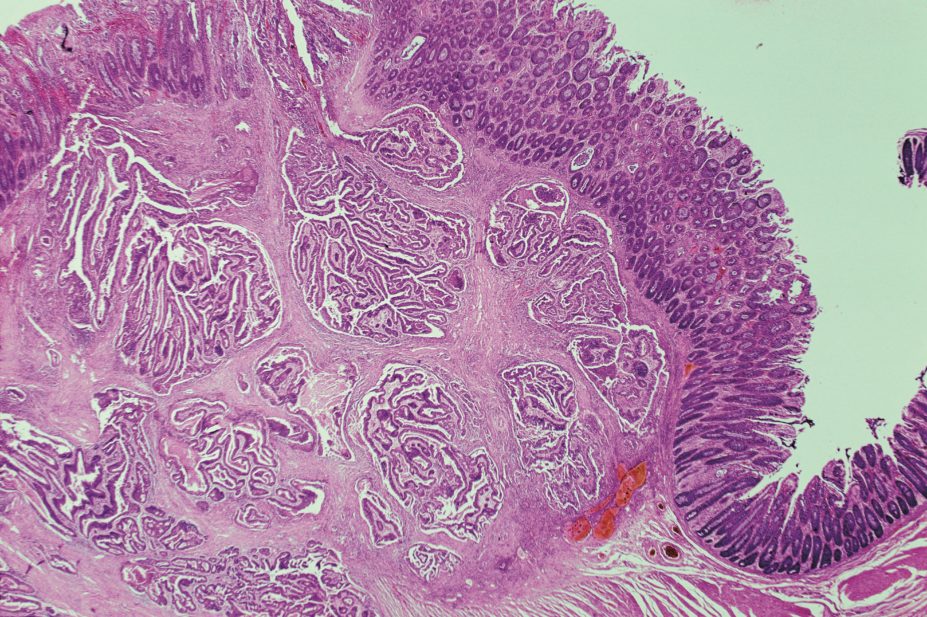
PHOTOTAKE Inc. / Alamy Stock Photo
Decreases in blood cholesterol that cannot be explained could be an indicator of undiagnosed colorectal cancer, according to research published in PLOS Medicine[1]
(online, 26 April 2016).
Researchers from the University of Pennsylvania, Philadelphia, analysed UK patient records to “disentangle” the association between statins, cholesterol and colorectal cancer, a relationship they describe as “complex”.
They believe their analysis suggests that the previously reported link between statin use and reduced risk of colorectal cancer may be explained by indication bias – the bias that results from treatment choices being made according to a patient’s disease severity or prognosis. The team conclude that statins should not be prescribed for the prevention of colorectal cancer.
“Although the risk of colorectal cancer was lower in statin users versus non-users, no difference was observed among those who continued versus discontinued statin therapy, suggesting the potential for indication bias,” say the researchers. “The association between decreased serum cholesterol and colorectal cancer risk suggests a cholesterol-lowering effect of undiagnosed malignancy.” They add that clinical judgement should be used when considering causes of cholesterol reduction in patients, including those on statin therapy.
The researchers based their conclusions on an analysis of the records of 22,163 patients with colon cancer and another 86,538 non-cancer patients. They compared statin use and blood cholesterol levels between the two groups and discovered a decreased risk of colorectal cancer with statin use (odds ratio [OR] 0.95 for long-term use; 95% confidence interval [CI] 0.91–0.99; OR 0.92 for short-term use; 95% CI 0.85–0.99).
The researchers went on to consider whether the link could be attributed to indication bias by examining data for a subgroup of patients, 5,102 of whom were prescribed a statin and 19,032 of whom discontinued their statin therapy. They found that the cancer risk between the two groups was not significantly different (OR 0.98; 95% CI 0.79–1.22).
The researchers also found that increased blood cholesterol was associated with a decreased cancer risk (OR 0.89 per mmol/L increase; 95% CI 0.87–0.91) but that the association only occurred if cholesterol was measured close to the time that the cancer was diagnosed.
Decreases in total blood cholesterol of more than 1mmol/L one year before cancer diagnosis were associated with subsequent colorectal cancer (OR 1.25 for statin users; 95 CI% 1.03–1.53; OR 2.36 for non-users; 95 CI% 1.78–3.12).
Sotiris Antoniou, consultant pharmacist in cardiovascular medicine at Barts Health NHS Trust in London, says some earlier trials have “reassuringly suggested a neutral effect” of statin use on overall cancer risk and some observational studies have “raised the possibility of an inverse association between statins and overall cancer risk, and risk of specific cancers including colorectal cancers”.
However, he points out that there are limitations in assessing cancer risk from meta-analyses of randomised controlled trials with insufficient follow-up duration and from observational studies.
“Despite the limitations, we are starting to get a consensus on the take home message: that there is insufficient evidence to recommend the use of statins for cancer prevention, but there is clear evidence of benefit in reduction of major adverse cardiovascular disease,” says Antoniou.
References
[1] Mamtani R, Lewis JD, Scott FI et al. Disentangling the association between statins, cholesterol, and colorectal cancer: a nested case-control study. PLoS Med 2016;13:e1002007. doi: 10.1371/journal.pmed.1002007