istockphoto.com
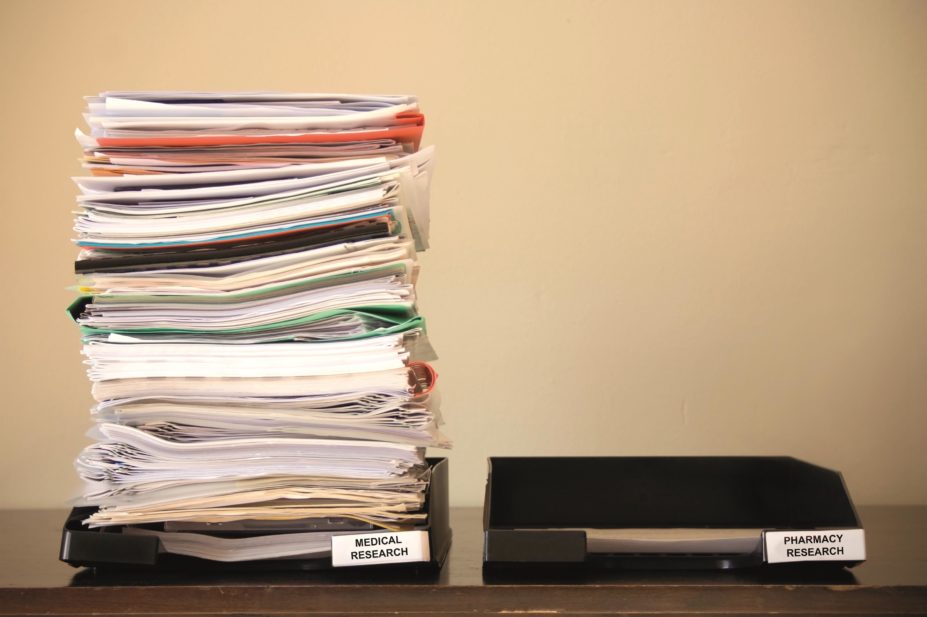
In the past several decades there has been an accelerating momentum in the publication of research investigating the benefits of expanded healthcare roles for community pharmacy. The rise in chronic diseases — with a parallel rise in medication use and medication-related problems — the ageing of the population, and gaps in healthcare provision, especially in primary care, have established a rationale for more effective deployment of healthcare professionals such as community pharmacists to help address the unmet needs of patients. The critical importance of establishing robust evidence supporting the clinical and cost-effectiveness of new clinical roles for pharmacists cannot be understated. Such evidence is needed to convince various stakeholders, including policymakers, other healthcare professionals and the public, that these non-dispensing clinical roles are feasible and add value to patient care.
Successfully conducting research in the community pharmacy practice setting crucially depends on the willingness, cooperation and active participation of not only pharmacy owners but their employee pharmacists, as well as other staff in the community pharmacy.
Getting involved in research
A recent systematic review of the literature[1]
identified a growing trend in recent decades among pharmacists across different countries and care settings towards increasingly positive attitudes and a widely shared belief in the importance of practice research for the development of the profession. The data were synthesised from 15 studies published since 1990, of which 10 were directed at community pharmacists. Most studies were survey based and depended on self-reported data, with the associated potential for respondents to answer questions in a way that they thought may be expected of them. While some studies surveyed a random sample of a population[2],[3]
others used a sample of community pharmacists who had already participated in research[4],[5]
, a group who, on the whole, might be expected to hold more positive attitudes than the general population of pharmacists. Even studies that used a random sampling approach were hampered by low response rates which, again, left open the possibility that those pharmacists who did respond may have held generally more favourable views than non-respondents.
Involvement of pharmacists
It is impossible to estimate accurately the extent of pharmacists’ involvement in research. The most recent survey of a random sample of 1,000 registered pharmacists in Australia, published in 2009, identified that approximately 20% of respondents were or had been involved in research activities[3]
. An earlier UK survey of community pharmacies in east London and Essex reported that 43% (168/390) of respondents had participated in some form of pharmacy practice research[2]
. However, both these studies had low response rates of 37%[3]
and 60%[2]
, respectively.
Even among those pharmacists who volunteer or agree to take part in the research, how well do they perform? It is well known among experienced practice researchers that in every trial of a new clinical service or intervention, there is a proportion of pharmacies that initially agreed to take part and fail to complete the trial. They may drop out at any stage during the course of the trial or, even if they persist, may fail to recruit any participants.
Various strategies are used in the recruitment of pharmacies and pharmacists for research, including personal invitation letters from academics, professional organisations, advertisement through professional journals, e-newsletters, and convenience and snowball sampling of known contacts in an area. Once again, it is not really known which is the most effective strategy and the use of a particular strategy will depend on the size of the study and the available funding to conduct the research. In some jurisdictions, pharmacists can gain continuing professional development (CPD) credits by participating in the research and this, anecdotally, serves as an effective incentive.
Barriers to participation
There are many reasons for lack of engagement, persistence and success. Barriers common to many studies include a lack of research knowledge and skills, financial support, and logistical issues related to staffing and time to dedicate to recruiting patients and implementing the clinical service[1]
.
Small pharmacies with a single pharmacist on duty and limited number of shop staff have rarely been successful in recruiting the target sample of patients or implementing trial clinical services
In my own experience as a practice researcher, infrastructure issues are a common barrier. Small pharmacies with a single pharmacist on duty and a limited number of shop staff have rarely been successful in recruiting the target sample of patients or implementing trial clinical services. Even where there are more pharmacists on duty at any one time, if only one pharmacist has been trained to implement the service and he or she leaves or is ill, the programme cannot be completed. Community pharmacy practice studies work best when there is a strong commitment from the management or owner and involvement of all pharmacy staff such that different staff members can be responsible for different aspects of the research protocol (for example, patient recruitment, making telephone calls, confirming appointments and clinical services delivery). Similarly, provision of support and mentoring to trial sites by the research team, especially in the early stages of the research, also increases the likelihood of successful implementation.
