Jonathan Buisson
The biggest IT medicines safety drive in the world begins in less than six months, but the UK is far from ready.
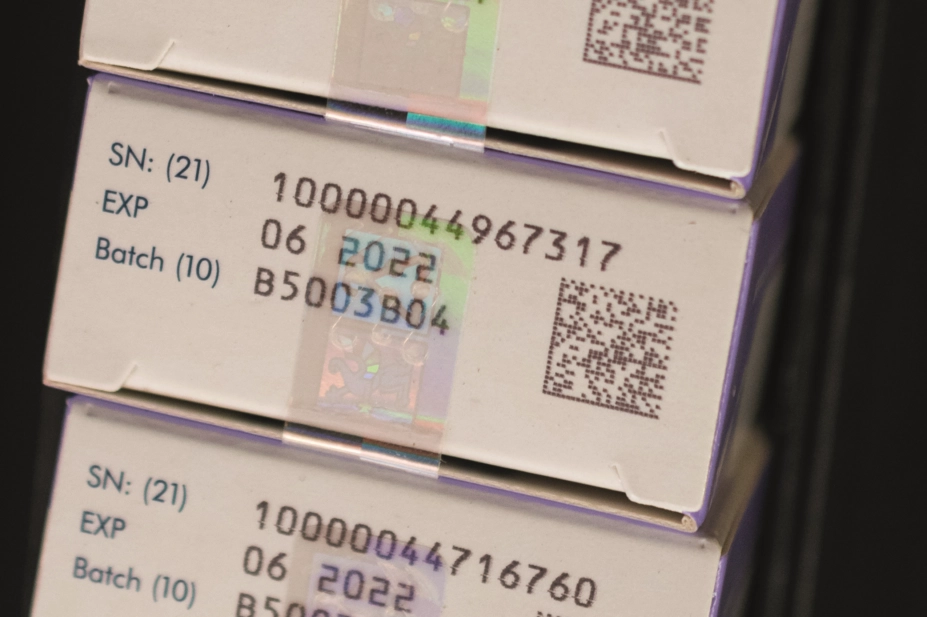
The Falsified Medicines Directive is designed to stop fake medicines from entering the supply chain, with a mega-database set up in Brussels that will track where drugs go around Europe. All pharmacists will be legally required to verify any medicines they receive and decommission any leaving the supply chain, for example when dispensing to patients, from 9 February 2019. It is a huge logistical challenge.
Pharmacists can prepare now by revising workflows and contacting their IT supplier, but crucial information is still missing. We don’t know what sanctions pharmacists will face for not adhering to the regulations (that was only put out for consultation in July 2018), what the anti-tamper devices will look like and whether the EU hub will have all the data it requires on launch — worryingly, only 5% of pharmaceutical companies are fully connected to the hub, and a third have not even started the process.
More importantly, the whole question of who is going to pay for the new hardware required is shrouded in doubt. The Medicines and Healthcare products Regulatory Agency (MHRA) published an assessment of the impact of FMD for wholesalers, care homes, opticians and prisons in July 2018. But this assessment did not cover the potential costs to community or hospital pharmacies.
A spokesperson from the agency told The Pharmaceutical Journal that “the MHRA has not published a UK-specific full impact assessment, and does not intend to publish one at this point in time”. But is this really good enough?
The only assessment of how much this is all going to take out of each pharmacy’s bottom line is a 2015 document from the European Commission, which said a community pharmacy would be expected to face costs of around €530 per year to modify software for FMD compliance, purchase new barcode scanners and perform medicines authentication. A hospital pharmacy, the report said, would face annual costs of up to €750.
Not large amounts of money, but the current advice from experts is for community pharmacies to be cautious about purchasing any new scanners or other technology before they have assurances on whether this expenditure will be reimbursed. National negotiations are ongoing, although the most recent update from the Pharmaceutical Services Negotiating Committee suggests costs will only be “recognised in future NHS funding settlements” — i.e. after the regulations are brought in.
And to compound the situation, these regulations are set to come into force just six weeks before the UK leaves the EU, with all the disruption that could bring. Indeed, some experts are questioning how long the FMD system will be needed post-Brexit as, under Article 7 of the EU withdrawal Bill, the UK could lose access to all EU networks and information systems and databases post-transition. The UK government is aiming for regulatory alignment on medicines policy that should allow for continued access, but is also talking up a ‘no deal’ scenario that could leave all FMD preparations in tatters.
The government appears to be asleep on the job, while confusion reigns. Pharmacists need immediate clarity from the Department of Health and Social Care on how these regulations are going to be brought in and a promise that all costs will be reimbursed. The time for answers on FMD is well overdue.
For more information about how to prepare for FMD, visit fmdsource.co.uk
You may also be interested in

MHRA confirms it will consider UK version of Falsified Medicines Directive

More than 40% of people with ADHD waiting at least two years to access mental health service, study finds
