
Shutterstock.com
Anna suffered severe symptoms of chronic fatigue syndrome (CFS), a mysterious disease also known as myalgic encephalomyelitis (ME), from the age of 21 years. The disease forced her to abandon her master’s degree and leave her job as a teacher. She became increasingly confined to her apartment, removed from the life she once knew. “Any time I tried to do something that I didn’t have the energy for, I felt nauseous and dizzy, with fever and pains in my joints and muscles,” she says.
After a couple of years she sought help from a physiotherapist for her wasting muscles. “[My physiotherapist] mentioned this study and asked if she could give my name to the researchers,” she says. So in 2008, Anna (whose name has been changed) was enrolled in a phase II double-blind placebo-controlled trial testing a radical new treatment for CFS/ME. The research group, from Norway’s Helse Bergen University, administered intravenous drips to Anna but she showed no improvement and, after 12 months, discovered she was in the placebo arm of the trial. She was then eligible to receive the real medicine.
For the first time in my life I felt restless because I wanted to do things
This time, Anna started to notice a change after about three months. “On the one hand I was more tired, but then I’d have small bursts of energy where I’d feel great for maybe half an hour and I’d do the dishes and the hoovering.” Gradually, Anna felt less and less tired and after about a week the bursts of energy began to last. “It was amazing, oh god it was wonderful,” she says. “For the first time in my life I felt restless because I wanted to do things.”
The medicine Anna received was not designed to treat CFS/ME and had no stimulant properties. Rather, Anna had been given rituximab, a monoclonal antibody used to treat lymphoma and rheumatoid arthritis. Rituximab destroys the antibody-producing B cells of the immune system. Its effect on CFS/ME was discovered by chance, suggesting to researchers that the illness could be some sort of immune system dysfunction. However, the drug is very potent — Anna suffered serious side effects — and some doctors have raised concerns about its use.
CFS/ME is an illness that affects 250,000 people, mostly women, in the UK. But the disease is controversial; standard medical tests find nothing wrong, which initially led many doctors to dismiss it as psychological, a stigma some patients still battle. In recent years, however, more sophisticated tests and innovative clinical trials have yielded small clues that researchers are hopeful might eventually lead to some answers on how to treat the condition.
For 70% of CFS/ME patients, their disease is preceded by an infection, usually glandular fever, caused by Epstein-Barr virus. In Anna’s case, she experienced mild symptoms from the age of 16 but only began suffering severely after a fever while travelling in India at the age of 21.
Struck by a profound fatigue, patients with CFS/ME are often unable to carry out basic tasks. Symptoms can worsen if patients attempt to push themselves, called post-exertional malaise, and there may be ‘brain fog’, as well as nausea, muscle pain and unrefreshing sleep. For many patients this can continue for years, if not decades.
Chronic fatigue syndrome remains a medically unexplained syndrome
“The symptoms are very similar to flu symptoms,” says Alastair Miller, a consultant in infectious diseases at North Cumbria University Hospitals NHS Trust who specialises in CFS/ME and is chair of the British Association of CFS/ME (BACME). Isolated and unable to participate in society, patients with CFS/ME are seven times more likely to commit suicide than the general population. Yet despite these profound and debilitating symptoms, “it remains a medically unexplained syndrome”, he says.
Disease recognition
The first medical description of the condition dates back to 1869 when George Miller Beard, a US neurologist, described a condition he called neurasthenia, or nervous exhaustion, now believed to be synonymous with CFS/ME. Neurasthenia gained widespread attention in medical literature until the 1930s but its popularity declined in western medicine until medics once again began to take an interest in the condition in the 1980s. The term “chronic fatigue syndrome” was first used in 1988 by the US Centers for Disease Control to formalise the name given to the collection of symptoms.
Following the recognition of CFS, there was a highly publicised and protracted battle between parts of the medical community and patient advocate groups. Some doctors believed it was “all in the mind”, owing to its unexplained nature. Patients reported being treated with disrespect by doctors or offered aggressive exercise regimens. Meanwhile, patient advocate groups campaigned to have the disease recognised as a physical condition. But it was not until 2002 that there appeared to be a shift in attitude to the disease in the UK.
A report, commissioned by the UK’s chief medical officer, effectively banned doctors from stating they did not “believe” in the condition. The report also incorporated ME into the name at the request of patient groups, who felt that CFS did not adequately reflect the physical aspects of the disease. Leading up to the publication of the report, NHS funding increased and there are now many specialist treatment centres for CFS/ME in the UK, although there are still few treatment options.
