Shutterstock.com / JL
The introduction of minor ailment schemes (MASs) was a central plank of a much-heralded government scheme to use the “enormous potential” of pharmacy to deliver access to clinical services to people in “the most deprived areas”. But cash-strapped local commissioners in England are taking an axe to them.
An investigation by The Pharmaceutical Journal has revealed that around one in five pharmacy MASs in England have been cut over the past three years (see Box 1).
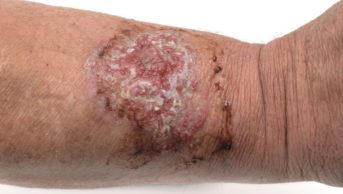
These schemes — which cost an average of £86,000 per clinical commissioning group (CCG) — are designed to provide free NHS treatment for minor conditions, such as colds, allergies and minor skin conditions, at pharmacies, so that patients do not need to visit a GP for a prescription. But The Pharmaceutical Journal has learnt that 23 of the 104 pharmacy minor ailment schemes in England were decommissioned between 2015 and 2018, and a MAS that covers 14 London boroughs is only hanging on by a thread.
This is in stark contrast to the situation in the devolved nations, where Scotland is expanding its pharmacy MAS. In Wales, a common ailments service is now available in more than 80% of Welsh pharmacies (see Box 2).
The cuts in England come as CCGs are enthusiastically implementing new guidance that restricts the prescribing of common over-the-counter (OTC) treatments for minor conditions, such as coughs, earache and diarrhoea. The Pharmaceutical Journal discovered that nearly two-thirds of CCGs have implemented this guidance — or had similar guidelines in place already (see Box 3).
People on low incomes could have to choose between whether they eat or treat
Some pharmacists in these areas say that people who can afford to pay for their own treatment will be able to cope with these cuts, but people on low incomes could be hit hard, perhaps — in some cases — having to make the choice between whether they “eat or treat”.
Different vision
The picture was different in 2008 when the then Department of Health published the white paper ‘Pharmacy in England: Building on strengths — delivering the future’, which included plans for MASs in all pharmacies in England.
The government said at the time that “pharmacy’s ready availability in more deprived areas offers enormous potential on which to capitalise and expand access to healthcare services for more disadvantaged groups or those who do not regularly use other health services”. In October 2016, the then health minister David Mowat said he expected MASs would be commissioned across all of England by April 2018.
Box 1: Minor ailment schemes in England
- 43% — the proportion of areas that currently commission a pharmacy minor ailment scheme (MAS).
- 12% — the proportion of areas that have decommissioned a pharmacy MAS between 2015 and 2018.
- 22% — the proportion of MASs cut by commissioners between 2015 and 2018.
- £86,837 — the median annual spend per MAS. Knowsley Clinical Commissioning Group’s (CCG’s) ‘Care at the chemist’ scheme had the highest average annual budget of £280,000, while the lowest budget was in Oldham, where funding for 2017/2018 was £3,000.
Source: Investigation by The Pharmaceutical Journal. Data provided by 190 CCGs under the Freedom of Information Act.
This all changed in 2017. That October, Keith Ridge, chief pharmaceutical officer for England, acknowledged in a meeting of the All Party Pharmacy Group that CCGs were beginning to decommission MASs, saying that “things have moved on”.

Source: Jeff Gilbert
Keith Ridge, chief pharmaceutical officer for England, acknowledged in 2017 that clinical commissiong groups were beginning to decommission minor ailments schemes, saying that “things have moved on”
At that meeting, Ridge said the decommissioning of MASs was, in part, owing to the rollout of the NHS Urgent Medicine Supply Advanced Service scheme, which utilises volunteer pharmacies to provide out-of-hours emergency prescriptions. He also attributed the cuts to what was then an NHS consultation on reducing the prescribing of common OTC products and “low-volume” medicines.
That guidance has now been formally introduced, despite concerns raised at the time by the BMA, the RPS and others
That guidance has now been formally introduced, despite concerns raised at the time by the British Medical Association (BMA), the Royal Pharmaceutical Society (RPS) and others that it could affect deprived populations the most.
Saving money
When it published
guidance for CCGs
on limiting prescriptions for OTC items, NHS England said it could “free up to almost £100m for front-line care each year”. At the time of publication, Graham Jackson, co-chair of the joint clinical working group that developed the list of conditions and co-chair of NHS Clinical Commissioners, said the NHS recognised that the changes “may be difficult for some patients who have previously been prescribed these products, but it is right that we prioritise our spending on those that provide the best outcomes for patients”.
