JL / Alamy.com
Cardiovascular disease is the leading cause of mortality worldwide, accounting for around 17.7 million deaths per year[1]
. The leading risk factor for cardiovascular disease is hypertension, which affects around 1 in 4 people worldwide, and 12.5 million people in England[2]
. But only around 35% of people with hypertension in England are diagnosed and treated to recommended blood pressure levels[2]
. If just 15% more adults in England with hypertension were successfully diagnosed, the NHS could save around 7,000 quality-adjusted life years and approximately £120m in healthcare and social care costs[2]
.
Public Health England concedes that the nation’s performance on spotting and managing high blood pressure “is still a long way off”, compared with what has been achieved in other countries, such as Canada, where 65% of people with hypertension have a diagnosis and are treated to recommended target levels
[2]
. But, as most healthcare professionals know, hypertension can be treated easily with a combination of changes to lifestyle and medicines, and evidence suggests that pharmacists should be involved in care for the condition.
Realising pharmacists’ value
Other nations have already realised pharmacy’s value in this area
Simply put, pharmacists are both medication experts and the healthcare professionals most accessible to patients. As primary care professionals based in the community, pharmacists are in an ideal place to detect and manage hypertension, and they can play an important role because many patients do not see their GP for this asymptomatic condition.
Other nations have already realised pharmacy’s value in this area. The Canadian, European and American guidelines for hypertension all advocate pharmacists’ involvement in care[3]
. In my home country, Hypertension Canada — a non-profit organisation dedicated to preventing and managing the condition — has made engaging primary care pharmacists in hypertension care a national priority and is developing a certification programme in hypertension management.
Blood pressure
There is extraordinarily robust research evidence for the benefits of pharmacist care in hypertension. In a systematic review, Santschi et al. reported on 39 randomised trials of pharmacist care for people with hypertension and showed an average blood pressure reduction of 7.6/3.9mmHg, compared with usual care[4]
.
The odds of reaching the recommended target blood pressure was 2.3 times higher in the pharmacist prescribing group
Even greater effects have been demonstrated when pharmacists independently prescribe and care for patients with hypertension. In the Canadian RxACTION study[5]
, 248 patients with suboptimally managed hypertension were randomised to either pharmacist prescribing and follow-up (according to the Hypertension Canada guidelines), or usual physician care. In the pharmacist prescribing group, systolic blood pressure was 18.3mmHg lower compared with baseline (and 6.6mmHg lower than usual care) after six months — a statistically significant decrease. Furthermore, the odds of reaching the recommended target blood pressure was 2.3 times higher in the pharmacist prescribing group.
Risk of cardiovascular events
Our RxEACH study took the pharmacist care model in Canada one step further[6]
; more than 700 patients who were at high risk of cardiovascular events (including those with established vascular diseases such as heart attack or stroke), diabetes or chronic kidney disease, or who had a high Framingham Risk Score (a measure of cardiovascular risk) were randomised to either pharmacist prescribing or usual care. In the pharmacist prescribing group, pharmacists focused on managing hypertension, dyslipidaemia, glycaemic control and smoking cessation. After three months, the pharmacist care group showed a 21% greater reduction in risk for cardiovascular events compared with usual care. A systematic review and meta-analysis, involving more than 3,000 patients, has also shown community pharmacist-led interventions to significantly reduce blood pressure[7]
.
Cost savings
We also undertook a cost-effectiveness analysis based on the RxACTION study[8]
. After taking into account the costs to train and pay pharmacists to provide care, as well as extra medication costs — and balancing them with the expected downstream cost savings from reduced heart attacks, strokes and kidney failure — it was estimated that pharmacist involvement could save $CAD6,364 (£3,660) per patient over a 30-year period. From a population perspective, if only 50% of those with poorly controlled hypertension sought care from their prescribing pharmacist, the cost saving to society could be $CAD15.7bn (£9bn) over 30 years.
This prospect is even more exciting in the UK
These findings represent an extraordinary opportunity — pharmacist prescribing and care for hypertension is both better than usual care and saves money. This prospect is even more exciting in the UK, where the population is almost double that of Canada, and where rates hypertension control are half that of Canada.
Patients prefer pharmacists’ care
The patients in the RxEACH study were interviewed by a third party, so they could freely share their feelings about the care provided by their pharmacist[9]
. They expressed their appreciation for a strong relationship with their pharmacist, pharmacists’ deep compassion and caring nature, their ability to clearly explain complicated concepts, their accessibility, and their ability to collaborate with the patient’s physician. Patients expressed their high level of trust in their pharmacist, a high degree of satisfaction and a feeling of empowerment.
What pharmacists can do
To ignore this opportunity is to ignore our societal duty of care
Community pharmacists’ management of hypertension is a ‘no brainer’. Pharmacist consideration for hypertension and cardiovascular risk adds significant value to patients’ care — it is supported by strong evidence and cost savings to society, and patients prefer their support. To ignore this opportunity is to ignore our societal duty of care. While pharmacists in England present a strong case for managing hypertension, they are not yet supported and remunerated to do so. But the Pharmaceutical Services Negotiating Committee has suggested that contract negotiations will consider enhancing the role of community pharmacists in the management of long-term conditions, such as hypertension, during its negotiations of community pharmacy’s new contract.
