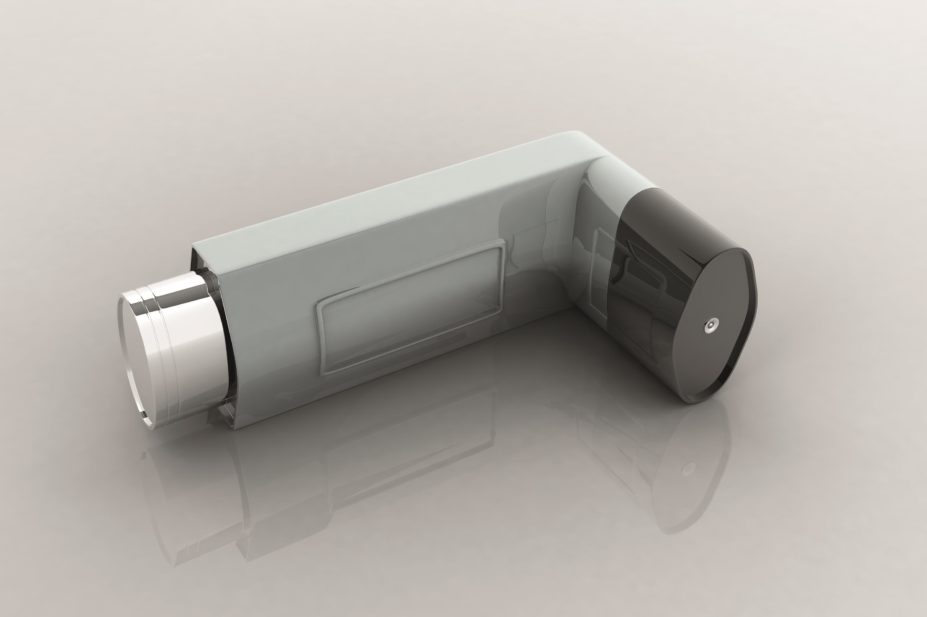
Shutterstock.com
After reading the ‘National review of asthma deaths report’, published in May 2014, I was surprised by how many of these were preventable.
In the report there is an analysis of how many short-acting beta agonist inhalers (SABA) were prescribed in the year before death. One patient was prescribed 112 SABA inhalers in that year. That equates to roughly two inhalers per week. Ten patients were prescribed more than 40 SABA inhalers in the year before death. These figures are shocking.
Based on the Scottish Intercollegiate Guidelines Network/British Thoracic Society guideline on the management of asthma, using a reliever inhaler more than three times per week is one sign of poor control. Therefore, six puffs per week (assuming two puffs per dose) could be considered the edge of control.
If we take a 200-dose salbutamol inhaler as an example, then using one inhaler more than every 30 weeks (assuming six puffs is used per week) could be deemed as overuse. Pharmacists would be justified in having a conversation with the patient if they spotted this level of SABA use. They may even choose to intervene and use the asthma control test to assess the level of control exhibited by that patient. A diligent community pharmacist who can spot the overuse of a salbutamol inhaler might just save a life.
I have met and worked with pharmacists who are enthusiastic about monitoring the frequency of the dispensing of hypnotics like benzodiazepines, and rightly so. These same pharmacists, however, seem happy to dispense a large number of SABA inhalers to patients without asking questions.
My perspective has shifted recently because I have completed my independent prescribing course. I am now concerned with the management of patients as well as the safe supply of their medicines. My clinical check covers the usual things such as dosage, contraindications, drug interactions, etc, but now I consider the diagnosis of the patient much more than before. I am interested in what evidence-based supportive intervention I can make to improve a patient’s control of his or her long-term condition.
A simple example of this in asthma is a check of inhaler technique. If a patient’s technique is poor with a metered dose inhaler, for example, I would prescribe a spacer device, especially if asthma control is poor. This is an example of a safe, evidence-based, patient-centred intervention.
By beginning to risk assess patients more thoroughly as they collect their medicines in the pharmacy, perhaps we can contribute to an improvement in the findings of the ‘National review of asthma deaths report’. After all, patients will always come to the pharmacy to collect their reliever inhalers but may not always attend their annual asthma review at the surgery. Community pharmacists could help identify these patients and assist in the management of their asthma.
Johnathan Laird is a community pharmacy manager and independent prescriber working in rural Aberdeenshire.