The guidance includes exemptions for cases where prescriptions should continue. Patients who qualify for free prescriptions are not automatically exempted, but people who need OTC medicines to help with a long-term condition are. So are patients who, in the judgement of a clinician, may be unable to adequately manage self-care owing to “medical, mental health or significant social vulnerability”.
In the guidance, CCGs are advised that they must take steps to protect vulnerable patients from these restrictions, and three-quarters of CCGs said they have taken steps to do this. However, there is wide variation in what form this action has taken; most CCGs have simply circulated the guidance with the exemptions highlighted, but a few have taken further measures.
Box 2: Where pharmacy minor ailments schemes are expanding
In September 2018, the Scottish government announced that following a pilot in Glasgow, a universal minor ailments scheme (MAS) would be rolled out nationwide to all patients, regardless of age and social circumstance. In Wales, a common ailments service is now available in more than 80% of pharmacies, a scheme Andrew Evans, the Welsh chief pharmaceutical officer, says diverts people from “less appropriate” parts of the NHS.
New minor ailments schemes are being commissioned in England, but it is rare. One example is in Dudley clinical commissioning group (CCG). Jag Sangha, a pharmaceutical adviser at the CCG, said in August 2018 when his CCG established a new MAS that the group was “conscious of the inequality of access” to medicines that would be addressed through the scheme for some people on low incomes.
Airedale, Wharfedale and Craven, Bradford City and Bradford Districts CCGs said they completed an engagement exercise prior to implementation of the guidance “to assess whether the population had different needs to those identified by the NHS England impact assessments”. Trafford CCG said that a “full equality and quality impact assessment has been completed as part of implementation”.
But pharmacists are worried about the impact of this guidance and the concurrent move to decommission MASs. Stephen Foster is pharmacist manager at G Whitfield pharmacy in Houghton-le-Spring, near Sunderland. His was one of a small number of pharmacies that provided a MAS in his area before it was decommissioned in April 2018. Prescribing restrictions have also been introduced within his CCG.
Patients must be thinking twice about whether they can afford to buy medicines over the counter
Foster says patients “must be thinking twice” about whether they can afford to buy medicines over the counter. He cites the example of ibuprofen and paracetamol for children with colds and head lice treatment, which is included in the prescribing restrictions but costs £10 to buy. “Before, we could provide treatment through the minor ailments scheme,” he says. “Anecdotally, the head lice situation is pretty bad. Patients can’t afford to pay, so there’s a lack of treatment. This warm summer, I think we saw an increase in kids with head lice.”
Protecting vulnerable patients
In the Sunderland area, “more savvy” GP practices do follow elements of the guidance that is designed to protect vulnerable patients, but it is patchy among local doctors, says Foster. “I’ve seen things that ‘shouldn’t’ be prescribed being prescribed,” he says. “But in a wider sense, not all GPs seem to be using the ability to recognise that they can prescribe if they want to.”
In London, the future of the pharmacy minor ailments schemes is unclear
In London, the future of the pharmacy MAS is unclear. NHS England London announced that it was ending the service in June 2018, but The Pharmaceutical Journal revealed in August 2018 that it will run until at least March 2019 when a decision will be made on its long-term future. The delay to decommissioning the MAS was announced after concerns from pharmacists and GPs that many vulnerable patients would not be adequately protected if the service was scrapped.

Source: Royal Pharmaceutical Society
Sanjay Ganvir, director of Green Light Pharmacy and chair of Camden and Islington local pharmaceutical committee, says he has had “awful conversations with patients” about what would happen if the London minor ailments scheme ends
Sanjay Ganvir, director of Green Light Pharmacy (a small chain of London pharmacies) and chair of Camden and Islington local pharmaceutical committee (LPC), says he has had “awful conversations with patients” about what would happen if the scheme ends. “They’ve said, ‘What am I going to do? I can’t afford to buy food as it is. If it comes to a choice, I’ll go without food so my kids get medicine’. That’s the reality of it. That’s life for a lot of people.”

