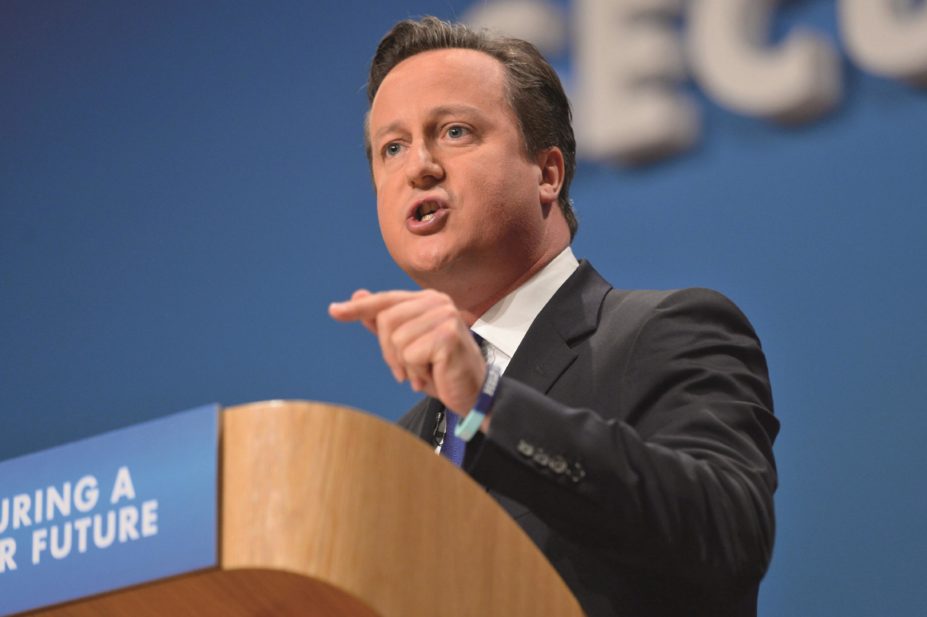
Ray Tang / Rex Features
Community pharmacists are taking patient referrals from GPs to treat common conditions in a pilot scheme that allows pharmacists access to patient records.
Some 16 community pharmacies and 18 GP practices are involved in the Extended Primary Integrated Care (EPiC) initiative, which will allow patients’ access to a GP or pharmacist from 8am to 8pm weekdays and for six hours on Saturdays and Sundays.
It is being funded with £1.8m from the Prime Minister’s challenge fund set up to look at ways of improving access to primary care services in the UK.
Details of the pilot scheme in Brighton and Hove, which was launched on 26 September 2014, were revealed as Prime Minister David Cameron promised UK voters access to a GP from 8am until 8pm seven days a week if the Conservative Party wins the next election.
“This absolutely fits in with what’s going on politically,” says Sue Oliver, an independent prescriber and community pharmacist, and consultant to the project which is being co-ordinated by the Brighton and Hove Integrated Care Service, a primary care federation.
“We have been saying for years that we should be more integrated in to the primary care team and this seems like the first time that we have been asked by GPs to help in this sort of initiative.”
Community pharmacists will offer one of three levels of care. Level one will give the pharmacist access to the patient’s medical record and the pharmacist will offer advice about medicines issues or review medication.
Pharmacists who deliver a level two service will be able to take referrals from GPs to treat ten common conditions such as eye infections or upper respiratory tract infections working to agreed patient group directions.
GPs, following a telephone triage, will refer patients for a 15 minute appointment with a pharmacist of their choice.
Pharmacists who are independent prescribers will be able to offer a level three service. This will involve taking GP referrals and holding community pharmacy clinics for a wider range of common conditions that could require treatment with a prescription medicine.
“This could become a national model for the future,” says Oliver, who has previously held clinics within an independent pharmacy in a GP practice. “A lot of the appointments were taken by patients who didn’t need to see a GP and it gave GPs more time to deal with more complex cases.”
Daisy Farrell, EPiC’s acting project co-ordinator, explained that all pharmacy expenses — including for extra hours worked — will be met out of funds from the pilot scheme.
The initiative tests pharmacy as a new route into primary care, says Farrell. “It’s making pharmacy part of the integrated primary care team,” she says. “We will make sure that we collect the right data to show which areas are successful.”
Elizabeth Butterfield, a member of the Royal Pharmaceutical Society’s English Pharmacy Board, echoed this view. “I absolutely hope it will become a national model because it is the way forward for community pharmacy,” she says. “It’s creating more effective joint working so that the patient can access care more easily.”
She says the EPiC project is significant because it gives pharmacists access to the GP record, with patient consent, and allows them to add details of their consultation with the patient to the record.