Viral aetiology
But some doctors have dedicated their careers to finding treatments for patients with CFS/ME, rejecting the idea that it is psychological despite the scepticism that lingers around the disease. Jose Montoya, a doctor and researcher at Stanford University, California, recalls his first encounter with a CFS/ME patient in 2004. “What struck me was how much life this patient had lost,” he says. As an infectious diseases specialist, he had been asked to examine the patient for an underlying infection.
It went from instinct to professional specialism — it could be the greatest scientific and medical challenge of this century
Montoya ordered tests, which revealed that the patient had high levels of antibodies to cytomegalovirus and human herpes virus 6. He decided to use valganciclovir, a strong antiviral that he had been using for immunosuppressed patients after organ transplant. After the patient received the drug, “we saw a dramatic difference”, he says. Motivated to help more patients, Montoya went on to establish a CFS/ME initiative at Stanford that aims to understand the role that viral infections can play in triggering the disease. “It went from instinct to professional specialism — it could be the greatest scientific and medical challenge of this century,” he says.

Courtesy of Dr Jose Montoya
Jose Montoya, a doctor and researcher at Stanford University, California, conducted a trial of antiviral drug valganciclovir in chronic fatigue syndrome/myalgic encephalomyelitis patients
Montoya pursued the idea that CFS/ME may be caused by an inappropriate immune response to a viral infection, such as human herpes virus or Epstein-Barr virus, which can periodically reactivate or reinfect patients. In 2013, he published the results of a placebo-controlled trial of valganciclovir with 30 CFS/ME patients that had raised antibody levels to either human herpes virus 6 or Epstein-Barr virus. After nine months, patients who received valganciclovir showed improvements on the fatigue severity scale (1–7), with scores declining from 6.1 to almost 5.5, compared with a slight increase from 6 to 6.2 in the placebo group, although a score above 5 is still considered severe fatigue. There were also improvements on the mental fatigue subset of the multidimensional fatigue inventory, as well as in patient-reported cognitive function[1]
.
The purist in me says wait for the large study, but the compassionate side says I’m allowed to use these drugs and week after week I see patients getting better on these antivirals
But the evidence is not definitive, partly because of the small number of patients in the trial. “We want to follow it up with a much larger sample size, but there’s no money,” Montoya says. Despite this, he continues to use the drug in the clinic. “The purist in me says wait for the large study, but the compassionate side says I’m allowed to use these drugs and week after week I see patients getting better on these antivirals.”
The lack of funding for research into CFS/ME is something that has been hampering treatment for years, says Montoya. But this may be about to change. In February 2015, after reviewing 9,112 published papers, the influential Institute of Medicine in the United States released a report stating that CFS/ME is a serious physiological and not psychological illness and criticised the lack of research funding. In response, in October 2015 the National Institutes of Health (NIH), said it would bolster research efforts under the guidance of Walter Koroshetz, director of the National Institute for Neurology Disorders and Stroke at the NIH. Montoya believes this recognition will lead to more research money, but he estimates that between US$100m and US$400m is needed each year to catch up with other diseases.
Despite the paucity of funding for research, Montoya has been involved in some small breakthroughs. In 2014, a brain imaging study of 15 patients with CFS/ME found distinct differences to 14 healthy controls[2]
. In the front, right side of the brain there is “a band of fibres that is thicker” in patients with CFS/ME, says Montoya. This is more pronounced in sicker patients and could serve as biomarker for the disease, he adds.
In 2015, research published in Science found that during the first three years of the disease, patients had elevated levels of interferon gamma, a cytokine released in response to viral infections and which the researchers say is consistent with the hypothesis of a viral trigger or of immune system dysregulation[3]
. In collaboration with Columbia University, New York, Montoya is now helping to examine an extensive panel of 51 cytokines.
In separate findings at Cornell University, New York, researchers have identified changes in the gut microbiome and inflammatory microbial markers in blood samples taken from patients with CFS/ME. Using this information, the researchers correctly distinguished 83% of patients from healthy controls, which they say offers non-invasive diagnosis and a step towards understanding the cause of the disease[4]
.
Immunological imbalance
Montoya believes that the disease is probably inflammatory in nature. The research in Norway that Anna was involved in fits with this theory, he says. But the Norwegian researchers would rather describe the disease as an immunological imbalance of some sort, not inflammation in the usual way of defining it. “We don’t see evidence of classic inflammation and tissues damage,” says Øystein Fluge, a researcher and oncologist at Haukeland University Hospital, part of Helse Bergen University in Norway, who is conducting the research on rituximab. Classic signs of inflammation include redness, swelling, pain and invasion of immune cells that can cause tissue damage.