Source: Nic Bunce / The Pharmaceutical Journal
Sandra Gidley, chair of the English Pharmacy Board of the RPS said that cutting minor ailments schemes means that people on low incomes could be forced to either eat or treat their illness
Sandra Gidley, chair of the English Pharmacy Board of the RPS, agrees: “We had concerns at the time the NHS guidance was introduced that it could be the death knell of MASs. [It] potentially means that people on low incomes may not be able to afford certain products and are forced to ‘eat or treat’.”
Gidley adds that this, in combination with the guidance restricting the prescribing of low-value items, will have the consequence of putting more pressure back on GPs: “Many GPs feel that if they have identified a need for treatment, they are morally bound to prescribe it. An unintended consequence is that patients will redouble their efforts to obtain products from their GP, putting extra pressure on an already stretched system.
Pharmacists are working to limit the damage caused to vulnerable patients by the change in policy
“Maybe it is time that more serious consideration is given to pharmacy being the first port of call for common ailments, with a list of common ailments standardised and provisions made for those who can genuinely not afford the medicines they need. Not necessarily free for all children, but based on family income.”
Box 3: Restrictions on over-the-counter and low-value medicines
- 64% — the proportion of clinical commissioning groups (CCGs) that have implemented the new guidance from NHS England or had similar pre-existing guidance to restrict the prescribing of over-the-counter (OTC) or “low-value” medicines.
- 23% — the proportion of CCGs which are planning to implement the guidance later, or are “considering” implementing it (as at the end of October 2018).
- 73% — the proportion of CCGs which said that they had taken steps to protect vulnerable patients when introducing the NHS advice on restricting OTC medications, with a further 2% saying they were considering or planning measures to ensure exemptions were in place.
- 52% — the proportion of CCGs with no pharmacy minor ailments scheme and have implemented, or are in the process of implementing, the new guidance to restrict the prescribing of OTC or low-value medicines.
Source: Investigation by The Pharmaceutical Journal. Data provided by 190 clinial commissioning groups under the Freedom of Information Act.
However, in other areas, pharmacists are working to limit the damage caused to vulnerable patients by the change in policy. In Derbyshire, the CCG said the introduction of the OTC prescribing guidance was a factor in its decision to decommission minor ailments schemes. Jackie Buxton, chief officer of Derbyshire LPC, says her committee was “disappointed” that its MAS had been decommissioned because it supported GP practices by freeing capacity and particularly helping vulnerable patients access medicines safely. “We are concerned that the decommissioning of the service will lead to more requests for GP appointments, adding to the strain on primary care services,” she says.
But Buxton says arrangements have been put in place to ensure patients are protected. “We encourage local discussions between practices and pharmacy teams so that patients receive consistent messages from both,” she says. “We also meet regularly with Healthwatch and have ensured their teams are aware of and understand the CCG’s self-care policy, and the NHS England guidance about restricting prescribing for minor, self-limiting conditions.”
Michael Keen, chief executive officer of Kent LPC, says that in his view: “The matter of vulnerable patients still receiving a prescription, rather than being asked to pay for medicines, is clouded by the way that NHS England advised CCGs to stop the prescribing of OTC medicines but did not simply blacklist the items. In essence, they shifted the responsibility to the CCGs.” He added: “I believe GPs will continue to do what is in the interests of vulnerable patients in front of them, and others needing long-term treatments, as the BMA advises and has stated is the correct approach.”
It’s basically saying to prescribers, do some sort of arbitrary means-testing, based on you having a patient in front of you
A spokesperson for NHS England said it was up to individual CCGs to decide whether to commission MASs “where they make a meaningful difference to patients, are affordable, represent good value for money and reflect guidance on OTC medicines”. They added that NHS England was investing in new services, such as the digital minor illness referral service, which allows NHS 111 operators to refer people with minor health concerns to a chosen community pharmacy for a booked consultation, which makes “the best use of the clinical skills of community pharmacists to provide timely, convenient and accessible care to patients with minor health concerns”.
But Ganvir speaks for many pharmacists when he expresses his concerns that patients will be the ones who are likely to suffer from this sudden policy switch. He says: “It’s basically saying to prescribers, do some sort of arbitrary means-testing, based on you having a patient in front of you — when GPs are, by the NHS’s own admission, under pressure,” he says. “It’s outrageous, and it’s non-evidence based.”
- The Pharmaceutical Services Negotiating Committee were approached for comment, but did not respond in time for publication.