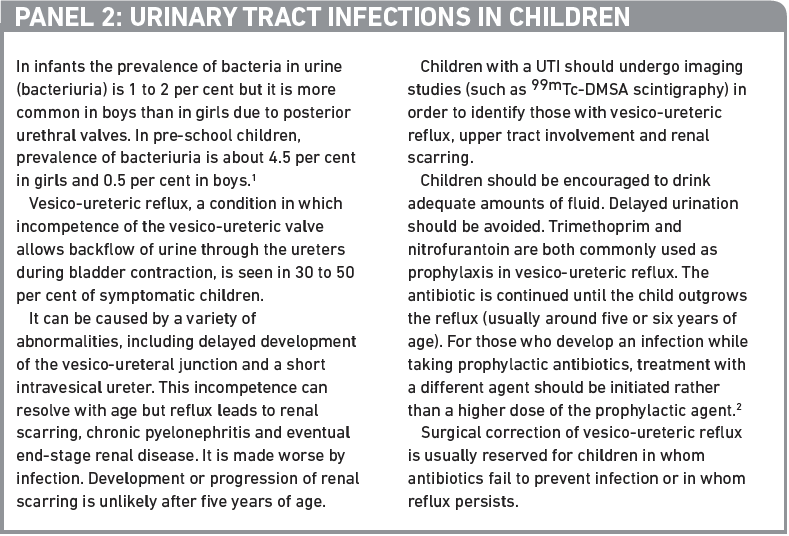
Presentation can also be non-specific, particularly in the elderly, in whom confusion may be a predominant feature. Patients with symptoms of cystitis and who are male (see Panel 1), under 16 (see Panel 2), or pregnant (see Panel 3), or who have diabetes, heart disease or renal conditions should be referred to their GP.
Admission to hospital is required in a few situations, for example, patients who are severely ill with acute pyelonephritis or bacteraemia secondary to UTI. Although it may be possible to manage mild to moderate pyelonephritis with oral antibiotics, the nausea and vomiting that are a feature of more severe infection do not allow this. In these cases, following 48–72 hours of intravenous therapy, it is usually possible to discharge the patient on suitable oral treatment after the acute symptoms and signs have settled. Patients infected with a multi-resistant pathogen (eg, extended-spectrum beta-lactamase producing enterobacteriaeceae) for which there are limited effective oral therapeutic options may also require hospital admission.
Reflect
- How is urinary tract infection diagnosed?
- What options are available for urine collection in children?
- What strategies are used for prophylaxis? Before reading on, think about how this article may help you to do your job better.
Organisms
UTI accounts for around 23 per cent of hospital-acquired infections. Over 95 per cent are unimicrobial, the most common family of micro-organisms involved being Enterobacteriaceae.
In normal urinary tracts Escherichia coli is the most common pathogen. Recurrent infection, however, is a feature of anatomically or physiologically abnormal urinary tracts, and other micro-organisms, such as Proteus spp, Enterobacter spp, Enterococcus spp, Staphylococcus spp and Pseudomonas aeruginosa, are more common in these cases.
The prevalence of antibiotic-resistant infections tends to be higher in patients with recurrent infections, in those who have had multiple antibiotic exposures for other illnesses and in nosocomial (eg, urinary catheter related) infection.
