MD Anderson Cancer Center
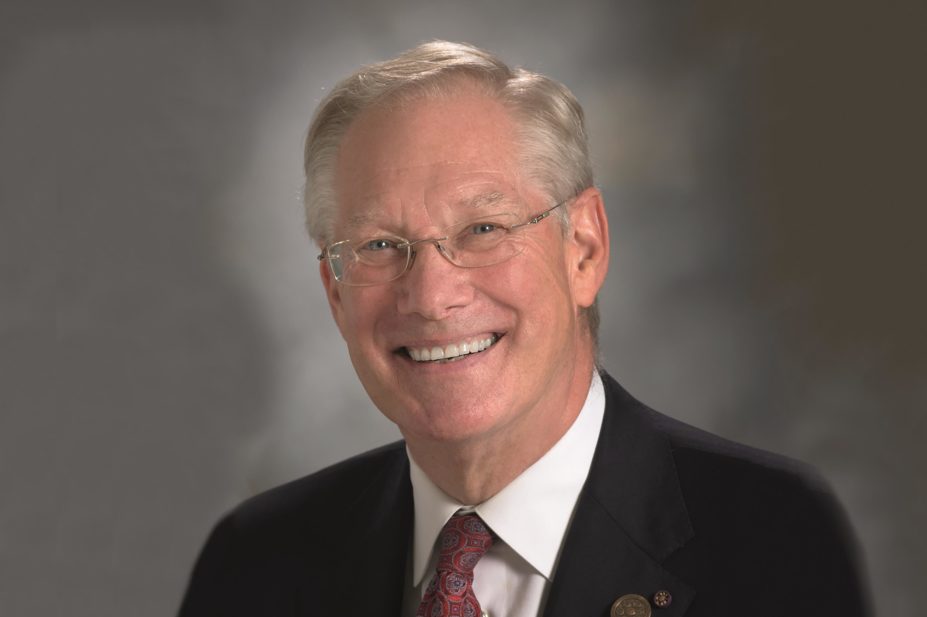
V Craig Jordan, Dallas/Fort Worth living legend chair of cancer research, professor of both breast medical oncology and molecular and cellular oncology at the University of Texas MD Anderson Cancer Center in Houston, is best known as “the father of tamoxifen”.
Labelled “very unusual” at school in Cheshire because of his pioneering approach to chemistry, Jordan took a special studies pharmacy course at University of Leeds before specialising in endocrine breast cancer research. Handed a failed contraceptive called tamoxifen to investigate after completing his PhD, he proceeded to carry out seminal laboratory studies that would provide the necessary evidence to underpin its long-term use to treat and subsequently prevent breast cancer.
Jordan has spent many years at leading research institutes in the United States, taking a translational approach to research, with the aim of identifying simple solutions in the laboratory that will have a worldwide impact on human health. His current research is focusing on oestrogen-induced apoptosis as a method of reducing breast cancer recurrence following adjuvant treatment with tamoxifen or aromatase inhibitors. He predicts that a similar approach to androgen-induced apoptosis will have a major impact on the future of treatment for prostate cancer.
Jordan has received many prestigious awards for his research and, in 2002, he was appointed an OBE for services to international breast cancer research. He is honorary member of the Royal Pharmaceutical Society, the first non-professional pharmacist to be elected.
I poisoned myself with chlorine gas, set fire to the curtains and killed the grass outside my window — it grew back blue
Here, Jordan talks about his early adventures as a schoolboy chemist, the fortuitous events that enabled him to choose how to investigate tamoxifen and the subsequent research that helped to differentiate the effects of a variety of selective oestrogen receptor modulators (SERMs) in breast cancer, osteoporosis, heart disease and uterine cancer. He also offers valuable advice to pharmacists who would like to get involved in drug research.
How did your interest in science and drug research start?
At grammar school, my main passion was for chemistry and, in a moment of insanity, my mother allowed me to set up a lab in my bedroom. I poisoned myself with chlorine gas, set fire to the curtains and killed the grass outside my window. It grew back blue!
I always wanted to be a chemistry technician at ICI Pharmaceuticals, which later became AstraZeneca, near where I lived in Cheshire. But the careers master said that I should go to university because I was an unusual boy and, by that time, I’d set up a lab at school and was teaching chemistry to other pupils in the lunch hour.
I went to University of Leeds on the special studies pharmacy course in the pharmacology department, took to it like a duck to water, and came top. However, I was the least likely person to do it, given that I only got three ‘O’ levels, including chemistry, of course, but my mother had persuaded the school to let me stay for the sixth form on the promise I would get a few more.
You’ve been labelled “the father of tamoxifen” — the first targeted therapy for breast cancer. How did this discovery come about?
