3D4Medical.com / Science Photo Library
In 1714, the British government offered a £20,000 incentive for the solution to what was then the greatest scientific challenge of the century — to develop a method to determine the longitude of a ship in just 30 minutes.
The prize was won by a self-educated clockmaker called John Harrison with his invention of the marine chronometer, which went on to revolutionise the safety of long distance sea travel.
Three hundred years later, in November 2014, the Longitude Committee reconvened to launch a new prize, based on one of the biggest challenges of the modern era — antibiotic resistance. The topic was decided by the public from a selection of six, which also included flight, food, paralysis, clean water and dementia.
To be in with a chance of winning the now £8m prize, teams have until 30 September 2019 (or until a winner is chosen with entries assessed every four months) to develop a rapid point-of-care diagnostic test that will help prevent the overuse and misuse of antibiotics (see Panel 1).
Here, we showcase four of the teams competing for the prize who are developing tests that could end up being used by pharmacists — each of these teams has received a Discovery Award to help them develop their ideas further. Discovery Awards are small seed grants that are given to promising competitors who may not be able to access other sources of funding or are working on a particularly novel idea. So far, there have been three rounds of the awards, with 29 teams receiving a grant.
Panel 1: The Longitude Prize criteria
Time to develop test: five years
The test must:
- Improve the targeted use of antibiotics for common globally-occurring infections;
- Improve antibiotic treatment decisions and improve on currently available diagnostic approaches;
- Be accurate enough to eliminate harmful treatment decisions, inform more targeted antibiotic use and give users the confidence to act upon the results;
- Be affordable for purchase and use in its intended global market;
- Give results in less than 30 minutes;
- Be suitable for point of care in all global healthcare settings;
- Be minimally reliant on healthcare resources;
- Be easy to use and interpret;
- Have a feasible business plan for full-scale manufacture and global distribution;
- Not infringe on the intellectual property rights of others;
- Have benefits that outweigh the risks.
Tests with an in-built data recording and transmitting capacity will be favoured but this is not essential to win the prize. The test must be an optimised prototype with a set design that is ready for performance evaluation in preparation for regulatory approval.
Module Innovations
Aim of test: rapid identification of UTI-causing uropathogens

Source: Courtesy of Module Innovations
Team name: Module Innovations (pictured from left to right: Rahul Chaudhari, Usman Khan, Maya KV and Sachin Dubey; not pictured: Mohit Dubey, Prajyot Gandhi)
From: Pune, Maharashtra, India
The idea for Module Innovation’s test came about when its chief executive and co-founder Sachin Dubey’s pregnant sister-in-law got a urinary tract infection (UTI). It took almost three days for the organism causing the infection to be identified and for her to be treated. But, according to Dubey, this is not unusual in India.
“Being in a city environment it is a bit easier to get access to culture [to help identify the bacteria], but if you go into rural areas of India, it is almost impossible,” he says.
“So with this in mind we started to develop USense.”
It’s the size of a credit card, with four wells in each corner, each representing the four uropathogens
USense is a handheld, diagnostic platform that allows for the rapid identification of UTI-causing uropathogens.
“It’s the size of a credit card, with four wells in each corner, each representing the four uropathogens [Escherichia coli, Staphylococcus aureus, Klebsiella and Enterococci],” explains Dubey.
The urine sample is dropped into the central well on the card which then flows to each of the four corner wells. The credit card-sized strip is made up of colour changing nanofibers that are able to detect four different kinds of bacteria.
“In almost 30 minutes, a simple colour change from blue to red [in one of the corner wells] enables you to identify which uropathogen is causing the UTI.”
Dubey says the test is currently 90% accurate but that he and his team are hoping to eventually achieve 98% sensitivity. Otherwise, he believes they have already met many of the prize criteria.
“The test is rapid, it’s portable, it doesn’t need any instrumentation and it works at the point of care.
“The only challenge I see is in meeting the criteria regarding sensitivity, but as we do larger scale validation the picture will become clearer.”

