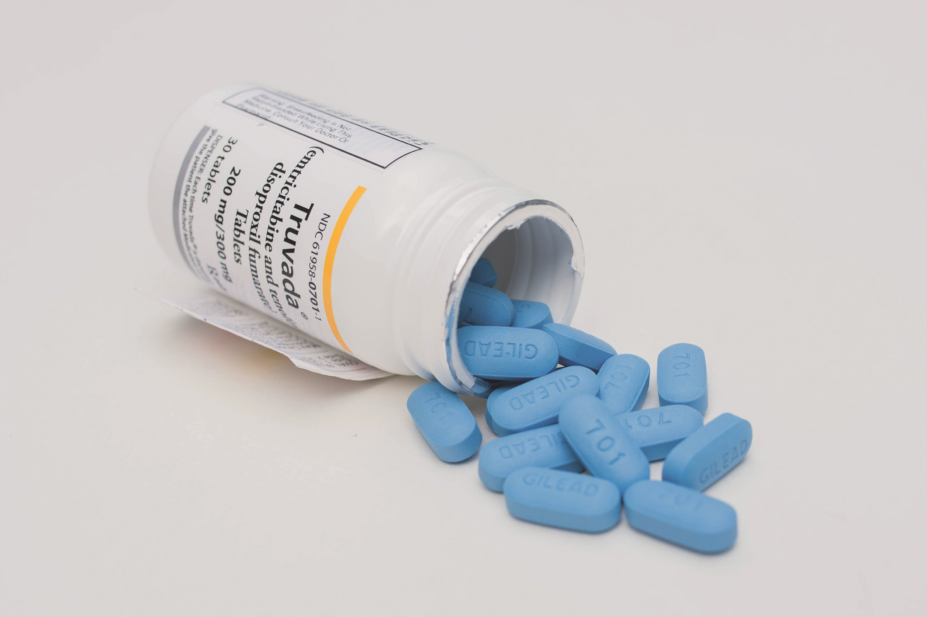
Shutterstock.com
Simply, pre-exposure prophylaxis (PrEP) works.
Numerous studies have shown that the PrEP pill is highly effective in preventing HIV transmission and the 2016 PROUD (pre-exposure option for reducing HIV in the UK: immediate or deferred) study showed that PrEP would be a cost-effective way to fight the HIV epidemic in the UK
[1]
.
As far back as September 2015, the World Health Organization recommended that “people at substantial risk of HIV infection should be offered PrEP as an additional prevention choice, as part of comprehensive prevention[2]
”.
However, access to PrEP remains inconsistent across the UK. In Scotland, PrEP has been routinely available via sexual health clinics since 2017; in Wales, people can access the drug through an uncapped trial; and there is now routine access in Northern Ireland.
But the NHS in England — the British nation accounting for the highest rates of new HIV infections — is still not providing routine access to the drug[3]
.
In October 2019, Matt Hancock, the secretary of state for health and social care, said: “The rollout from a trial to routine commissioning will happen [in England] in April [2020].” But with this milestone fast approaching, we have heard nothing about how this scheme will be implemented[4]
,[5]
.
PrEP in the UK
We at the HIV and sexual health charity the Terrence Higgins Trust have been fighting for increased access to PrEP in the UK since 2015. Despite this, it remains a missing permanent piece of the toolkit to end new HIV transmissions in England. We support the ‘Joint United Nations Programme on HIV/AIDS’ in eliminating new HIV transmissions by 2030, but, in England, limited access to PrEP undermines efforts to realise this goal[6]
.
Progress towards ending the epidemic is slowing down: according to the latest statistics from Public Health England, there were 4,484 new HIV diagnoses in the UK in 2018 — a 6% decrease in cases, compared with 2017, and a 29% drop since 2015[7]
. We now risk plateauing unless decisive action is taken to halt new transmissions.
There have been big advancements in our understanding of HIV; we now know that people on effective HIV treatment cannot pass on the virus. There is international evidence to show zero transmissions among couples — one of whom has HIV but is on effective HIV treatment, and the other who is HIV-negative. In the UK, 97% of people who are diagnosed and on treatment are virally suppressed, and there is zero risk of onward transmission[7]
.
The same progress must now be made in populations that continue to be at risk of HIV. PrEP is transformative for people at risk of HIV, and, compared with the cost of a lifetime of HIV treatment, it is a cost-effective intervention.
In May 2019, the pharmaceutical company Gilead relinquished is patent for PrEP, and generic PrEP is now available and being used in Scotland and Wales.
It’s a different story in England: after a legal challenge by the National AIDS Trust in 2016, NHS England was found to be responsible for the provision of PrEP[8]
. Its response was a national three-year trial designed to assess the demand for PrEP among populations at risk of HIV, including gay and bisexual men, black African communities and trans people.
Following a series of delays, the trial began enrolling people in October 2017. Demand for the trial has far outstripped its initial 10,000 places and NHS England has since more than doubled its places to 26,000[9]
.
In June 2019, then health minister Seema Kennedy revealed that 38 of the 147 sites involved in the trial were not open for recruitment for men who have sex with men, and 36 remain closed to new recruits[10]
,[11]
.
We have been unequivocal in our demand that no one should be turned away from accessing the trial; a capped trial, designed to test demand, can never fully capture the true level of demand.
Despite the increase in places, some gay and bisexual men who were on waiting lists have since been diagnosed with HIV; 15 people on waiting lists, who were confirmed to be HIV-negative at their first assessment for the trial, are now confirmed to be HIV-positive, although the actual figure may be much higher[12]
. Perhaps, if these people had access to highly effective preventative treatment, these diagnoses could have been prevented.
