Medi-Mation/Science Photo Library/ Shutterstock.com
In the mid-2000s there was a wave of excitement across the pharmaceutical industry. Unravelling before scientists’ eyes was a new discovery about cells that had the potential to transform medicine. “The world became enamoured with this idea — because it was very powerful. If you can inject something into a person that can silence only one gene, you can treat an awful lot of diseases that no one could before,” says Christopher Anzalone, chief executive officer of Arrowhead Pharmaceuticals. “It was hyper specific. It was truly a surgical drug.” But just a few years later and the industry that had sprung up around this discovery had “crashed”, he says.
If you can inject something into a person that can silence only one gene, you can treat an awful lot of diseases that no one could before
The industry in question is RNA interference (RNAi) therapeutics. RNA, or ribonucleic acid, is the lesser-known cousin of DNA, deoxyribonucleic acid. Scientists discovered RNA’s important function in the expression of genes many years ago. Segments of DNA are copied into something called messenger RNA (mRNA), which is is used as a template for the synthesis of proteins. The problem is that if the template is faulty, so is the protein, which can cause a large number of diseases. However, it was not known that a whole other type of RNA is able to shut this process down.
In 1998, geneticists Craig Mello, then working at the University of Massachusetts Cancer Center in Worcester, and Andrew Fire, who was at the Carnegie Institution of Washington in Baltimore, Maryland, made the discovery that if double-stranded RNA (dsRNA) was injected into small worms, it switched off the dsRNA’s corresponding gene[1]
. This led to the identification of RNA interference (RNAi) as a new cellular pathway, for which the researchers won the Nobel Prize for Medicine and Physiology in 2006.
It was found that dsRNA with a sequence complementary to one encoded by mRNA targets the mRNA for destruction before it can be used as the template to build a protein. By introducing a small dsRNA molecule, called small interfering RNA (siRNA), into a cell, a gene can be effectively silenced (see Figure). When it was established in 2002 that this process was common to mammals[2]
,[3]
, “it became apparent that this could work as a therapy because all the machinery was already there”, says Mark Kay, a geneticist at Stanford University, California, who was the first to demonstrate RNAi in mammals.
Investments and disinvestments
A string of new companies and multimillion dollar investment deals followed. “People got excited that this was going to transform medicine so there was tonnes of hype,” says Anzalone. One of the first and biggest RNAi companies, Alnylam, was founded in 2002. In 2005, Novartis agreed to purchase 19.9% of the company’s stock with an upfront payment of US$57m and potential for payments of up to US$700m. Two years later, Roche paid US$331m for the purchase of just under 5% of Alnylam’s stock in a deal worth up to US$1bn. In 2006, Merck waded into the field with the purchase of a different biotechnology company Sirna for US$1.1bn. And another company, Dicerna, was founded in 2007 hoping to capitalise on new discoveries in the field.
Things like monoclonal antibodies try to mop up faulty proteins … and it’s like mopping up the floor after a spill, whereas we turn off the source of the faulty protein before it’s made
One of the reasons for all the interest in RNAi was that it has a number of potential advantages over existing strategies. Brendan Martin, the general manager of Alnylam Pharmaceuticals for the UK and Ireland, says that RNAi-based therapies could help treat previously untreatable diseases at very low doses and potentially before they even emerge. “Things like monoclonal antibodies try to mop up faulty proteins … and it’s like mopping up the floor after a spill, whereas we turn off the source of the faulty protein before it’s made,” explains Martin. In addition, he says, RNAi takes up residence in the cell where it has a “sort of catalytic mechanism” enabling it to destroy one piece of mRNA after another: “So a very low dose can last for a long time”.
However, bringing RNAi to the clinic has not proved quick or easy. Initial clinical targets were diverse; spread across eye disease, cancer and viral hepatitis[4]
. The first clinical trial of an RNAi was in 2004 — with a study on the potential for siRNAs to treat wet age-related macular degeneration, a common cause of blindness. Despite promising early results, when the candidate progressed to phase III in 2008 the trial was terminated because of a lack of efficacy. Suspicions were later raised that the strategy could itself cause another form of blindness in certain patients[5]
. The company developing the candidate subsequently dropped it.