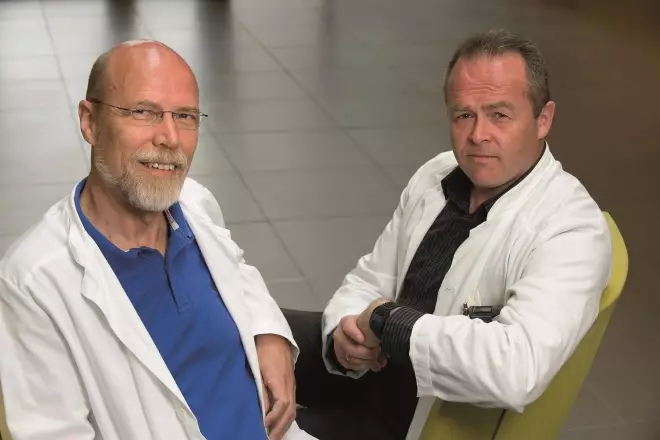
Courtesy of Olav Mella and Øystein Fluge
Olav Mella (left), director of the oncology department at Haukeland University Hospital, Norway, and Øystein Fluge, a researcher and oncologist, from the same hospital, are conducting a phase III trial of rituximab in chronic fatigue syndrome/myalgic encephalomyelitis patients
Like Montoya, Fluge first came across a patient with CFS/ME by chance. A patient with Hodgkin’s lymphoma had been wheelchair bound with CFS/ME for seven years. After chemotherapy she experienced major relief of her fatigue symptoms, says Fluge. At first, he wasn’t sure if the improvement was just by chance. Then in 2007, he treated another patient for large B-cell lymphoma who had been bed bound with CFS/ME for eight years. Four and a half months after treatment with rituximab, she too experienced major relief of her symptoms. “So then we thought perhaps this isn’t a coincidence,” he says.
In 2008, Fluge, along with the director of the hospital’s oncology department Olav Mella, conducted the 30-person randomised trial in which Anna participated. A major or moderate response was observed in 67% of patients (10/15) who were given rituximab, compared with only 13% given placebo (2/15)[5]
.
Fluge and Mella then carried out a further open-label phase II trial with 29 patients that showed similar results, with 64% of patients having a major or moderate response to the drug[6]
. On average, there was a 27.4 point improvement on the Short Form-36 (SF-36) physical function score (a scale of 0–100) at 20 months in the open-label trial, and a slight to moderate patient-reported improvement in fatigue score from a baseline of extreme to moderate fatigue. However, responders (17/27) had an average 40.4 point improvement on the SF-36 physical function score at 20 months and a self-defined moderate to major improvement in fatigue after treatment. Six of these patients were back in full-time work or study and five more in part-time work. The researchers believe that this indicates there is a group of patients for whom rituximab is effective. And the research has attracted the attention of several CFS/ME organisations.
But larger studies are needed before conclusions can be drawn. So the team are now testing rituximab in a 24-month double-blind phase III trial with 152 patients across five centres in Norway. Fluge hopes the results will be published in early 2018.
Maybe an antibody is targeting a receptor without causing the classic signs of inflammation, this also means it might be reversible
Fluge hypothesises that the disease could be caused by rogue antibodies (produced by B cells, which are the target of rituximab). “Maybe an antibody is targeting a receptor without causing the classic signs of inflammation, this also means it might be reversible,” muses Fluge. However, patients with CFS/ME do not have elevated B-cell levels, something that other researchers, including Miller, say casts doubt over the Norwegian group’s findings. Fluge counters that B cells, which mature into plasma cells, can singularly produce vast quantities of antibodies, “you only need one to be pathogenic to cause problems”. It’s a waste to eliminate all the B cells, he adds, and eventually he wants to identify the specific antibody.
Miller says he supports the phase III rituximab trial, but adds that rituximab is “a very toxic drug and I wouldn’t want to use it in patients without far more solid evidence”. Indeed, both times Anna was given rituximab, she suffered late-onset neutropenia, requiring intravenous antibiotics. One other patient in the open-label rituximab study also experienced late-onset neutropenia and two others an allergic reaction to the drug.
