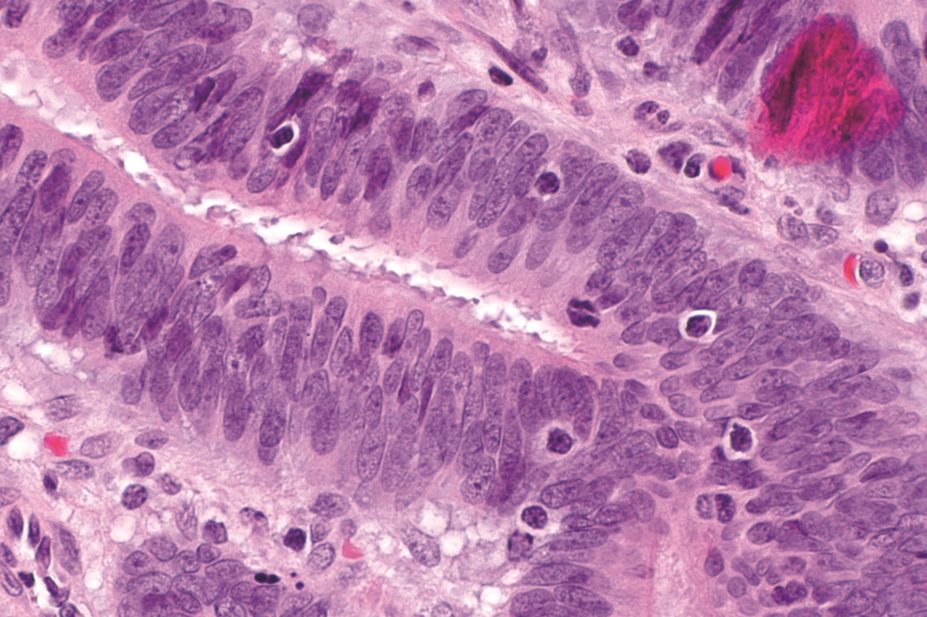
Nephron / Wikimedia
Obesity is associated with a greater risk of colorectal cancer in patients with Lynch syndrome (LS) – also known as hereditary non-polyposis colon cancer – but this risk is offset by taking aspirin regularly, an international study published in the Journal of Clinical Oncology
[1]
shows.
The study confirms other literature that shows obesity is a risk factor for colorectal cancer. “What was surprising was that the effect was much greater in those who also had a genetic predisposition and that the excess was largely cancelled by having taken aspirin for two years,” says John Burn, a professor at Newcastle University, who led the research. “This provides an insight into how obesity influences the cancer process.”
The researchers hypothesised that, compared with LS patients of normal weight, obese LS patients may have a greater cancer risk because of their diminished ability to combat DNA damage.
They tested their hypothesis on 937 LS carriers in 16 countries who were enrolled in the colorectal adenoma/carcinoma prevention programme 2 study. The LS carriers either took 600mg of aspirin per day for two years or a placebo.
The results showed that at follow-up, up to ten years later (mean follow-up 56 months), 55 LS carriers had bowel cancer. For obese participants, colorectal cancer risk was 2.4 times greater than for underweight and normal-weight participants. However, those who took aspirin had the same risk irrespective of whether they were obese.
Although the mechanism responsible for the increased cancer risk among obese patients with LS remains unknown, the researchers suggest that “given the germline loss of DNA mismatch repair capacity in LS, it may be hypothesised that adverse sequelae of greater body fatness (e.g. chronic low-level inflammation) have a promoting effect on those stem cells that have accumulated DNA damage because of this dysfunctional repair system.”
“This study helps to further underline the importance of the obesity-colorectal cancer link, with particular relevance to patients with LS,” says Mark Hull, representing the British Society of Gastroenterology. “The data hint that the beneficial effect of aspirin on colorectal cancer risk may be heightened in overweight individuals.”
Nick Bason, director of external affairs for Bowel Cancer UK, says the research is helpful in furthering understanding of the risk of bowel cancer in people with LS, and the role aspirin can play in helping to reduce that risk.
“The research also shows that all aspects of risk need to be considered, and having a healthy body weight is an important part of that. We recommend that anyone who thinks they are at higher risk of bowel cancer go to their GP before taking aspirin,” he adds.
According to the report, these findings suggest that, in addition to recommended bowel surveillance, patients with LS are likely to benefit substantially from prevention – or effective treatment – of obesity and from regular aspirin use. A large-scale follow-up trial is now being planned, with researchers hoping to recruit 3,000 people around the world to determine the effect of different doses of aspirin.
References
[1] Movahedi M, Bishop DT, Macrae F et al. Obesity, aspirin, and risk of colorectal cancer in carriers of hereditary colorectal cancer: a prospective investigation in the CAPP2 study. Journal of Clinical Oncology 2015. doi:10.1200/JCO.2014.58.9952.


