MarinaVladivostok / Wikimedia Commons
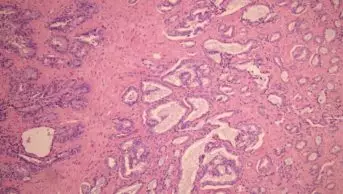
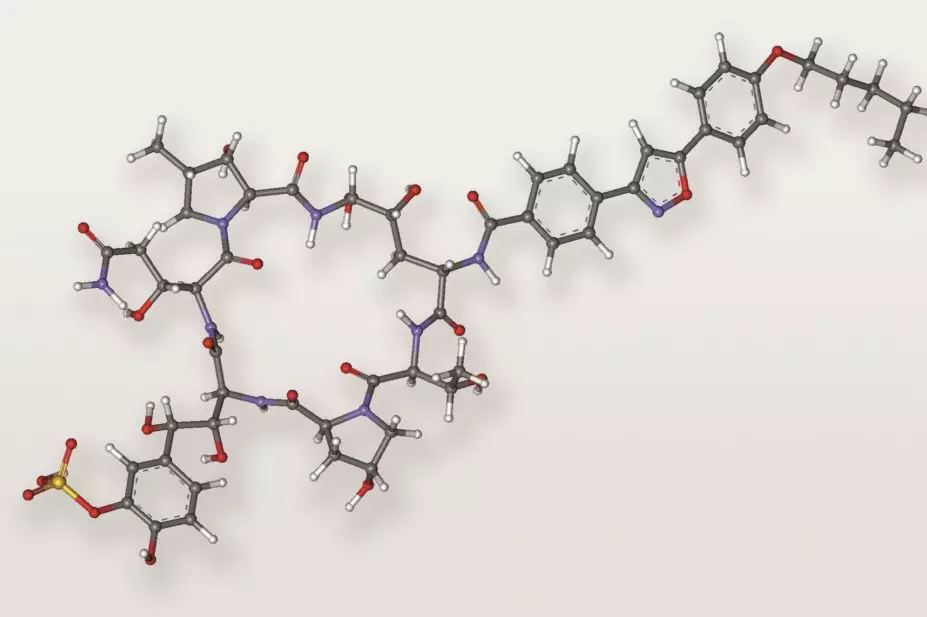
Micafungin is as effective at preventing fungal infections in leukaemia patients but is better tolerated than older formulations of posaconazole, interim results from a study suggested[1]
.
The research, presented at the American Society for Microbiology’s annual ICAAC meeting in Washington DC, showed that patients were much more likely to complete a course of treatment, at 71%, compared with 30% given posaconazole, partly because the drug was administered intravenously. Patients who experience severe mucositis due to chemotherapy often cannot swallow pills.
Genovefa Papanicolaou, a physician at Memorial Sloan Kettering Cancer Center in New York City, and colleagues conducted a randomised trial to test the feasibility of substituting micafungin, which is available in an IV formulation.
“I would not say micafungin is better, I would say it’s better tolerated, since the efficacy is the same,” noted Papanicolaou. “More and more patients get targeted inhibitors and aromatase inhibitors, and can’t take posaconazole due to abnormal liver function after chemotherapy or intractable vomiting.”
Posaconazole is considered standard prophylaxis for neutropenia-related fungal infections, and is now available in intravenous (IV) and liquid suspension formulations approved more recently than the oral form tested in the study. Although micafungin is approved in the US and Europe for prophylactic use in stem cell transplant patients, its use in leukaemia or myelodysplastic syndrome is off-label, Papanicolaou noted.
Subjects for the study had to be at least 18 years old with newly-diagnosed or first relapsed acute leukaemia (acute myeloid leukaemia or acute lymphoblastic leukaemia) or myelodysplastic syndrome. Individuals with prolonged QT intervals were excluded. The interim data come from 45 patients randomised to receive micafungin (100mg delivered intravenously daily) and 43 randomised to posaconazole (400mg twice a day), until the patient had recovered from the neutropenia, or for a maximum of 28 days.
“During this time, if the patient gets a fungal infection, abnormal fever or abnormal CAT scan, it’s considered a breakthrough of the prophylaxis, and preventive treatment stops,” explained Papanicolaou. It took those on micafungin a median of 12 days until treatment failed, compared with 6.5 days for those on posaconazole (P=0.0118).
According to the interim results, 21% of those who received micafungin needed recourse to empiric antifungal treatment, compared with 45% of those on posaconazole, Papanicolaou noted.
Gastro-intestinal (GI) conditions were markedly worse in those on the standard treatment: 7% of posaconazole patients had a GI adverse event, compared with none randomised to receive micafungin. And among those patients who discontinued the prophylactic agent early, GI toxicity was given as the reason in 16% of cases for those on posaconazole; no patients taking micafungin stopped for this reason, added Papanicolaou. However, the prevalence of colitis was roughly similar in both groups – 31% in the micafungin group, compared with 30% of those on posaconazole.
The trial, not yet complete, needs data from 114 patients for statistical purposes, and the researchers hope to have completed the study by early 2015. Funding for the study was provided by Astellas, manufacturer of micafungin.
References
[1] Huang Y-T et al. Micafungin versus posaconazole prophylaxis in adult patients with acute leukemia undergoing induction chemotherapy. [Presentation T-2033] American Society for Microbiology. Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington DC. 9 September 2014.