Two years later and no closer to bringing a drug to market, the pharmaceutical industry’s initial optimism was dead. In 2010, Novartis announced that it would not be continuing its partnership with Alnylam, causing the biotechnology company to lay off more than a quarter of its workforce. More bad news quickly followed when Roche also decided to discontinue investment in RNAi research. Arrowhead Pharmaceuticals bought up Roche’s RNAi research in 2011, but Anzalone says it was a “dark time” for the field.
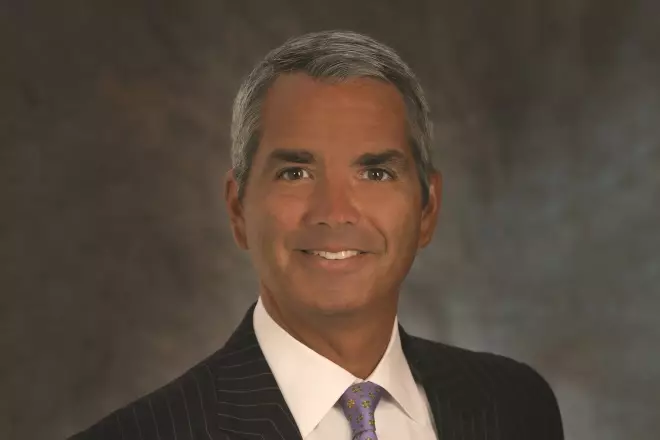
Source: Courtesy of Christopher Anzalone
Christopher Anzalone, chief executive officer of Arrowhead Pharmaceuticals, says that, initially, people got excited that RNAi was going to transform medicine but just a few years later and the industry that had sprung up around this discovery had crashed
This was when the industry “crashed”, says Anzalone, and it was “because the world realised: actually this is hard and there’s an awful lot of questions in this brand-new technology that we need to answer”. While so-called ‘naked’ RNA molecules have the potential to cause an immune response when injected, they are also fragile molecules, easily degraded in the body and they need to be delivered to the right cells. “Any drug development effort is a huge challenge. When you’re trying to deal with a new platform the challenges are significantly greater,” says Martin. He adds that the first ten years and US$1bn of funding at the company was spent tweaking the chemistry of the RNA molecules to “turn them into drugs”.
The rollercoaster ride of RNAi discovery and development

Source: Arne Dedert/DPA/PA Images
1998 US geneticists Craig Mello (right) and Andrew Fire (centre) discover that when double stranded RNA (dsRNA), called small interfering RNA (siRNA), is injected into worms, it switches off the corresponding gene, which leads to the identification of RNA interference (RNAi) as a whole new cellular pathway.
2002 It is established that RNAi is a pathway common to mammals. One of the biggest RNAi companies, Alnylam, is founded.

Source: Shutterstock.com
2004 The first clinical trial of an RNAi is conducted in patients with wet age-related macular degeneration.
2005 Novartis agrees to purchase almost 20% of Alnylam’s stock.
2006 Mello and Fire win the Nobel Prize for Medicine and Physiology for their work, and Merck purchases biotechnology company Sirna for US$1.1bn.
2007 Roche purchases just under 5% of Alnylam’s stock and RNAi company, Dicerna, is founded.
2008 A phase III trial of RNAi in wet age-related macular degeneration is terminated because of a lack of efficacy.

Source: Shutterstock.com
2010 Novartis and Roche announce that they are discontinuing their partnerships with Alnylam, and Roche discontinues investment in RNAi research.
2011 Arrowhead Pharmaceuticals buys Roche’s RNAi research.
2012 Alnylam discovers that a sugar molecule called N-acetylgalactosamine is key to getting RNAi into liver cells.
2014 Sanofi Genzyme enters into a deal with Alnylam, but Merck announces it is selling the company Sirna, which Alnylam subsequently buys.
2016 Alnylam reports an “imbalance of deaths” in a phase III study for a drug called revusiran, designed to treat hereditary transthyretin amyloidosis, and development is subsequently discontinued. Dicerna scraps the first two of its drugs to make it to clinical trials because preliminary results do not meet the company’s expectations, and the US Food and Drug Administration refuses to grant approval for further clinical trials of any of Arrowhead’s RNAi drugs because of unexplained deaths in chimpanzees. Arrowhead partners with Amgen.