Source: Christopher Ratcliffe; Courtesy of Nesta
The urine sample is dropped into the central well on the USense device and then flows to each of the four corner wells
Dubey says tests such as theirs need to be validated in different geographies and settings. However, he notes that people in the UK and in India have different opinions about USense only being able to identify the bacteria and not the antibiotic needed.
“In India, people are requesting that this test has the potential to identify the antibiotic, but in the UK, doctors have a very positive view of this test, as rapidly knowing the target means they can start the medicine earlier,” he says.
Dubey explains that the problem of antimicrobial resistance is quite different in India because patients can easily get antibiotics over the counter, resulting in long-term misuse.
As a result, he is hoping that the test will be used to empower clinicians, not patients, to quickly identify bacteria and prescribe the correct medicine.
“We don’t want to make it available to the users and have them then to go to the pharmacy to buy the medicines,” he says.
The low cost of this test, which is expected to be around £2, is also crucial to drive its use in India and other developing countries, he points out.
Dubey says he is optimistic that by the end of October 2018, his team will have validated prototypes ready for submission.
The team is also planning to expand the capabilities of USense by developing an artificial intelligence-powered telephone app, which uses the phone camera to determine the bacterial load present in urine. The aim is to enable doctors to determine the appropriate dose of a particular antibiotic.
“UTIs are a global problem, with about 150 million cases happening every year,” says Dubey.
“It’s not just for countries like India — a lot of developed countries would benefit from USense.”
Rapid AMR Detection Team
Aim of test: antimicrobial susceptibility
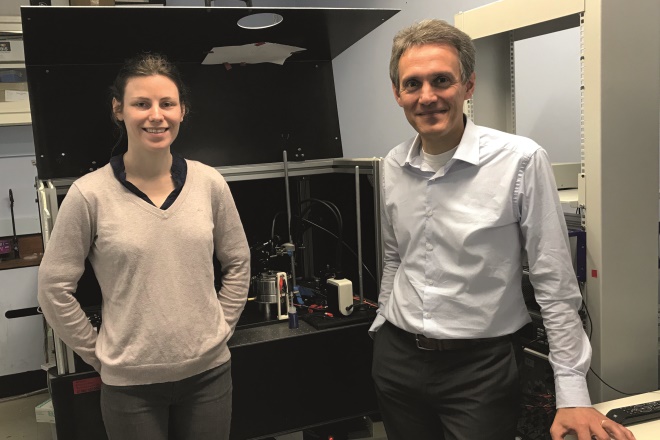
Source: Courtesy of Massimo Antognozzi
Team name: Rapid AMR Detection Team (pictured: Charlotte Bermingham, Massimo Antognozzi. Not pictured: Matthew Avison, Ruth Oulton, Krishna Coimbatore Balram, Helen Baxter and Niamh Redmond)
From: Bristol, UK
Three years ago, a research group in Switzerland, led by Sandor Kasas, made a fascinating discovery. Using tiny force sensors, they found that they could detect vibrations, known as nanoscale fluctuations, from bacteria that indicated that they were alive and active.
Because bacteria are so miniscule, these vibrations were previously unknown to the microbiology community since no optical system had been developed to see them.
“The way [Kasas’s team] visualised this was in an indirect way by absorbing the bacteria on to a mechanical microsensor and looking at the microsensor as a microcantilever [a mechanical element capable of detecting small forces acting on it] that vibrates,” explains Massimo Antognozzi, one member of the rapid antimicrobial resistance (AMR) detection team from the University of Bristol.
“They found that if the bacteria were alive, the microsensor would have a very noisy signal … but when the bacteria were treated with an antibiotic, the fluctuation would decrease significantly.”
This important discovery laid the foundations of the rapid AMR detection team’s project and, combining their expertise in nanotechnology, microbiology, engineering and biophysics, they set out to develop an optical technique to enable them to directly monitor the fluctuations from a single bacterium.