Fluge stresses that he does not support the use of rituximab outside of clinical trials. “We have a biological hypothesis, that it’s the B cells, at least in a subgroup of patients like Anna,” he says. But the phase III data are needed to verify or refute this hypothesis, he says, and points out that “we are open to the different outcomes”.
Fluge is right to be cautious — there have been false hopes in the past. In 2009, a study published in Science identified a new mouse retrovirus, called XMRV, which was present in a high proportion of CFS/ME patients and not in healthy controls. Immediately, the CFS/ME community wanted treatment with antiretrovirals and a test was developed for the virus, says Miller. However, dozens of subsequent trials failed to replicate the study and eventually it was found that the presence of the virus was the result of contamination.
In addition to the rituximab trial, the team at Haukeland is conducting a trial using chemotherapy drug cyclophosphamide. Fluge has treated three CFS/ME patients with breast cancer using cyclophosphamide, after which they had remission of their CFS/ME symptoms. A 40-person open-label trial is now underway, with the results expected to be published in January 2017, he says.
CBT and GET
Until the results of the 152 patient rituximab trial are published, there are evidence-based therapies available but these are perhaps the most controversial of all. “One of the only proven therapies is cognitive behavioural therapy (CBT) and graded exercise therapy (GET),” says Miller. In 2011, researchers from the UK published a study in The Lancet, called PACE: comparison of adaptive pacing therapy, CBT, GET, and specialist medical care for CFS[7]
.
Adaptive pacing therapy is a technique advocated by patient groups that recommends patients adjust their activity levels to match their energy reserves and do not push themselves. This technique was pitted against CBT and GET, which were administered based on the theory that “fear avoidance” of activity or physical deconditioning resulting from inactivity, respectively, perpetuate the symptoms of fatigue. Patient groups have responded angrily, saying that it implies the disease is psychological and are disputing the data (Queen Mary University of London is currently fighting a freedom of information request for patient level data to be released). Fluge also takes issue with the fear avoidance theory, saying that “when I see patients improve they are really eager to grip life”.
Yet after 52 weeks of follow up, fatigue scores were significantly lower in the CBT and GET groups compared with specialist medical care (by 3.4 and 3.2 points, respectively, on the Chalder fatigue scale [a 0–33 point scale]) and physical function scores improved (by 7.1 and 9.4 points on the SF-36 scale compared with specialist medical care, and 19.2 and 21.0 points from baseline). Adaptive pacing, however, did not lead to any improvement compared with specialist medical care. Miller, who was involved in reviewing the adverse events data in the trial, says “a bunch of people are very against [CBT and GET] and it’s really demoralising”.
Maybe all chronic disease patients could learn to cope better with CBT
Miller argues that “we use CBT and GET in cancer and rheumatoid arthritis as an adjunct for pain control, it’s not because we see this as a mental health condition”. Fluge agrees, pointing out that “maybe all chronic disease patients could learn to cope better with CBT”. But he says he does not believe that there is any effect on the underlying disease mechanisms.
Across the many specialist CFS/ME centres in the UK, CBT and GET is the mainstay of treatment, because it’s really all that is available along with pharmacological symptom management (table 1). Simon Collin, a researcher at the University of Bristol who examines outcomes data for CFS/ME patients who access NHS services, says the national outcomes data “roughly reflect” the results of the PACE trial.
| Symptom | Drug management |
|---|---|
| Source: British Association of CFS/ME (BACME) guide for therapy and symptoms management in CFS/ME | |
Pain | Low-dose tricyclic antidepressants (e.g. amitriptyline), anticonvulsants (e.g. gapapentin or pregabalin), non-steroidal anti-inflammatory drugs |
Gastrointestinal symptoms: | |
Nausea Functional non-ulcer dyspepsia or gastro-oesophageal reflux disease Irritable bowel syndrome | Antihistamines if associated with migraine Antacids, proton pump inhibitors Antispasmodics, loperamide, antimotility, macrogol laxative, linaclotide, low-dose tricyclic antidepressants |
Autonomic symptoms, commonly including postural hypotension or postural tachycardia syndrome | Increase fluid intake to 2.5 litres |
Sleep disturbance | Amitriptyline, short-term zolpidem or zopiclone, antihistamines |
Co-morbid mental health issues, such as PTSD, depression and anxiety disorders | Citalopram, fluoxetine, sertraline, mirtazapine, duloxetine |
Pete Gladwell, a physiotherapist, leads the Bristol CFS/ME service. He explains that both CBT and GET aim to stabilise a patient at a baseline of activity before gradually trying to improve. “The important thing with CFS/ME patients is that there is the possibility of full or partial recovery … but there is debate about how to define this,” he says. For example, an athlete may return to average levels of physical activity, “but does that count as a full recovery for them?” he asks. Collin concurs. In a two-year follow up of the PACE study, published in Psychological Medicine, researchers said recovery was 22% in both the CBT and GET arms, compared with 8% for adaptive pacing therapy and 7% for specialist medical care[8]
. But this research, Collin says, provoked “a flurry of angry responses from patient groups“, which dispute the criteria used to judge recovery.