It was accidental. After the pharmacy course, I wanted to develop drugs for cancer but there was no opportunity and I ended up doing a PhD at Leeds on the structure function relationships of non-steroidal antioestrogens that were failed contraceptives. The university recruited Arthur Walpole, head of reproduction research at ICI, as external examiner for my PhD, and he then facilitated my move to the Worcester Foundation for Experimental Biology, in Massachusetts, for two years, prior to me taking up a lectureship in pharmacology back at Leeds. My supervisor in the US promptly left for another job, saying I could do whatever I wanted and, fortunately, Walpole secured funding from ICI to investigate the anticancer properties of ICI 46,474 — a failed contraceptive eventually called tamoxifen.
The animal studies I carried out at the Worcester labs during the early 1970s and later back at Leeds confirmed the antitumour effects of tamoxifen and provided the first consistent evidence that tamoxifen blocks the binding of oestradiol to the human breast and endometrial cancer 8S oestrogen receptor. Soon, tamoxifen was used in breast cancer treatment but only for a year after surgery, and the real Eureka moment came in 1977, when my animal experiments showed that indefinite treatment of oestrogen receptor positive tumours stopped them from growing.
We carried out research that ultimately supported use of tamoxifen for breast cancer prevention, although at the time it was considered science fiction
People in the clinical community were skeptical because they had based their one-year treatment recommendation on data from women with metastatic disease. But I thought microscopic disease was different, so tamoxifen was needed for much longer to suppress the cancer. Of course, women now take it for up to ten years.
In the mid-1970s, we also carried out research that ultimately supported use of tamoxifen for breast cancer prevention, although at the time it was considered science fiction.
What did discoveries around tamoxifen lead to in terms of development of other SERMS?
Once we started giving tamoxifen to well women to prevent breast cancer, we needed to learn more about its effects on bones. Because it was an antioestrogen, we didn’t want to prevent breast cancer but cause osteoporosis. When we gave tamoxifen and a failed prospective antioestrogenic cancer drug, keoxifene, to animals which had had their ovaries removed, they were both more effective at maintaining bone density than oestrogen. In some other experiments we gave tamoxifen to immunosuppressed animals with both oestrogen-receptor-positive (ER+) breast and ER+ endometrial tumours, and found that the breast tumours were controlled but there was dramatic growth in the endometrial tumours.
We started to realise that tamoxifen and keoxifene, which became raloxifene, varied in the way they selectively switched oestrogen receptors on or off in different parts of the body, owing to differences in the biochemistry of the target site. They were both SERMS that acted on the same receptor, but different connector molecules in different tissues made them act either as an agonist or an antagonist.
By the end of the 1980s, we knew we could do better than tamoxifen by looking for SERMS that could prevent osteoporosis and coronary heart disease (by lowering cholesterol) and also reduce the risk of breast cancer while not increasing the risk of uterine cancer. Raloxifene proved to be the first of these drugs, and we now have five different SERMs on the market here in the United States.
How has the treatment of ER+ breast cancer changed over the past few decades since your breakthrough discoveries?
For all the good, bad and ugly of tamoxifen, it’s probably prescribed more than aromatase inhibitors because of its cost-effectiveness
Endocrine therapy has moved ahead with the introduction of the aromatase inhibitors. They cause fewer blood clots and less risk of endometrial cancer than tamoxifen, although they do reduce bone density. They’re only available for post-menopausal women but they do have a proven benefit in the long-term control of breast cancer. Now that they’re coming off patent, their prices will fall so they will become available in countries which can’t afford expensive drugs.
Even so, tamoxifen is still widely used. For all the good, bad and ugly of tamoxifen, it’s probably prescribed more than aromatase inhibitors because of its cost-effectiveness.
What are the greatest challenges remaining for breast cancer treatment?
Tamoxifen was the first targeted, personalised treatment for any cancer. Now, everyone’s screening the genome for mutations that can be targeted by precision medicines. In a way, the pharmaceutical industry is challenged by having too many targets because, if you can’t find treatments to act on those targets, you won’t save lives.
The pharmaceutical industry is challenged by having too many targets because, if you can’t find treatments to act on those targets, you won’t save lives
Another challenge is to get people to keep taking the tablets. Many women don’t continue tamoxifen treatment for five years and, if you start adding other treatments to make endocrine therapy work better there may be more side effects, making it even harder to get patients to keep taking them.
There is also the need to find treatments that countries can afford within limited budgets. The new generation of genetically targeted treatments are expensive, and we need also to develop treatments that are cost-effective enough to be used in poorer countries where breast cancer is becoming more common as people live longer.
Your published papers are among the most cited in breast cancer research and you have won numerous awards. What is your next major goal?