It’s like having a pair of glasses — it’s a very direct way of looking at these things
Unlike Kasas’ microsensor technique, Antognozzi’s team’s technique allows individual bacterium to be observed. As a result, in just a few seconds it is possible to see if the bacterium is vibrating, and therefore alive, or not vibrating, and therefore dead.
“All the microbiologists we’ve shown are very excited about it because they can see that there is information in the optical images that was not uncovered before.
“It’s like having a pair of glasses — it’s a very direct way of looking at these things,” says Antognozzi.
While groundbreaking for the microbiology community, it is also significant in terms of antimicrobial resistance because the aim of the test is to give healthcare professionals the ability to determine if an antibiotic is going to be effective. And this impact on patient care, says Antognozzi, is what motivates him the most.
“Yes, there is economic value to research but our drive is much more the impact on society — it doesn’t get mentioned very often but most people involved in this research will probably tell you the same,” he explains.
However, the team has come up against some significant challenges in its work, primarily because it has been carrying out the research in the physics department of the university.
“That means that we don’t have the biosafety level laboratory required to investigate pathogenic bacteria — so we are limited on the type of bacteria that we have been able to investigate so far,” explains Antognozzi.
“Fortunately, we have almost finished [producing] a dedicated piece of equipment that will go into the microbiology lab in the school of cellular and molecular medicine at the University of Bristol.
“Thanks to a very active collaboration with our colleagues from this school we hope we will be looking at a much larger number of pathogens.”
Antognozzi says that, from a theoretical point of view, there is nothing stopping the team from moving forward.
“There are a variety of things that are difficult to predict at the moment but we are on the path to achieve [what we want] and we have all the technology required, it’s just a matter of implementing it.”
The team plans to install a testing unit in a hospital within the next 12 months. Furthermore, the University of Bristol has now created a spinout company, called Vitamica, with the aim of commercialising the technology.
Going Against the Flow
Aim of test: sepsis detection

Source: Courtesy of David Anderson
Team name: Going Against The Flow (pictured from left to right: David Anderson, Riya Palchaudhuri, Mary Garcia. Not pictured: Suzanne Crowe, Clovis Palmer, Shirley Vallance and Steve McGloughlin)
From: Melbourne, Australia
Sepsis is a rare but serious complication of severe infections and, without rapid treatment, it can quickly lead to multiple organ failure and death. The speed at which the infection leading to sepsis is detected is therefore critical in determining whether a patient survives.
At the Burnet Institute, in Melbourne, Australia, which focuses on global health and infectious disease, David Anderson and his team are developing a test to speed up sepsis diagnosis.
“Sepsis is a big problem throughout the world,” explains Anderson.
“While hard to manage in the first world, it’s completely unmanageable in the third world as healthcare workers don’t have the training and biochemical tests to help identify people with sepsis — as a result people just die.”
The team initially set out to produce a diagnostic test for the developing world. However, by chance it ended up with a discovery that could lead to a test that is more accurate than any sepsis test that currently exists in developed countries.
According to Anderson, for more than a decade one leading test for sepsis has been based on flow cytometry, a complicated technique requiring a trained operator, which is used to analyse the physical and chemical characteristics of particles in a fluid as it passes through a laser. The test measures a protein, called CD64, which can be found on the surface of neutrophils, a type of white blood cell.
“It is well accepted by everyone that CD64 increases on the surface of neutrophils during sepsis or severe infections but in many published papers and in tens of thousands of patients, [flow cytometry] only works 80% of the time,” says Anderson.
Instead, the Australian team is developing a lateral flow test, a simple device used to detect the presence of a particular molecule in a sample. The technique involves dissolving blood samples in detergent, revealing everything that is present in the solution. Through this, the team made an important discovery about the CD64 protein.
“We found that there was a hidden population of CD64 inside the neutrophils [as well as on the surface], which the previous test was unable to detect in roughly 17–20% of patients,” explains Anderson.
