
Courtesy of Baguiasri Mandane
In June 2016, I embarked on a life-changing journey to the Gambia, located in the West of Africa, alongside a group of students and lecturers from De Montfort University and Global Hands UK, a non-profit organisation that aims to tackle global inequality.
While in the Gambia, we engaged in various humanitarian activities, from teaching science in secondary schools to building the second biggest library in the country with the philosophy to “teach people how to fish instead of giving them the fish”.
In this blog, I will focus on my clinical experience in one of the biggest healthcare facilities in the region, The Faji Kunda Community Hospital in Serrakunda.
Healthcare differences
The 24-hour Faji Kunda Health Centre consisted of: one female, one paediatric and one male ward; one operating theatre; two labour wards; one tropical and infectious diseases laboratory; and various clinics including family planning, postnatal, outpatient and walk-in consultation clinics.
Due to the high poverty rates in the country, there is a high level of demand for public health services. Only two doctors were available to cover the entire hospital. Neither of them were able to be present on site between 11am and 4pm and only one doctor was “on-call” for emergencies. Thus, all the clinics were run by nurse practitioners. Patients had to pay a sum of 25 Dalasis (approximately 42p) for each consultation. The medicines issued on the prescription, however, were free provided that the health centre’s pharmacy had them in stock. If they do not have them in stock, the patients would need to pay for the medicines and obtain them from private pharmacies.

Source: Courtesy of Baguiasri Mandane
Community Hospital’s Ambulance Service (one ambulance, covering the whole region)
Some of my other hospital colleagues and I were given an opportunity to help with various clinical tasks in the outpatient clinics, including taking patients’ blood pressure measurements. Upon discussion with the nurse practitioners it was clear that, despite having few resources, they were determined to provide the best clinical service for all their patients.
All the clinics were run by nurse practitioners
The pharmacy department
The pharmacy department was a small room with a dedicated and trained dispensary team. In the pharmacy, there were three trays of medicines, all of which were assembled in small plastic bags. The medicine bags were marked with a pen to help the patients remember the instructions, for example “Take TWO tablets THREE times a day” would be indicated on the bag as two lines, three times in a row.
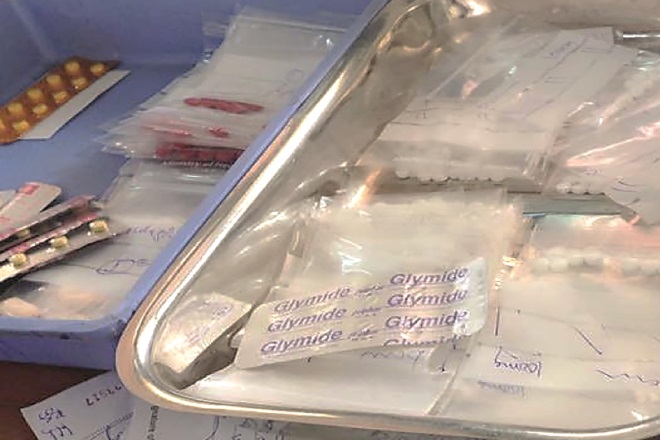
Source: Courtesy of Baguiasri Mandane
The pharmacy department in Faji Kunda Health Centre
Unfortunately, neither the wards nor the pharmacy department had any pharmacists. All the prescriptions would arrive at the pharmacy through a little hatch and the medicines would be given out by the dispensing assistants. Nonetheless, the dispensary staff informed me that the bigger health centres in the capital city would usually employ pharmacists for the clinical services.
Medicines management
During my time at the hospital, the pharmacy stores did not have a functioning fridge. Therefore, insulins had to be kept outside the fridge at room temperature (>30 degrees Celsius).
The facilities and limited resources made it difficult to fix problems in a timely manner. Additionally, medicines being unavailable or only available privately at high cost meant it was challenging to ensure that patients received the necessary treatment for their conditions.
The pharmacy stores did not have a functioning fridge. Therefore, insulins had to be kept outside the fridge at room temperature
Antimicrobial stewardship
More than 50% of the patients seen in the outpatient clinics were prescribed one or more antibiotic. Additionally, community pharmacies in the local villages sell antibiotics, including amoxicillin and doxycycline, over the counter without a prescription. I believe there is a need for further training around the antimicrobial stewardship.
The future
This humanitarian work was life changing and I would encourage others to do something similar. We owe it to humanity to help others around the world.
You may also be interested in
The importance of diverse clinical imagery within health education

Government should consider ways to prevent ‘inappropriate overseas prescribing’ of hormone drugs, review recommends