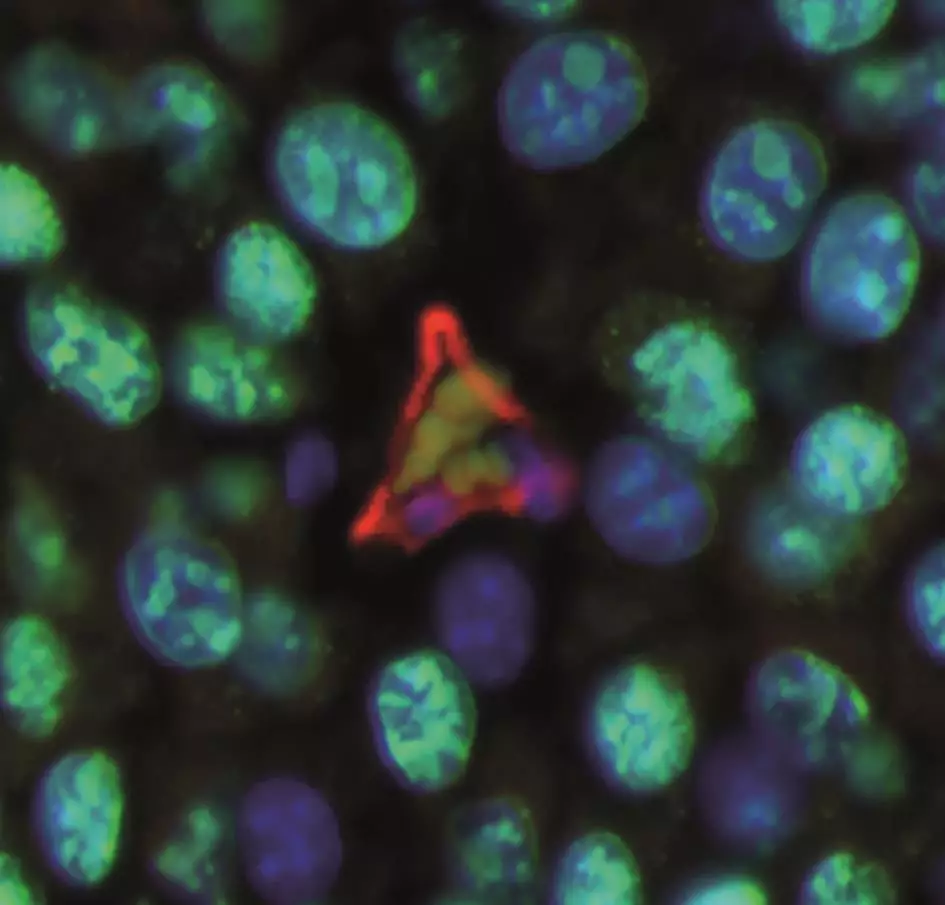
I am focusing on what happens to breast cancer cells when you stop tamoxifen or aromatase inhibitors after five or more years of treatment. These drugs control breast cancer, but they don’t kill cancer cells so, when you stop treatment or a woman becomes resistant to them, any remaining micrometastases may trigger a recurrence. The answer appears to lie with oestrogen-induced apoptosis.
When oestrogen increases after antioestrogen therapy is withdrawn, it no longer stimulates growth of breast cancer cells — as it would before antioestrogen therapy — it stimulates apoptosis and kills breast cancer cells. In 30% of women, we can measure DNA markers from dying cancer cells after antioestrogen therapy is stopped. I now want to test drugs already on the market to see if they can trigger oestrogen-induced apoptosis, so we can increase the proportion of women with evidence of dying tumour cells to 80% and, in this way, prevent disease recurrence.
The same approach could be used in men with prostate cancer who become resistant to anti-androgen therapy, by enhancing their natural occurring androgen-induced apoptosis. Nature is telling us something about this family of diseases and we just need to learn how to make best use of this approach.
Could you give three pieces of advice to young pharmacists wanting to go into drug research?
Take responsibility for training yourself in the skills you need to become the best you can be. You need to find the models you want to work with, practise your techniques and become the expert so you can teach others.
Use the literature to find out the movers and shakers in the field and learn how to meet and talk to them at scientific conferences
Use the literature to find out the movers and shakers in the field and learn how to meet and talk to them at scientific conferences. Read papers in your field in detail so you can stand out at scientific meetings with your knowledge and interest and your ability to answer any question that comes at you.
Set your goals and ensure you’re talent spotted. Learn how to give talks and present your information in a public forum, to be engaging and make the arguments and draw conclusions that make sense. If you can’t get up and give a talk, on time and with excellent slides, you won’t succeed. This is the reality I’ve lived.