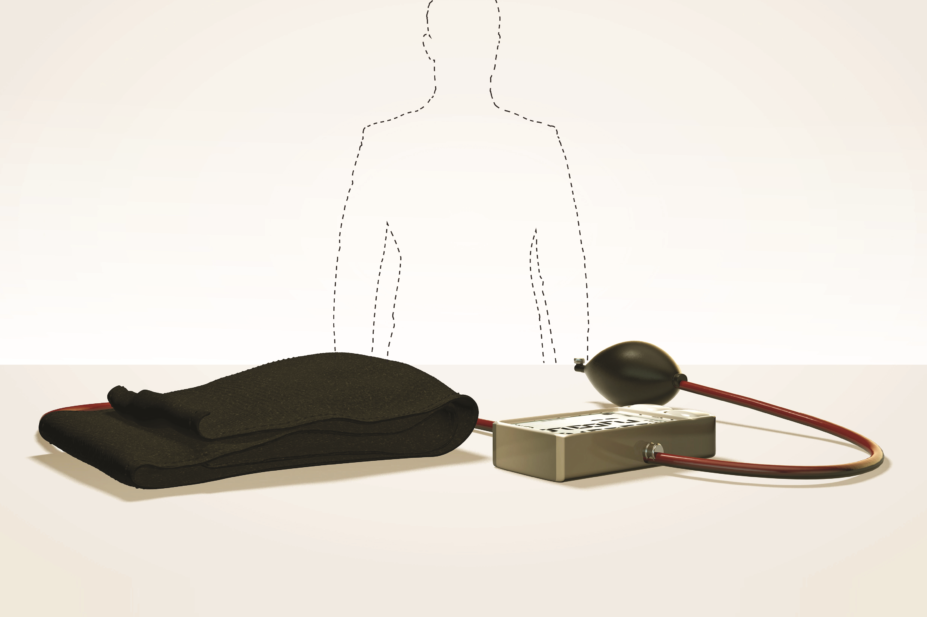
So what would pharmacist care for hypertension look like in practice? It would involve being proactive and practising to pharmacy’s full scope. Pharmacists could set up a system to conduct case-finding, to help them systematically identify patients with hypertension[10]
, and they should offer to check all of their adult patients’ blood pressure at least annually. Patients with known hypertension should have their blood pressure checked each time they come to collect their repeat prescription. Pharmacists could also advise patients on how to monitor their blood pressure at home, or perhaps implement a validated blood pressure kiosk in the pharmacy. They could educate their patients on hypertension and cardiovascular risk. Prescribers could take the responsibility to adjust doses and add complementary antihypertensive medicines (most patients will require at least two medicines to achieve recommended blood pressure levels). Importantly, pharmacists should schedule regular follow-up with patients to check their progress.
Community pharmacy in England is still waiting for its new contract, but it can begin to take responsibility for patients’ hypertension care. To get started, pharmacists should read hypertension guidelines from the National Institute for Health and Care Excellence and the British and Irish Hypertension Society[11]
,[12]
, and engage in conversations on hypertension with patients. Given the high prevalence and poor control of the condition in the UK, and pharmacists’ medication expertise, getting involved in cardiovascular risk reduction could be the most important thing pharmacy does for its patients and public health.
Ross T Tsuyuki, professor of medicine (cardiology) and chair, Department of Pharmacology; director, EPICORE Centre, Faculty of Medicine and Dentistry, University of Alberta
References
[1] World Health Organization. Cardiovascular disease. 2011. Available at: http://www.who.int/cardiovascular_diseases/en/ (accessed June 2019)
[2] Public Health England. Health matters: combating high blood pressure. 2017. Available at: https://www.gov.uk/government/publications/health-matters-combating-high-blood-pressure/health-matters-combating-high-blood-pressure (accessed June 2019)
[3] Anker D, Tsuyuki RT, Paradis G et al. Pharmacists to improve hypertension management: guideline concordance from North America to Europe. Can Pharm J (Ott) 2019;152(3):180–185. doi: 10.1177/1715163519839675
[4] Santschi V, Chiolero A, Colosimo AL et al. Improving blood pressure control through pharmacist intervention: a meta-analysis of randomized controlled trials. J Am Heart Assoc 2014;3(2):e000718. doi: 10.1161/JAHA.113.000718
[5] Tsuyuki RT, Houle SKD, Charrois TL et al. Randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: the Alberta Clinical Trial in Optimizing Hypertension (RxACTION). Circulation 2015;132(2):93–100. doi: 10.1161/CIRCULATIONAHA.115.015464
[6] Tsuyuki RT, Al Hamarneh YN, Jones CA & Hemmelgarn BR. The effectiveness of community pharmacist interventions on cardiovascular risk reduction: the multicenter randomized controlled RxEACH trial. J Am Coll Cardiol 2016;67(24):2846–2854. doi: 10.1016/j.jacc.2016.03.528
[7] Cheema E, Sutcliffe P & Singer DR. The impact of interventions by pharmacists in community pharmacies on control of hypertension: a systematic review and meta-analysis of randomized controlled trials. Br J Clin Pharmacol 2014;78(6):1238–1247. doi: 10.1111/bcp.12452
[8] Marra C, Johnston K, Santschi V & Tsuyuki RT. Cost-effectiveness of pharmacist care for managing hypertension in Canada. Can Pharm J 2017; 150(3):184–197. doi: 10.1177/1715163517701109
[9] Al Hamarneh YN, Lamb S, Donald M et al. Pharmacist prescribing and care improves cardiovascular risk, but what do patients think? A substudy of the RxEACH study. Can Pharm J (Ott) 2018;151(4):223–227. doi: 10.1177/1715163518779092
[10] Kassamali A, Houle S, Rosenthal M & Tsuyuki RT. Case finding: The missing link in chronic disease management. Can Pharm J (Ott) 2011;144(4):170–172. doi: 10.3821/1913-701X-144.4.170
[11] National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. Clinical guideline [CG127]. 2016. Available at: https://www.nice.org.uk/guidance/cg127 (accessed June 2019)
[12] British and Irish Hypertension Society. Guidelines. 2012. Available at: https://bihsoc.org/guidelines/ (accessed June 2019)