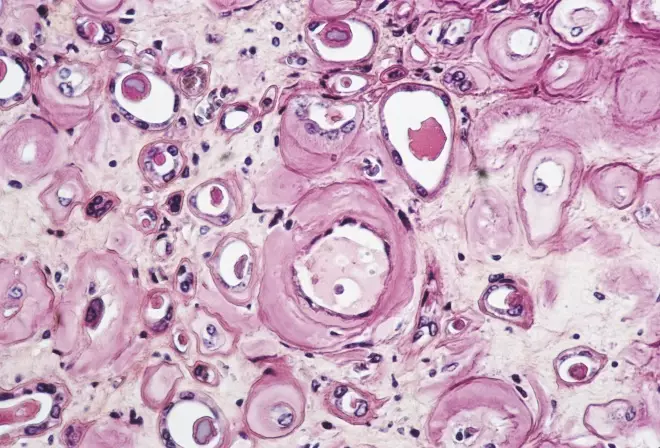
Source: Science Photo Library
2017 Alnylam’s drug patisiran is found to be effective and safe in a phase III trial for treating hereditary transthyretin amyloidosis (pictured) with neuropathy.
2018 Several of the key companies expect to start numerous clinical trials of new RNAi therapeutics.
A new focus
Bob Brown, chief scientific officer at Dicerna, says that “the biggest hurdle has always been delivery”. In 2010, the idea of using lipid nanoparticles started to gain traction as a way to protect the RNA molecules from degradation and also facilitate their transport across the cell surface. Kay, at Stanford, says that lipid nanoparticles mostly ended up in the liver because it is the organ responsible for first-pass metabolism, and also because liver cells have unique open fenestrations that allow large molecules to get close.
Having tried to explore a number of different diseases, we cracked the code for getting these molecules into the hepatocytes in the liver and making sure that they remain active there
This new focus on the liver led to one of the most significant developments in the field when, in 2012, Alnylam made a breakthrough. “Having tried to explore a number of different diseases, we cracked the code for getting these molecules into the hepatocytes in the liver and making sure that they remain active there,” says Martin. That ‘code’ is a sugar molecule called N-acetylgalactosamine (GalNAc). GalNAc is the ligand for a receptor present only on the surface of liver cells. Attaching GalNAc to siRNA targets it to the liver and triggers internalisation. Alnylam subsequently “rationalised the targets we were looking at back to the liver” and the whole field turned its focus to the liver too.
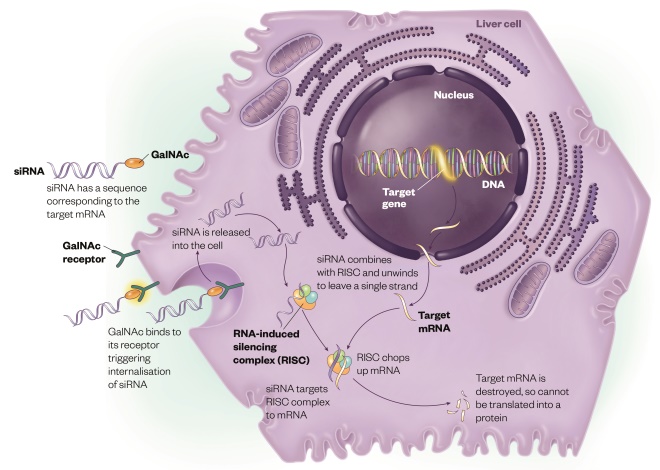
How RNA interference works
Source: Illustration by Alex Baker
By introducing small interfering RNA (siRNA) into a cell, a specific gene that drives disease can be targeted and silenced
With some progress being made, there was also a shift in the investment landscape. In 2014, Sanofi Genzyme entered into a deal worth US$700m with Alnylam. Another big pharmaceutical company decided to pull out of the area, however, with Merck announcing it was selling the company Sirna. This was to be to Alnylam’s advantage when it bought the company for US$175m, a drastic reduction in value compared with eight years earlier.
Now, Alnylam, Dicerna and Arrowhead all have their own patented methods of conjugating GalNAc to siRNA, and between them they have ten drug candidates in clinical trials. But it was the long awaited announcement of positive phase III results that has really buoyed the field. In September 2017, Alnylam’s drug patisiran was found to be effective and safe for treating a rare genetic disease. Madhu Lal-Nag, a molecular oncologist at the National Center for Advancing Translational Sciences at the National Institutes of Health who was not involved in the research, says this has been one of the most significant developments for the field. “It’s made people a lot more optimistic,” she says.