Although remuneration has frequently been identified as a barrier to participation in research and the adoption of new clinical services in pharmacies, in practice, even if remuneration is available, the service will not be successfully implemented in the absence of suitable infrastructure to support its delivery.
Another challenge to researching new clinical services in community pharmacy has been a lack of support from those in the medical profession, who see extensions of the pharmacist’s clinical role as a threat or encroachment on their patient care roles[6]
. From my own research experience, where pre-existing effective professional working relationships between pharmacists and GPs have been in place, implementation of pharmacy practice trials of new clinical services has been far easier to implement and more likely to succeed.
Feeling motivated
There are ways to motivate pharmacists to participate in research. A strong belief in the importance and value of pharmacy practice research is a critical motivational force[1]
. Exposure to and experience in conducting pharmacy practice research in the course of pharmacy education encourages the development of positive attitudes to research and a willingness to undertake or participate in research in the future[7]
. Similarly, once a pharmacist has been involved in a research project and has come to appreciate the benefits of the research, in terms of personal professional development, value for pharmacy as a profession and the health impacts for their patients, they are much more likely to seek further opportunities to participate in other studies
[6],
[8],[9]
.
In recent years, the formation of pharmacy practice research networks (PBRNs) of community pharmacies in the United States[10]
and Canada[11]
has been reported in the literature. The objectives of the PBRNs are to enhance pharmacy practice research capacity by building communities of practitioners skilled in research and readily able to participate in well designed trials of new clinical services. Based on surveys of community pharmacies, it appears that the PBRN concept offers an attractive strategy to foster the development of a pharmacy practice research culture.
In the UK, the Research Ready initiative, developed by Pharmacy Research UK in conjunction with the Royal College of General Practitioners and the National Institute for Health Research Clinical Research Network, is an online self-accreditation tool covering the basic requirements for undertaking primary care research in the UK.
Another successful strategy has been the application of action research approaches to engage practitioners to work with researchers as collaborators from the start through to implementation and evaluation[12]
. This approach was applied in a Danish project that aimed to investigate the unmet needs in pharmaceutical care services in Danish pharmacies. The study involved researchers as initiators and resources for the study, internship pharmacies as hosts and study mediators for pharmacy staff and interns, and the internship students themselves as local leaders in their respective internship, responsible for data collection on the pharmaceutical care service needs of different patient groups[12]
.
Long way to go
Although there is a growing appreciation of the critical role of research in establishing new clinical pharmacy services, this has not translated into widespread engagement and normalisation of practice research into the professional culture of pharmacy. A range of strategies are needed to influence attitudes, enrich knowledge and skills, build communities of research practice and thereby empower practitioners to commit to and become collaborators in research to advance the societal value of community pharmacy.
Ines Krass is professor of pharmacy practice at the University of Sydney, Australia.
References
[1] Awaisu A & Alsalimy N. Pharmacists’ involvement in and attitudes toward pharmacy practice research: a systematic review of the literature. Res Social Adm Pharm 2014. doi:10.1016/j.sapharm.2014.12.008
[2] Rosenbloom K, Taylor K & Harding G. Community pharmacists’ attitudes towards research. International Journal of Pharmacy Practice 2000;8:103–110. doi:10.1111/j.2042-7174.2000.tb00994.x
[3] Peterson GM, Jackson SL, Fitzmaurice KD et al. Attitudes of Australian pharmacists towards practice-based research. J Clin Pharm Ther 2009;34:397–405. doi:10.1111/j.1365-2710.2008.01020.x
[4] Simpson SH, Johnson JA, Biggs C et al. Practice-based research: lessons from community pharmacist participants. Pharmacotherapy 2001;21:731–739. doi:10.1592/phco.21.7.731.34570
[5] Saini B, Brillant M, Filipovska J et al. Factors influencing Australian community pharmacists’ willingness to participate in research projects — an exploratory study. International Journal of Pharmacy Practice 2006;14:179–188. doi:10.1211/ijpp.14.3.0004
[6] Emmerton LM, Smith L, LeMay KS et al. Experiences of community pharmacists involved in the delivery of a specialist asthma service in Australia. BMC Health Serv Res 2012;12:164. doi: 10.1186/1472-6963-12-164
[7] Kritikos VS, Carter S, Moles RJ et al. Undergraduate pharmacy students’ perceptions of research in general and attitudes towards pharmacy practice research. Int J Pharm Pract 2013;21:192–201. doi:10.1111/j.2042-7174.2012.00241.x
[8] Armour C, Brillant M & Krass I. Pharmacists’ views on involvement in pharmacy practice research: Strategies for facilitating participation. Pharm Pract 2007;5:59–66. PMID: 25214919
[9] Lowres N, Krass I, Neubeck L et al. Atrial fibrillation screening in pharmacies using an iPhone ECG: a qualitative review of implementation. Int J Clin Pharm 2015. PMID: 26202627
[10] Snyder ME, Frail CK, Seel LV et al. Experience developing a community pharmacy practice-based research network. Innovations in pharmacy, 2012.
[11] Hebert J, Laliberte MC, Berbiche D et al. The willingness of community pharmacists to participate in a practice-based research network. Can Pharm J (Ott) 2013;146:47–54. doi:10.1177/1715163512473240
[12] Sorensen EW & Haugbolle LS. Using an action research process in pharmacy practice research — a cooperative project between university and internship pharmacies. Res Social Adm Pharm 2008;4:384–401. doi:10.1016/j.sapharm.2007.10.005

