Shutterstock.com
The majority of patients with mild, persistent asthma who had a low level of eosinophils, showed no significant difference in their response to an inhaled corticosteroid (ICS) when compared to placebo, study results have shown.
Funded by the National Heart, Lung, and Blood Institute, the researchers carried out a 42-week, double-blind, crossover trial involving 295 patients with mild, persistent asthma who were at least 12 years old.
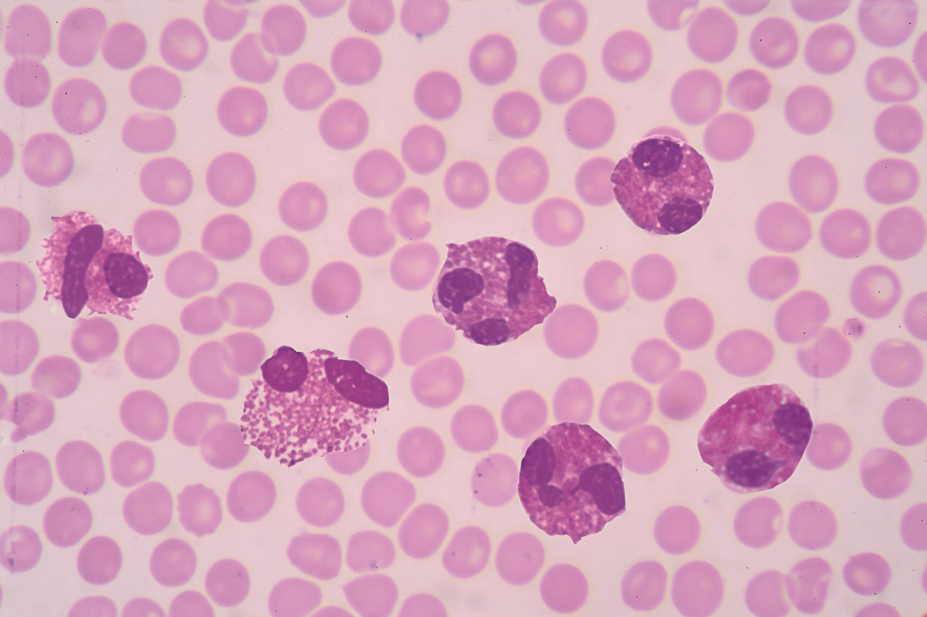
Each patient was categorised according to the levels of eosinophil in their sputum and assigned to either mometasone, an ICS; tiotropium, a long-acting muscarinic antagonist (LAMA); or a placebo.
More than 70% of the patients were characterised as having a low eosinophil level (a sputum eosinophil level of <2%).
The researchers found no significant difference in the response to the ICS or the LAMA in these patients, when compared with placebo.
It was found that 57% of patients had a better response when taking mometasone, while 43% had a better response to the placebo. Some 60% of patients taking tiotropium had a better response to the drug, while 40% had a better response to the placebo.
Patients’ responses were assessed by looking at “treatment failure, asthma control days and the forced expiratory volume in one second”, the study said.
However, in patients with a high eosinophil level (a sputum eosinophil level of ≥2%), 74% of patients taking mometasone had a better response to the drug, compared to 26% who had better symptom control while taking the placebo.
In contrast, for those taking tiotropium, 60% had a better response to tiotropium, whereas 40% responded better to the placebo.
According to the study, which was published in the New England Journal of Medicine (19 May 2019), the appropriate treatment for low eosinophil levels is currently unknown; however, the researchers said that their study added to a growing body of evidence that different patients with mild asthma should be treated differently.
Stephen Lazarus, professor of medicine at the University of California, San Francisco, and lead author of the study, said: “We’re intrigued by the results of this study and believe it raises questions about the way doctors manage mild persistent asthma.
“We’re not saying that steroids are unimportant for mild asthma, but our study does suggest that treatment guidelines should be re-evaluated for patients with mild persistent asthma who have low sputum eosinophils.”
Anna Murphy, consultant respiratory pharmacist at University Hospitals of Leicester NHS Trust, described the study as “interesting”, but said that the results were contrary to the new Global Initiative for Asthma (GINA) guidelines, which are in currently in draft form.
“From 2019, for safety, GINA no longer recommends starting with SABA [short-acting beta2 agonist]-only treatment. GINA recommends that all adults and adolescents with asthma should receive ICS-containing controller treatment, to reduce their risk of serious exacerbations and to control symptoms.
“Low-dose ICS markedly reduces asthma hospitalisations and death — for mild asthma an inhaler containing an ICS and formoterol is recommended for PRN use.”
She added that while others may argue that an individualised approach is required to manage patients, further studies were required as this study was limited by patient numbers and a short duration on each medicine.
“We do, however, know that the following are important in managing our patients with asthma: confimation that the diagnosis is of asthma; that inhaler delivery is optimised and technique checked regularly; that treatments are reviewed regularly and individualised for the patient; and that prescribing of SABA is minimal.”