Collin says the Medical Research Council and the Wellcome Trust in the UK are taking the question of what causes CFS/ME “very seriously”. The UK’s CFS/ME Research Collaborative launched a grand challenge at its conference in 2015, which aims to collect 10,000 samples from patients and analyse genetics, epigenetics and gene expression, although it hasn’t yet secured funding.

Courtesy of Simon Collin
Simon Collin, a researcher at the University of Bristol, examines outcomes data for patients with chronic fatigue syndrome/myalgic encephalomyelitis who access NHS services
After managing to secure some money from the NIH, researchers at DePaul University, Illinois, are hoping to study 6,000 students at Northwestern University in a bid to see who develops CFS/ME and understand the reasons why. “They know 600 will get glandular fever and about 60 will not recover,” says Collin. On a smaller scale, Fluge is collaborating with teams in Berlin, Arizona and London to analyse 200 patient samples for biochemical abnormalities.
Ultimately, most researchers agree that there is no dividing line between the body and mind, and that anything that helps one will help the other. But that is little comfort to patients whose lives have been devastated by the illness. For Anna, her response to rituximab lasted for years, changing her life dramatically. “When I was sick, I was alive, but I didn’t have a life. You miss out on everything. Now, I have a job, I have hobbies, I go dancing every week, I have money to buy a flat. I have a life and I didn’t before.”
Box 1: Symptoms for which there is no pharmacological therapy
- Fatigue: the hallmark of CFS/ME, which is chronic and disabling. It is not somnolence (sleepiness) and if somnolence is present, an alternative diagnosis, such as sleep apnoea, should be considered.
- “Payback”: post exertional malaise defined as worsening of symptoms after excess exertion.
- “Brain fog”: cognitive impairment, including low grade confusion and memory loss.
- Lymphadenopathy: a common complaint from patients, if not attributable to any other source, cannot be treated pharmacologically.
- Frequent upper respiratory tract infections: there is no role for prophylactic or frequent therapeutic antibiotics, unless there is convincing evidence of an acute bacterial infection.
Source: British Association of CFS/ME (BACME) guide for therapy and symptoms management in CFS/ME
References
[1] Montoya JG, Kogelnik AM, Bhangoo M et al. Randomised clinical trial to evaluate the efficacy and safety of valganciclovir in a subset of patients with chronic fatigue syndrome. Journal of Medical Virology 2013;85:2101–2109. doi: 10.1002/jmv.23713
[2] Zeinech MM, Kang J, Atlas SW et al. Right arcuate fasciculus abnormality in chronic fatigue syndrome. Radiology 2015;274:517–526. doi: 10.1148/radiol.14141079
[3] Hornig M, Montoya JG, Klimas NG et al. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Science Advances 2015;1:e1400121. doi: 10.1126/sciadv.1400121
[4] Giloteaux L, Goodrich JK, Walters WA et al. Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome. Microbiome 2016;4:30. doi: 10.1186/s40168-016-0171-4
[5] Fluge Ø, Bruland O, Risa K et al. Benefit from B-lymphocyte depletion using the anti-CD20 antibody rituximab in chronic fatigue syndrome. A double-blind and placebo-controlled study. PLoS One 2011;6:e26358 doi: 10.1371/journal.pone.0026358
[6] Fluge Ø, Risa K, Lunde S et al. B-lymphocyte depletion in myalgic encephalopathy/chronic fatigue syndrome. An open-label phase II study with rituximab maintenance treatment. PLoS One 2015;10:e0129898. doi: 10.1371/journal.pone.0129898
[7] White PD, Goldsmith KA, Johnson AL et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. The Lancet 2011;377:823–836. doi: 10.1016/S0140-6736(11)60096-2
[8] White PD, Goldsmith K, Johnson AL et al. Recovery from chronic fatigue syndrome after treatments given in the PACE trial. Psychological Medicine 2013;43:2227–2235. doi: 10.1017/S0033291713000020

