Wikimedia commons
This content was published in 2010. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
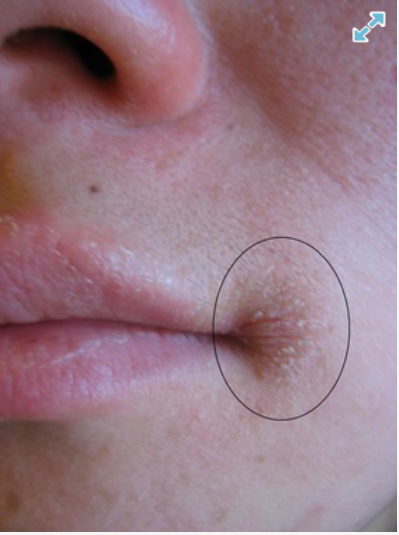
A: The most likely diagnosis here is angular cheilitis (also known as angular stomatitis, perleche or commissural cheilosis). This condition, which affects around seven in 1,000 people, is characterised by erythema, scaling and crusting in the corners of the lips (labial commissures).
Sufferers often experience pain or discomfort (sometimes described as a burning sensation) and the lips can split and bleed on opening the mouth wide.
The main differential diagnosis would be herpes labialis but cold sores are normally unilateral. (They start as macular lesions that become vesicular, pustulate and then undergo crusting.)
Angular cheilitis is most common in the elderly and in denture wearers. It is also seen in people with HIV, Crohn’s disease or ulcerative colitis.
Find out
There are several potential causes of angular cheilitis, including nutritional deficiency, inflammatory skin disease, mechanical trauma (eg, flossing can cause a short-term unilaterial lesions) and infection, so effective questioning is important to find a likely one. Windburn or excessive sun exposure can also give rise to the condition.
The basic pathophysiology leading to angular cheilitis is maceration of the skin in the commissures, which disrupts the epidermal barrier. Such disruption provides a breeding environment for fungi and bacteria. In the absence of cell cultures it is difficult to distinguish between a fungal or bacterial cause.
Licking sore lips exacerbates things because salivary amylase damages the barrier. In children, angular cheilitis can result from thumb sucking, use of dummies, lip biting or excessive lip licking.
Hypersalivation, which is often seen in Downs’ syndrome, can lead to cheilitis. Paradoxically, xerostomia (dry mouth) can also lead to cheilitis due to the lack of saliva, which contains antimicrobial proteins.
Angular cheilitis can involve staphylocci, where the reservoir infection occurs in the anterior region of the nostrils, or streptococci, where the organisms come from the mouth.
There is thought to be a link between angular cheilitis and nutritional deficiencies, in particular vitamin B compounds (riboflavin, niacin, folate and cyanocobalamin). The condition can also arise as a consequence of deficiencies of iron and zinc, so may be seen in people with eating disorders.
Angular cheilitis is known to be associated with inflammatory skin conditions such as atopic dermatitis and allergic contact dermatitis (eg, from the use of lip balms, lipsticks and even toothpastes). Oral retinoids (eg, isotretinoin, acitretin) can worsen the problem.
Candidiasis
Angular cheilitis is often associated with oral thrush. Although candida is part of the normal oral flora, in about 60 per cent of elderly people with dentures overgrowth of this yeast is a problem — dentures give rise to an anaerobic, low pH environment. Angular cheilitis has also been observed in patients with braces.
Overgrowth of candida is also linked to use of broad spectrum antibiotics, which alter the oral flora, and inhaled corticosteroids, which are thought to suppress cellular immunity and phagocytosis. (Rinsing the mouth with water after using inhaled steroids will help to reduce the oral accumulation of steroids.)
Other factors associated with candidiasis include a high carbohydrate diet, smoking, diabetes, Cushing’s syndrome and immunodeficiency.
Treatment
Successful treatment of angular cheilitis depends on the cause. For example, topical therapy is likely to fail in nutritional deficiency. In mild cases due to trauma, the use of lip balms containing occlusive agents, such as petroleum jelly, may be all that is required to allow the skin to heal.
It would be worth finding out if the girl has concomitant oral thrush or a history of any skin or eating problems. If oral thrush is present, a seven-day trial of miconazole oral gel, used inside the mouth and on the cheilitis would be appropriate.
(Although the product is not specifically licensed for angular cheilitis there is some evidence to support its use and some dermatologists and GPs prescribe it for cheilitis in the absence of thrush. Miconazole is also bacteriostatic to Gram positive organisms such as staphylococci.)
The treatment can be continued for a further seven days if there is some response to it. There is some evidence for the effectiveness of other antifungal agents such as nystatin and amphotericin.
When to refer
If topical antifungal therapy is not effective, it would be worth referring the girl to her GP for a more thorough assessment to exclude any underlying nutritional deficiencies. Measurement of ferritin levels and a full blood count to determine haemoglobin levels would be a first-line approach.
You might also be interested in…
How to select the right mouthwash

Thalassaemia and iron supplements