Risk factors
Risk factors for UTI include:
- Anatomical or physiological urinary tract abnormalities
- Sexual activity
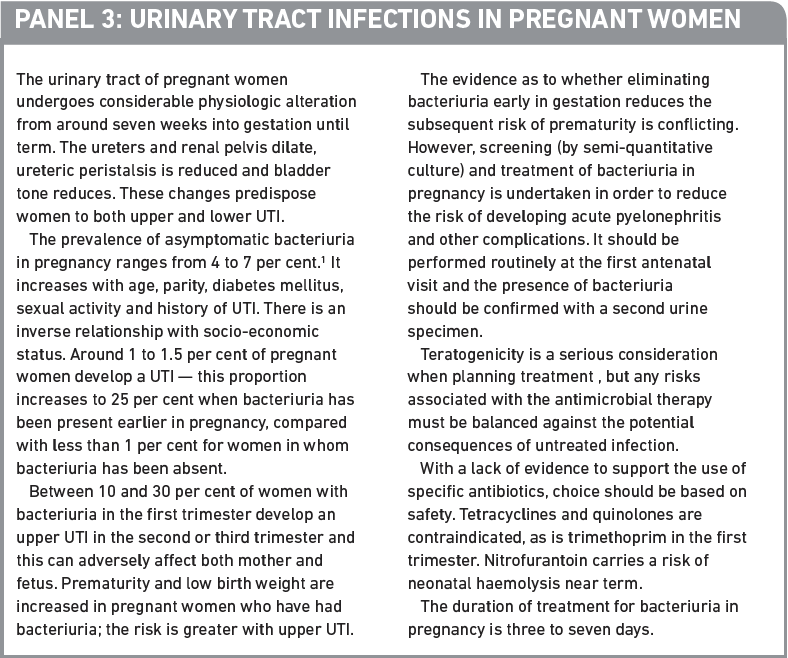
- Pregnancy
- Urinary tract procedures (eg, cytoscopy)
- Diabetes mellitus
- Being immunocompromised
- Catheterisation
Any condition that prevents complete voiding of urine predisposes to infection. In children, the most common is vesico-ureteric reflux (see Panel 2).
Prostatic hypertrophy can often cause urinary tract obstruction and, in elderly women, bladder prolapse can lead to incomplete voiding. Many neurological disorders, such as multiple sclerosis, can also affect voiding.
Urinary catheterisation provides a portal of entry for pathogens into the urinary tract — between 20 and 30 per cent of catheterised patients develop bacteriuria, of whom 2 to 6 per cent develop symptoms of UTI. The risk of acquiring bacteriuria is approximately 5 per cent for each day of catheterisation.
Diagnosis and testing
Urine specimens for diagnosis of infection include mid-stream urine and suprapubic aspirates and are discussed further in Panel 4.
Dipstick testing
Urine dipstick testing for nitrites and leucocyte esterase provides a rapid and economical means of screening for UTI. Bacteria tend to break down urinary nitrates to nitrites, which are not found in normal urine, and leucocyte esterase is produced by the increased neutrophils present during infection.
The combined negative predictive value of nitrites and leucocyte esterase of 98 per cent allows UTI to be excluded with confidence in many patient groups. On the other hand, the relatively low positive predictive value of this technique (38 per cent) must be considered.3
The detection of proteinuria and haematuria by dipstick testing is unreliable, with a high rate of false positives and false negatives, and is, therefore, of comparatively little diagnostic value.
In addition, dipstick testing has been found to be unreliable in pregnant women, children under three years of age and patients with urinary tracts with structural anomalies or diabetes mellitus, or who are immunocompromised. Urine specimens from these patients must be cultured regardless of the dipstick result.
Microscopy
Microscopy can be used to detect haematuria (ie, erythrocytes in the urine), white cells in urine (pyuria) and bacteriuria.
Haematuria, although a feature of cystitis, is not always present and is seen in many other conditions (eg, neoplasia, calculi). Pyuria indicates inflammation within the urinary tract. It is suggestive but not diagnostic of infection. For example, neutropenic patients will have UTI without pyuria. Bacteriuria, particularly in combination with pyuria, is, however, highly suggestive of infection. In children below three years of age, the sole presence of bacteriuria is accepted as evidence of urinary tract infection.2
Culture
Semi-quantitative culture is the mainstay of diagnosis. This technique makes it easier for the laboratory to distinguish infection from contamination — an important consideration given that the urethra, in contrast to the bladder, is not sterile.
Counts greater than 100,000 colony forming units/ml of a single isolate are generally accepted as indicative of infection. Smaller numbers (100–1,000 colony forming units/ml) and multiple isolates often reflect contaminated specimens but can, in some situations, be significant, particularly when patients are symptomatic. Any isolate from a suprapubic aspirate is likely to be significant regardless of colony count.