Patisiran treats a disease called hereditary transthyretin (TTR) amyloidosis with neuropathy. The disease stems from a mutation in the protein that transports vitamin A around the body, causing deposits of amyloid in the nerves, heart or eyes, depending on the specific mutation the patient has. The majority of the faulty protein is produced in the liver and patisiran is an siRNA designed to silence its production. “The therapeutic hypothesis was that if you weren’t making any more, if you were turning off the tap that was supplying more and more of this faulty protein, your body would have the chance to deal with some of the amyloid that had deposited,” says Martin.

Source: Courtesy of Brendan Martin
Brendan Martin, the general manager of Alnylam Pharmaceuticals for the UK and Ireland, says that RNAi-based therapies could help to treat previously untreatable diseases at very low doses and potentially before they even emerge
In all, 225 patients were enrolled in the 18-month study and those who received patisiran saw symptoms of neuropathy improve compared with baseline, whereas patients who received placebo had a worsening of neuropathy (P<0.00001). No significant safety concerns were identified. Martin says the results proved the therapeutic hypothesis “a bit beyond our expectations”. Biopsies indicated some clearance of amyloid in the nerves and indicators suggested recovery of function and quality of life. “It’s very unusual in peripheral nerve disease that you can actually see people recover,” he adds. The drug is currently with the US Food and Drug Administration (FDA) awaiting approval.
Delivery systems
Despite the success of patisiran, it does not showcase some of RNAi’s potential advantages. Patisiran uses Alnylam’s older lipid nanoparticle delivery system, which does not capitalise on the potential for using very low doses of siRNA. Frequent intravenous infusions are needed, which come with an increased risk of infusion reactions. Patients therefore need to be predosed with steroids and antihistamines. In contrast, formulations using GalNAc can be delivered by subcutaneous injection at much larger intervals. Martin says that, with the next generation of GalNAc technology, it may be possible to treat patients with only two subcutaneous injections per year. Patisiran, on the other hand, has to be dosed every three weeks.
Every other drug coming through the pipeline uses the company’s second-generation GalNAc technology, and a couple of candidates are already in phase III trials. This includes the drug givosiran for treatment of another rare genetic disease called acute hepatic porphyria. This is caused by a fault in haem synthesis, the oxygen carrying component in red blood cells, which leads to a build-up of toxic intermediates. Patients can experience severe pain and neurological symptoms. Some forms can even be triggered by sunlight, which Martin says “is supposed to be responsible for the legend of the vampire”. Current treatments are the administration of haem or a liver transplant. However, Anylam is not only focusing on rare diseases — another drug is in phase III trials for haemophilia and one of the four drugs at an earlier stage of development is for the treatment of high cholesterol by targeting the enzyme PCSK9.
Dicerna has also developed a drug against a rare liver disease called primary hyperoxaluria. Oxalate is a normal byproduct of an enzyme in the liver which is excreted in the kidneys. But mutations can cause a build-up of excessive amounts of oxalate that precipitates with calcium in the kidney, causing hard deposits. Outcomes can be severe, with some patients needing a kidney and liver transplant. Current treatments involve drinking extreme volumes of water and, in a small subset of patients, vitamin B6 injections seem to slow the disease, says Brown.
What our therapy would do is effectively give the patient a liver transplant chemically
“What our therapy would do is effectively give the patient a liver transplant chemically,” he says, explaining that the enzyme lactate dehydrogenase A (LDHA), which produces oxalate, would be “shut down” in the liver. In a healthy person, however, the enzyme has an ordinary function that would be lost in these patients. Brown says this does not appear to be a problem. “In this case we were able to specifically find documented and well-characterised examples of human beings that had no LDHA in their entire bodies because they were missing both copies of the gene,” he says, and “those patients show no effects in their liver at all”.

Source: Courtesy of Bob Brown
Bob Brown, chief scientific officer at Dicerna, says that the successes that have been observed with RNAi in the liver are giving Dicerna confidence to look at other tissues
A phase I study of the drug began in December 2017 in the UK, but the first results are yet to be released.
