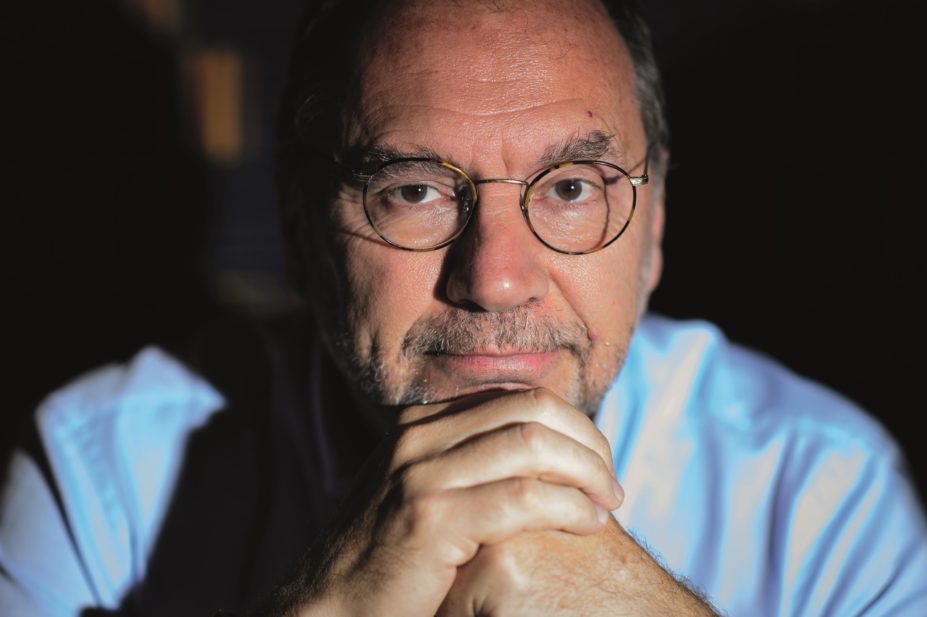
Leon Neal / AFP / Getty Images
How well has the current Ebola outbreak been handled?
We have a huge crisis right now because of inaction in the beginning. It has been shown over and over that Ebola can be contained if you act quickly. Once it gets into big cities and slums, it becomes very difficult to contain. Local governments, national governments and the international community need to take lessons from that. But now the priority is to deliver what the international community has promised. I must say I am proud of the UK response. It has been well coordinated: the Prime Minister’s office, the army, the Department of Health, non-government organisations [NGOs]. You cannot expect a heroic NGO like Médecins Sans Frontières to carry the whole weight of such an epidemic — it is, after all, an NGO and I admire them greatly, but we need governments to come in.
How contagious has it proven to be?
It is highly contagious if you have very close contact, but it is not contagious when you keep your distance as it is not air-borne. The big problem with Ebola as a contagion is the mortality — its lethality. So you do not want to take any risks. A slight mistake can be fatal.
What can be learned from the current crisis?
The first lesson is that anything can happen. We can have a completely destabilising epidemic in countries that until now have only had very limited outbreaks. The second lesson is that, although the outbreak can be thousands of miles away, if even one person is evacuated with the infection, the threat is immediate and also very expensive. So it is in everyone’s interest in an economic sense for the global community to support the control of the epidemic in Africa. Thirdly, we need a new paradigm to evaluate drugs and new vaccines for rare diseases and epidemic diseases. There need to be protocols ready in time for the next epidemic so we can test these drugs and vaccines in the epidemic circumstances. This is not easy, but we have to do it.
Do we know more from fast tracking experimental Ebola vaccines?
The Ebola epidemic, and to some extent pandemic flu, illustrates that it is possible to accelerate the development of new vaccines safely and ethically. We have to test them out to know they will work. But it is not necessary to spend so many years developing a vaccine if there is a way to do it more quickly.
Why do some infectious diseases remain neglected in the developing world?
There is a mixture of things. There is a market failure because it has not been an attractive market for the pharmaceutical industry. But also our scientific knowledge is very limited, so we don’t know exactly what had to be done for these diseases, and they are diseases of poverty in many cases. So a combination of things, but I think this is changing tremendously thanks to a number of partnerships.
What kind of advantages can public-private partnerships have in the development of new medicines?
Public-private partnerships bring together sectors and institutions that normally are not working in partnership: academia, pharmaceutical companies, NGOs, public sector funders. This requires an organisation to bring that together.
How important is it to consider the people who will deliver new treatments and medicines access in drug development?
Ensuring access to medicines has to be incorporated from the beginning, even when you don’t know whether a medicine is going to work or not. Otherwise you risk developing something that you will never see reach the people who actually need it. That is very important.
Once [your product] is more advanced, you need to involve communities and community leaders, because without acceptability and trust those people will not want it. It’s amazing that this has not been done more in the past.
Interview by Matthew Wright
Matthew Wright interviewed Peter Piot at an event held in the Japan Embassy in London in November 2014 to promote the Global Health Innovative Technology Fund — a public-private partnership involving five Japanese pharmaceutical companies, the Japanese government, the Bill & Melinda Gates Foundation and the United Nations Development Programme.

