Callie Jones
To err is human. But if you are a pharmacist it can land you in jail. Six years of campaigning to lift the threat of conviction for pharmacists who make a dispensing error have borne fruit, albeit unripe, with the launch of a consultation on 12 February 2015 from the UK health departments to have the law amended.
Making a dispensing error has been a criminal offence since the Medicines Act 1968 came into force. In the late 1960s, medicines supply was largely a commercial transaction and the law was introduced to prevent adulteration of pharmaceutical preparations meant for human use.
But in April 2009, the issue went from being largely academic to a matter for the real world when a locum community pharmacist was given a suspended prison sentence for making a dispensing error.
Pharmacists consider it unjust that a single, inadvertent dispensing error is considered a crime — a viewpoint reflected regularly in these pages. After all, no other healthcare professional in the UK has the same spectre hanging over their work.
The proposed changes recognise that the threat of prosecution can neither encourage reporting of dispensing incidents (which is essential) nor prevent someone from making a mistake.
Pharmacists must be aware, however, that the proposed changes do not “decriminalise” dispensing errors. Rather, the two draft statutory instruments introduce a defence that a registered pharmacist or pharmacy technician can employ if charged. For the defence to apply, the medicine must have been dispensed in registered premises by a registered pharmacist or pharmacy technician, acting in the course of his or her profession. The patient affected by the error must also have been notified promptly.
The burden, however, will be on the pharmacist or pharmacy technician to show that a defence applies before the case goes to court.
Pharmacists may be relieved to note that failure to comply with a procedure within the pharmacy “does not of itself constitute proof that the registrant was not acting in the course of his or her profession”.
Slow progress
At the time of the first prosecution, the UK pharmacy regulator the Royal Pharmaceutical Society of Great Britain said that it should be the body to deal with any dispensing errors and not the Crown Prosecution Service.
Since becoming a voluntary professional leadership body in 2010, while the General Pharmaceutical Council became the regulator (GPhC), the Royal Pharmaceutical Society (RPS) has lobbied to have the law changed. It has latterly joined, along with the GPhC, the Pharmaceutical Society of Northern Ireland and other stakeholders, the Rebalancing Medicines Legislation and Pharmacy Regulation Programme Board, set up to review the relevant legislation and regulation and to advise UK Ministers on policy.
There was an early setback when a proposed “due diligence” defence was withdrawn from the Health and Social Care Bill in 2011 after the measure lost support from pharmacy bodies.
Then, much of the UK medicines legislation from the Medicine Act 1968 was consolidated into the Human Medicines Regulations 2012, but those elements regarding medicines supply and pharmacy premises regulation remained untouched. This was a missed opportunity for reform.
The rebalancing programme board, chaired by Ken Jarrold, met for the first time in May 2013. Although the process appears drawn out — and the minister with responsibility for pharmacy Earl Howe has apologised for the delay — this consultation is a positive step and the rebalancing programme board has done well to navigate a complex area of legislation. Close inspection of the consultation and accompanying draft Orders, under section 60 of the Health Act 1999, reveals that some creativity was needed to find an acceptable solution. The rebalancing programme board has had to consider the medicine supply components of medicines legislation, the regulation of pharmacists and pharmacy technicians, as well as pharmacy premises regulation.
Among the complexities is the fact that pharmacy regulation is fully devolved in Northern Ireland, where pharmacy technicians are not a registered profession, and so the draft Pharmacy (Preparation and Dispensing Errors) Order 2015 requires the agreement of the Minister for Health, Social Services and Public Safety for it to start in Northern Ireland. In Scotland, the regulation of pharmacy technicians is a devolved matter specifically, and so the legislative proposals will also require debate and approval by the Scottish Parliament.
Room for improvement
The manoeuvring has also left some gaps.
Many hospital pharmacies are not registered premises and so the draft Orders do not cover for those, and this is proposed as part of a second phase of work. This is a practical concession to enable the rebalancing work to move forward at this time, but the defence must be extended to include hospital pharmacy at the earliest opportunity.
The programme board has also been asked to examine and provide greater clarity on the roles, accountability and competence of pharmacy owners, responsible pharmacists and superintendent pharmacists. This is to be considered in a later consultation. This work is important, and clarity is certainly needed in this area, but it must not delay implementation of the proposals currently under consultation.
Moreover, the timing of the consultation may be problematic, given that it closes on 14 May 2015. The UK governments must work together to expedite this law change and not let it stall in the aftermath of the May 2015 general election.
The rebalancing consultation states that “the greatest fear among pharmacy professionals is fear of prosecution”. The Pharmaceutical Journal is quite sure that the vast majority of pharmacists would say that causing harm or the death of a patient is their biggest concern. Nonetheless, it is not self-serving for the current situation to be rectified. A just culture is one that focuses on learning from incidents rather than blaming human error. This approach must be at the forefront of modern healthcare.
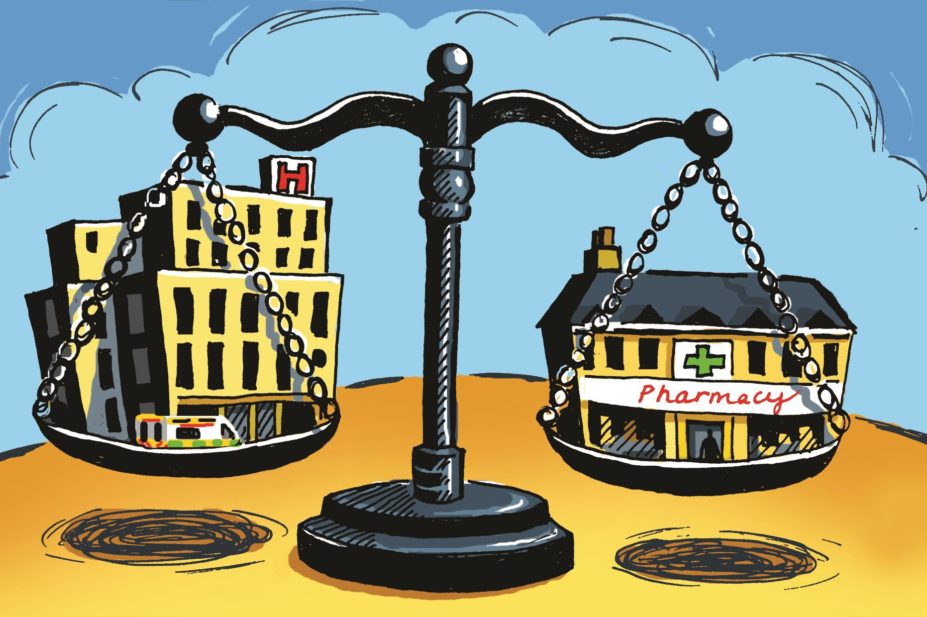
The consultation document acknowledges quite rightly that “fear is toxic to safety and improvement”, and it is in this spirit that the proposals seek to rebalance the scales.