Culture is the only option for catheter samples but multiple isolates are frequently obtained. These usually reflect catheter colonisation rather than UTI and do not require treatment in the absence of symptoms.
Routine urine culture is not required to manage lower UTIs in non-pregnant women but those who fail to respond to first-line therapy (usually trimethoprim or nitrofurantoin — see later) should have their urine cultured to inform subsequent treatment.
Susceptibility testing
Antibiotic susceptibility testing is performed whenever there is isolation of an organism deemed significant. The range of antibiotics tested will vary with local epidemiology, prescribing practices and policies.
Complications of UTI
Of patients with a UTI, 1 to 4 per cent develop bacteraemia and, of these, 13–30 per cent die.5 Perinephric and intrarenal abscesses are recognised complications of urosepsis.
Perinephric abscesses are relatively uncommon and usually complicate infections where urinary obstruction exists. Intrarenal abscesses are being increasingly recognised as a complication of acute pyelonephritis. The development of an abscess necessitates inpatient investigation and treatment. Imaging techniques include ultrasonography and computed tomography — percutaneous aspiration can often be performed under radiological guidance both to provide specimens for microbiological analysis as well as for therapeutic drainage. Antimicrobial treatment should target the pathogens isolated. Surgical drainage may be necessary if percutaneous drainage is not possible (approximately 10 per cent), particularly with larger abscesses. After good drainage, complete resolution of symptoms should occur in most cases with two weeks of antimicrobial therapy.
Treatment
Symptomatic UTIs
Female patients presenting to the pharmacy with cystitis and who do not need to be agents such as sodium or potassium citrate solutions for symptomatic relief. However, the evidence base for recommendation is limited and, in mild cases, symptoms are likely to resolve without treatment. Caution is needed in patients taking drugs such as angiotensin-converting enzyme inhibitors, potassium-sparing diuretics or lithium and drugs reliant on acidic urine for their excretion, which would include nitrofurantoin.
General advice that can be given includes maintaining adequate hydration and ensuring frequent urination; evidence to support a link with lifestyle factors is, however, limited.
If symptoms persist the woman should be referred to her GP. Current guidelines recommend that women with symptomatic lower UTI should receive empirical antibiotic treatment.6 According to Clinical Knowledge Summaries, on average, antibiotics shorten the duration of symptoms by about a day.
In asymptomatic bacteriuria the potential risks of not treating and the expected benefits of treatment need to be balanced against the side effects of the agent used.
Asymptomatic bacteriuria can be associated with permanent renal impairment from chronic pyelonephritis in pre-school children and poor outcomes in pregnancy so treatment in these cases is essential.
Asymptomatic UTIs
Given the serious consequences of persistent bacteriuria in these patients, a post-treatment urine specimen should be obtained to ensure bacteriological cure.
The elderly are more susceptible to the side effects of antibiotic therapy, and treatment of UTI is not associated with improvement in overall outcome. Moreover, the infection is much more likely to recur. In view of these factors, treatment of asymptomatic bacteriuria is not indicated in this population.
Options
First-line antibiotic choices for uncomplicated lower UTI include nitrofurantoin and trimethoprim. In women and children, symptomatic cure can be achieved with courses of short duration, usually for three days. Men should be treated for at least seven days.
In pregnancy, penicillins (eg, amoxicillin) or first generation cephalosporins are preferred as empiric treatment, but therapy should be adjusted according to sensitivities.
Upper UTI (or pyelonephritis) requires a longer duration of antibiotic treatment (10 to 14 days). Empiric treatment options include a second or third generation cephalosporin, coamoxiclav, quinolone or an aminoglycoside such as gentamicin. This empiric treatment is often given intravenously for 48–72 hours, and then switched, where possible, to oral therapy guided by microbiological results.