“[This] meant that we went from a test that worked 80% of the time to something that appears to work 97% of the time,” he says.
This meant that we went from a test that worked 80% of the time to something that appears to work 97% of the time
“The biology of our test is well accepted in the field, it’s just that no one ever thought to look for why 20% of the patients are not reactive in the [traditional] test for sepsis.”
According to Anderson, the result is produced by measuring the level of CD64 protein and the level of a second protein, called neutrophil elastase, which is found in relatively constant amounts in neutrophils and so can help determine the number of neutrophils in the sample. If a patient has elevated levels of CD64 compared with the number of neutrophils, this may indicate sepsis or a severe infection.
Owing to the simplicity of the test, Anderson says it could be used by all “frontline healthcare workers”, from hospital doctors in the developed world to minimally trained healthcare workers in the developing world.
The proposed test is small and suitable for point of care and Anderson expects it will present a response in just 20 minutes. A main advantage for the team is that the Burnet Institute is based on a teaching hospital campus so it can work closely with clinicians in the hospital and also has access to a plentiful supply of fresh blood samples.
Despite the team’s successes, it is still facing some challenges. The main problem is that it does not yet have its own source of the key reagents needed for the test.
“There’s no use us developing a test with material that we can’t manufacture with,” explains Anderson.
“We’re working hard to get over that hurdle so we can have the right reagents in hand — once we have those we’re confident we will have our first prototypes by the end of 2018 and fully functional prototypes by mid-2019.”
Microplate
Aim of test: Antimicrobial susceptibility
Source: Courtesy of Damion Corrigan
Team name: Microplate (pictured: Damion Corrigan. Not pictured: Paul Hoskisson, Will Shu and Alan Faulkner Jones)
From: Glasgow, UK
Damion Corrigan’s team of experts from Strathclyde in Glasgow is attempting to shrink the hospital microbiology laboratory on to a single microchip. Their aim is to develop a rapid test to determine the susceptibility of bacteria to antibiotics.
The team includes a leader in 3D and biological printing, a biomedical engineer, a microbiologist and an intensive care consultant. Corrigan, an expert in developing biosensors, explains that their approach is to shrink the traditional disc diffusion test — a test that uses antibiotic discs to assess the extent to which bacteria are affected by a particular antibiotic – on to a “lab on a chip”.
“The interesting part about the techniques we have chosen is that they are mass-manufacturable — the kind of techniques that make the microchips in an iPhone,” says Corrigan.
What’s more, the test has been designed to take any clinical sample, including blood, urine and sputum.
“A lot of the problems with biosensors arise from handling the sample and extracting the bacterial DNA — it’s quite difficult — whereas this approach can handle any kind of sample [and the DNA does not need to be extracted],” explains Corrigan.
He says he envisages the test to be primarily pharmacy-based.
“You see your GP in the morning, leave the sample with the pharmacist, then, after lunch or work, the pharmacist will call you to let you know if you need an antibiotic,” he explains, adding that research looking at routine infections has shown that delaying an antibiotic by 24 hours after a patient reports feeling unwell does not impact the final clinical outcome.
You see your GP in the morning, leave the sample with the pharmacist, then, after lunch or work, the pharmacist will call you to let you know if you need an antibiotic
“It’s actually OK to have that wait of a working day or morning to make sure that you’ve got the correct antibiotic,” he says.
Corrigan also sees the test being used in intensive care.
“Intensive care is a well-known area for the evolution of drug resistance,” he says. “When someone comes in with signs of an infection, they will almost certainly be given a broad spectrum antibiotic immediately and with good reason — they don’t have time to perform a test and also they have to wait for 12–72 hours for a result from the hospital laboratory.”
He adds: “We’re hoping that the test can be located at the bedside and that it will allow doctors to switch from a broad spectrum agent to the right drug quite quickly.”
The test could be positioned anywhere along the clinical workflow, he explains, “anywhere that you can afford to wait two to three hours to make sure that you have the right drug”.