Trial failures
It has not all been plain sailing, howver. Both Dicerna and Alnylam have had their fair share of clinical trials that have not gone as hoped. In 2016, the industry suffered another blow when Alnylam reported an “imbalance of deaths” in one of its phase III studies, with 16 deaths in the treatment arm compared with 2 deaths in the placebo arm. The drug, called revusiran, was also designed to treat hereditary TTR amyloidosis, but this time it was aimed at the cardiac phenotype. Martin says that in the relatively small study the results could be down to chance, but an effect of revusiran could not be ruled out. Alnylam subsequently discontinued its development.
The failure did not cause the company to significantly change tack. Revusiran used the company’s first-generation GalNAc, whereas other drugs in the pipeline are using the second-generation technology, which has ‘enhanced stabilisation chemistry’ that increases the potency and durability of the drug. This means, says Martin, that “one year of exposure to revusiran is equivalent to approximately 140 years of exposure for ALN-TTRsc02” (another drug for hereditary TTR amyloidosis in the pipeline that uses the second-generation technology).
Dicerna also scrapped the first two of its drugs to make it to clinical trials. Both of these used lipid nanoparticle formulations — one was designed to target solid tumours and the other was designed to also treat primary hyperoxaluria. In a statement, the company said that preliminary results did not meet the company’s expectations. Dicerna is now also focusing its efforts on using its GalNAc technology called GalXC.
Arrowhead has also had its share of difficulties — at the end of 2016 the FDA refused to grant approval for further clinical trials of any of the drugs it had developed on account of unexplained deaths in chimps. This forced the company to also focus on its own GalNAc platform but it has quickly rebounded with two drugs now in clinical trials — one for hepatitis B and one for a rare genetic disease — and expects to have three more before the end of 2018. Anzalone is optimistic. Arrowhead recently partnered with Amgen in a deal worth potentially US$617m and Anzalone says the investment environment has “really changed substantially”.
Golden age
Given the number of setbacks, the field appears to have recovered from its difficulties. “We are entering, I think, a golden age of RNAi where we have solved all of these issues and now have, we think, an extraordinarily safe way to silence target genes and very specifically,” says Anzalone. This at least applies to the liver, in which he believes “we can really develop a lot of medicines to treat various diseases”.
We are entering, I think, a golden age of RNAi where we have solved all of these issues and now have, we think, an extraordinarily safe way to silence target genes and very specifically
But the field may soon be taking its first steps into new territory. Brown says the successes that have been observed in the liver are giving Dicerna confidence to look at other tissues. Arrowhead is moving this idea forward and is expecting to have an RNAi therapy for a lung disease in clinical trials by the end of 2018. “We see the next steps in this golden age of RNAi as taking this outside the liver because there are plenty of diseases that could be addressed in other cell types,” says Anzalone.
After 16 years of trying to develop therapeutics, RNAi may finally be about to have its day. Although, according to Martin, this might have to be shared with the other platforms that tinker with our genes. “There are number of advanced therapies now, like gene therapy, gene editing … and RNAi, where you are blocking the expression of genes through one mechanism or another,” he says.
Anzalone believes the story of RNAi in some ways reflects the rough start that monoclonal antibodies had. Both and he and Martin are confident that it could have an equally happy ending. “I think those classes of medicines will be at least as important in 20 years’ time as monoclonal antibodies are today,” says Martin.
References
[1] Fire A, Xu S, Montgomery MK et al. Potent and specific genetic interference by double stranded RNA in Caenorhabditis elegans. Nature 1998;391:806–811. doi: 10.1038/35888
[2] Elbashir SM, Harborth J, Lendeckel W et al. Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. 2001. Nature 2001;411:494–498. doi: 10.1038/35078107
[3] McCaffrey AP, Meuse L, Pham TT et al. Gene expression: RNA interference in adult mice. Nature 2002;418:38–39. doi: 10.1038/418038a
[4] Haussecker D. The business of RNAi therapeutics. Mol Ther Nucleic Acids 2012;1:e8. doi: 10.1038/mtna.2011.9
[5] Yang Z, Stratton C, Francis P et al. Toll-like receptor 3 and geographic atrophy in age-related macular degeneration. N Engl J Med 2008;359:1456–1463. doi: 10.1056/NEJMoa0802437