In light of the emergence and rapid spread of resistance in organisms known to cause UTIs (eg, extended-spectrum beta-lactamase producing E coli), certain relatively old antibacterial agents are being reintroduced. For example, fosfomycin, which is unlicensed in the UK, is seeing increased use for lower UTI and temocillin is used for upper and complicated UTI. Both antibiotics achieve high urinary concentrations — uncomplicated UTI in most patient groups can be treated with a single dose of fosfomycin due to its slow excretion into the urine.
An application to switch trimethoprim from POM to P was withdrawn last year. It has been shown that in countries with fewer restrictions on antimicrobial supply resistance rates are higher. Improving prescribing practice can contribute to reducing antimicrobial resistance.
Recurrent infection may be caused by either the same or a different organism, therefore the same antimicrobial agent may be used again unless resistance is known. Recurrence relates to patient risk factors for reinfection rather than resistance to the antibiotic. Relapse involves the same organism and suggests treatment failure, potentially due to anatomical reasons that should be investigated.
Prophylaxis
Recurrent UTI in women is defined as three episodes in the past 12 months or two in the preceding six months. In addition to investigation, antibiotic prophylaxis should be considered for those who have frequent recurrences, especially if they are debilitating, result in hospital admission or require parenteral treatment. Suitable regimens include trimethoprim 100mg on and nitrofurantoin 50–100mg on. Prophylactic antibiotics should be taken at night when urine flow is low.
Use of any antibiotic over an extended period carries a risk of resistance developing, so prophylaxis is usually restricted to six to 12 months. The available evidence does not support longer duration of use.7
In children, the small benefit of reduced risk of UTI should be weighed against the increased risk of developing resistant organisms.
Women with frequent recurrences can be advised to take cranberry products on the basis that they inhibit the adhesion of bacteria to the urinary tract epithelium, therefore preventing infection. However, the potential for benefit varies, depending on patient group, dose and duration. Study results are inconsistent and the required dose is unclear. Patients taking warfarin should use cranberry products with caution.6 Women with normal upper urinary tracts may also find methanamine hippurate helpful in reducing the occurrence of symptomatic UTI.
If an infection develops while a patient is taking antibiotic prophylaxis, a different agent should be used for treatment, rather than a higher dose of the same antibiotic.
Antibiotic prophylaxis is not recommended in catheterised patients. One meta-analysis showed no significant reduction of bacteriuria and a two-fold increase in antimicrobial resistant bacteria (although not in those receiving methenamine).6
Genitourinary atrophy may increase the risk of bacteriuria. Oestrogen therapy has demonstrated variable efficacy in reducing the risk of symptomatic UTI, but it is clear that this is less effective than antibiotic prophylaxis. Two systematic reviews of vaginal oestrogen administration both report considerable inconsistency of results; some studies show significant reduction in risk of recurrent UTI while others show no significant effect and even a trend towards harmful effects. Oestrogen therapy may have a role in some patients, but it is not recommended for routine prevention of recurrent UTI in postmenopausal women.
Key points
- Refer men, children under 16, pregnant women, those with diabetes, heart or renal conditions, cloudy or smelly urine, haematuria, or thirst and unexplained weight loss.
- Guidelines recommend that women with symptomatic lower urinary tract infection should receive empirical antibiotic treatment but, on average, antibiotics shorten symptom duration by about a day.
- Use of prophylactic antibiotics for recurrent UTIs is usually restricted to six to 12 months.
Practice points
Reading is only one way to undertake CPD and the regulator will expect to see various approaches in a pharmacist’s CPD portfolio.
- Review questions to ask patients to presenting with cystitis.
- Make sure your healthcare assistants know which groups should be referred.
- Review the appropriateness of prophylactic antibiotics.
Consider making this activity one of your nine CPD entries this year.
Resources
- Further information about posterior urethral valves is available at www.gosh.nhs.uk
- A summary of updated international guidelines from the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases for the treatment of acute uncomplicated cystitis and pyelonephritis are available at www.escmid.org (accessed 20 August 2011).
References not currently available online.