Corrigan says that one of the main advantages of the test is that, at under £3 per test, it is cheap and highly sensitive owing to the tiny sensors. However, he adds that, compared with some of the other teams competing for the prize, his team is behind in its development.
“We’re a new team and some of the other teams are much more established — we’re definitely playing catch up.”
One of the biggest hurdles left is to improve the time to result.
“We’re really having to extend the limits of the sensitivity of our sensors to detect the bacteria,” explains Corrigan.
“Ideally, people would want a 10-minute test so they can wait in the pharmacy for the antibiotic but we’re looking at the bacteria dividing and it takes at least 20 minutes for bacteria to divide — we’re going to find it difficult to beat that natural limit.”
“If we can get our result time to half an hour we’d be very competitive,” he adds.
Corrigan says the team intends to have a prototype ready by the end of 2018. It has just secured funding to employ a research assistant to evaluate the test as part of a six-month pilot study, which he says will be essential to finding out if the technology will give them an adequate time to result.
A difficult challenge
The Longitude Prize is coordinated by Nesta, a UK charity that aims to grow new ideas that can “change the world for the better”, and co-funded by Innovate UK, a non-departmental public body funded by a grant-in-aid from the UK government. Public health expert Daniel Berman leads the running of the prize at Nesta.
According to Berman, the challenge faced by the teams is anything but simple.
“The reason why there’s a prize is because the challenge is very difficult,” he says.
The reason why there’s a prize is because the challenge is very difficult
“So far we’ve had 12 teams who have submitted their prototypes to win the prize money — we screened their applications to check they were complete, and then sent them on to the judging panel,” he explains.
“None of the 12 came close to meeting all of the criteria.”

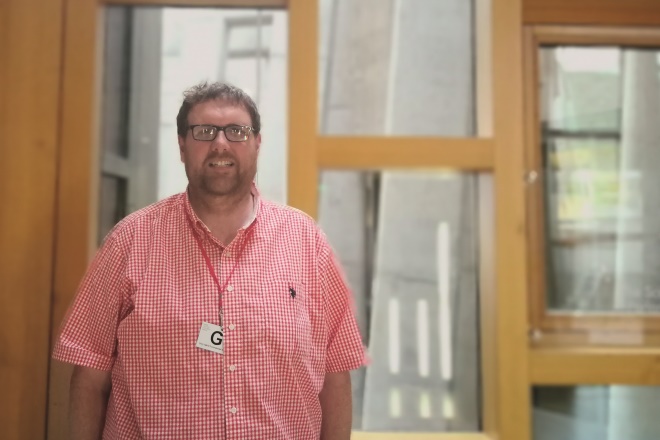
Source: Courtesy of Nesta
Daniel Berman, who leads the running of the prize at Nesta, believes the prize is already, in part, achieving its purpose by inspiring people all around the world to focus on the shared challenge of reducing resistance to antibiotics
The judging panel comprises 23 experts in diagnostic tests, antibiotic resistance and global health. It includes Dame Sally Davies, chief medical officer, and Francis Moussy, leader of diagnostics at the World Health Organization.
The current deadline for the prize is September 2019 but Nesta is open to an extension, says Berman.
“Our thinking is that we are open to keeping the competition going if necessary.
“No final decision has been made but we’re seeing quite a bit of progress and it would be a shame if no team makes it before the deadline.”
However, Berman believes the prize is already, in part, achieving its purpose by inspiring people all around the world to focus on the shared challenge of reducing resistance to antibiotics.
“It’s an exciting project to work on — there’s a lot of passionate, dynamic people and a lot of young researchers involved.
“I think having a prize makes them feel part of something.”
- On 1 June 2018, a correction was made to change the amount the winner of the Longitude Prize will receive from £10m to £8m, to reflect the fact that £8m will be awarded to the winner while £2m will be awarded to support promising entries along the way.