Budget cuts and broken promises
In England, people can access the PrEP trial only through sexual health clinics, but, since 2014, these services have had their budgets slashed by a quarter, following government funding cuts of £700 million to local council public health budgets[13]
. This austerity has left people not only struggling to access PrEP trial assessments, but also to get appointments for routine sexual health screenings, owing to service closures and staffing cuts[14]
.
Some clinics in south London have even had to turn away people who have presented with symptoms of sexually transmitted infections[15]
. We urgently need a proper funding solution for sexual health services.
PrEP must be embedded as a routine part of these services — a trial is only ever a temporary solution. But since Hancock’s announcement in October 2019, there has been no real progress. The Terrence Higgins Trust’s letter to Hancock, co-authored with 30 other charities and organisations in December 2019, which underlined the urgency of the PrEP situation, seems to have fallen on deaf ears[11]
.
April 2020 is approaching, but there has been no information from the government about how PrEP will be funded and what a national PrEP programme will look like. These concerns have been shared by the Local Government Association, which, in February 2020, urged the government to release details about future funding arrangements for PrEP[16]
.
Human cost of delay
Further stalling is causing uncertainty for the people who are currently on the trial and continued frustration for people trying to access PrEP. Hancock has talked of wanting to champion public health and disease prevention; PrEP is a shining example of a prevention strategy that works, and yet it is still not properly available.
Serious work must be done to ensure PrEP works for all communities that could benefit from it. And this means challenging the common misconception that PrEP is only for gay and bisexual men. This will require targeted work to ensure that anyone at risk of HIV — regardless of their demographic — gets the support they need to access the treatment.
Pharmacists are on the front line
One way to achieve this goal is to ensure that the future PrEP programme is designed in collaboration with the community groups and organisations who support people who are at risk of HIV.
The rollout of PrEP in England will begin in sexual health services. But, after that, it’s important to consider where else PrEP is made available and how. It is only by providing other routes to PrEP that we will guarantee equitable access to all of the diverse communities who could benefit from the treatment.
For example, pharmacists have an important front-line role in providing information and advice on sexual health. Ensuring that pharmacists understand PrEP will be essential in any national programme.
Ending new HIV transmissions
As part of the wider response to HIV, the UK government must now re-commit to its pledge to end new HIV transmissions in England by 2030[17]
. We have the tools to end HIV transmissions, through regular HIV testing, condom use, prevention information and effective HIV treatment, but PrEP plays a vital role in making this a reality.
Following the independent HIV Commission’s recommendations, due to be published in spring 2020, the government must produce a robust HIV action plan that sets out how it will end new HIV transmissions across the UK.
As we start the fourth decade of the HIV epidemic, we must redouble our efforts to end the epidemic once and for all. PrEP will help us to get there — we cannot wait any longer.
Debbie Laycock, head of policy, Terrence Higgins Trust
References
[1] McCormack S, Dunn DT, Desai M et al. Lancet 2015;387(10013):53–60. doi: 10.1016/S0140-6736(15)00056-2
[2] World Health Organization. 2019. Available at https://www.who.int/hiv/topics/prep/en/ (accessed March 2020)
[3] National AIDS Trust. 2018. Available at: https://www.nat.org.uk/we-inform/HIV-statistics/UK-statistics (accessed March 2020)
[4] UK Parliament. 2019. Available at: https://hansard.parliament.uk/commons/2019-10-29/debates/E7EBF5F8-EEA7-497F-AD49-7245419B75FE/Prep (accessed March 2020)
[5] Robinson J. Pharm J 2020;304(7934). doi: 10.1211/PJ.2020.20207741
[6] UNAIDS. 2014. Available at: https://www.unaids.org/en/resources/documents/2014/JC2686_WAD2014report (accessed March 2020)
[7] Public Health England. 2019. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/835084/hpr3119_hiv18-v2.pdf (accessed March 2020)
[8] National AIDS Trust. 2016. Available at: https://www.nat.org.uk/press-release/final-prep-hiv-drug-case-win-national-aids-trust-court-appeal (accessed March 2020)
[9] NHS England. 2020. Available at: https://www.england.nhs.uk/commissioning/spec-services/npc-crg/blood-and-infection-group-f/f03/prep-trial-updates/ (accessed March 2020)
[10] Wilkinson E.Pharm J 2019;302(7926). doi: 10.1211/PJ.2019.20206728
[11] Terrence Higgins Trust. 2019. Available at: https://www.tht.org.uk/news/urgent-action-needed-routine-commissioning-prep (accessed March 2020)
[12] Hunte B. BBC News. 2019. Available at: https://www.bbc.co.uk/news/health-49925389 (accessed March 2020)
[13] Local Government Association. 2019. Available at: https://www.local.gov.uk/parliament/briefings-and-responses/health-and-local-public-health-cuts-house-commons-14-may-2019 (accessed March 2020)
[14] Iacobucci G & Torjesen I. BMJ 2017;356:j1328. doi: 10.1136/bmj.j1328
[15] HIV i-Base. 2018. Available at: http://i-base.info/htb/33968 (accessed March 2020)
[16] Local Government Association. 2020. Available at: https://www.local.gov.uk/prep-fully-fund-councils-avoid-stalled-roll-out-anti-hiv-drug (accessed March 2020)
[17] Department of Health and Social Care. 2019. Available at: https://www.gov.uk/government/news/health-secretary-announces-goal-to-end-hiv-transmissions-by-2030 (accessed March 2020)


