MedSci / Alamy Stock Photo
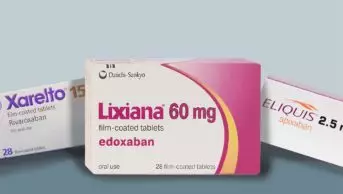
Patients prescribed antithrombotic drugs, such as low-dose aspirin, clopidogrel or warfarin, are at increased risk of having a subdural haematoma, research published in JAMA
[1]
(online, 28 February 2017) has confirmed.
The risk increases for older patients, especially those prescribed antithrombotics that belong to the vitamin K antagonist (VKA) class, including warfarin.
The researchers, led by David Gaist of the department of neurology at Odense University Hospital in Denmark, analysed data for around 10,000 people aged between 20 and 89 years who had been diagnosed with their first subdural haematoma between 2000 and 2015. They recorded whether patients were users of low-dose asprin, clopidogrel, a direct oral anticoagulant, such as dabigatran or rivaroxaban, or a VKA, and compared them with a control group made up of adults from the general population who were matched by age and sex.
“Antithrombotic drug use was associated with higher risk of subdural haematoma; and the highest odds of subdural haematoma were associated with combined use of a VKA and an antiplatelet drug,” say the researchers.
The results “add one more piece of evidence to the complex risk-benefit equation of antithrombotic drug use”, they add.
Among 10,010 patients with subdural haematoma (mean age 69.2 years), 47.3% were taking antithrombotic medications; low-dose aspirin was used by 26.7% compared with 22.4% in the control group; clopidogrel was used by 5.0% compared with 2.2% in the control group; a direct oral anticoagulant was used by 1.0% compared with 0.6% in the control group; and a VKA was used by 14.3% compared with 4.9% in the control group. All were associated with a higher risk of subdural haematoma.
When the researchers looked further they discovered that the risk was highest when a VKA was used at the same time as an antiplatelet drug (low-dose aspirin and a VKA: used by 3.6% of cases and 1.1% of controls; adjusted odds ratio [OR] 4.00, 95% confidence interval [CI] 3.40-4.70); clopidogrel and a VKA: used by 0.3% of cases and 0.04% of controls; adjusted OR 7.93, 95% CI 4.49-14.02).
Overall, subdural haematoma incidence increased from 10.9 per 100,000 person-years in 2000 to 19.0 per 100,000 person-years in 2015 (P<0.001 for trend). The largest increase was among patients aged over 75 years where the incidence rate increased from 55.1 per 100,000 person-years to 99.7 per 100,000 person-years (P< 0.001 for trend).
The researchers write: “In this case-control study… low-dose aspirin was associated with a small risk, use of clopidogrel and a direct oral anticoagulant with a moderate risk, and use of a VKA with a higher risk of subdural haematoma.”
Terry Dowling, principal pharmacist, haemostasis and thrombosis at Guy’s and St. Thomas’ NHS Foundation Trust in London, says the findings are further evidence of the association between anticoagulation, particularly with VKAs, and more recently with direct oral anticoagulants, and intracranial haemorrhage, including subdural haematomas.
“This study adds to and supports what is already known. It [also] brings robust evidence for the incidence of subdural haematomas on aspirin and clopidogrel therapy in particular.
“The results are unlikely to change current national or international guidelines about prescribing of antithrombotics because there is a wealth of evidence to support the benefits of these drugs in their respective indications,” he says. “The incidence of subdural haematomas has increased only in line with the increasing use of antithrombotics; there is no new highlighted risk/issue.”
References
[1] Gaist D, RodrÃguez LAC & Hellfritzsch M et al. Association of antithrombotic drug use with subdural hematoma risk. JAMA 2017;317(8):836-846. doi: 10.1001/jama.2017.0639