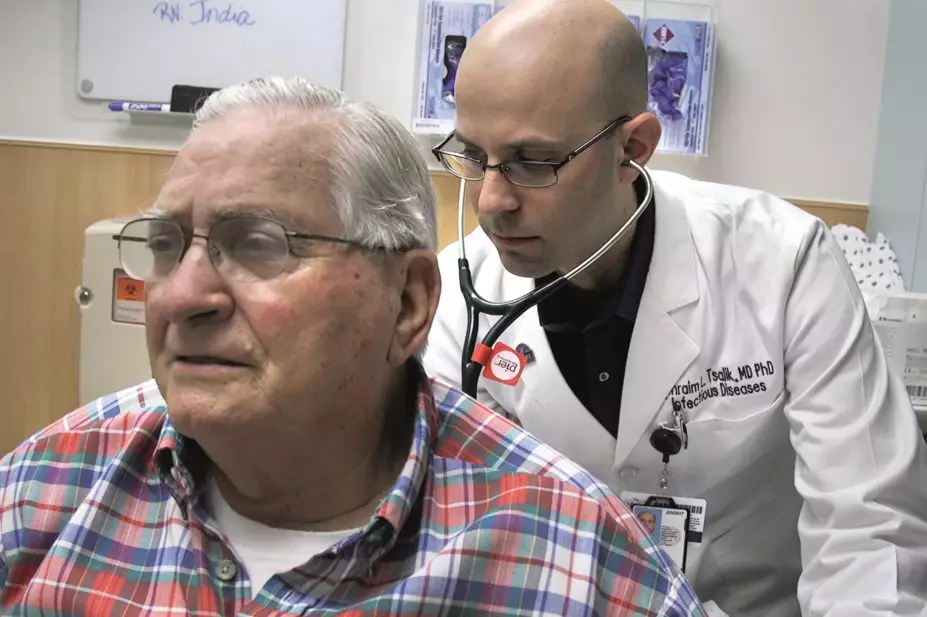
Duke Health
A new way to distinguish between bacterial and viral respiratory infections has been developed by researchers in the hope it could limit the inappropriate use of antibiotics, an important driver in the emergence of antibiotic resistance.
Researchers from Duke University in Durham, North Carolina, compared gene expression patterns in blood samples from 273 patients who were admitted to hospital with respiratory illness: 115 of whom had a viral infection; 70 had a bacterial infection; and 88 had a non-infectious illness, such as sarcoidosis or lung cancer. A total of 44 healthy adults were used as a control cohort.
The 273 patients were split into different groups, identifying a set of markers able to differentiate between the causes of respiratory illness, with an overall 87% accuracy. In comparison, a procalcitonin test, widely used to help identify bacterial infections, was only 78% accurate (P<0.03).
Commenting on the study, Kieran Hand, a consultant pharmacist in anti-infectives at University Hospital Southampton NHS Foundation Trust, says that the results build upon the relatively novel concept that host response biomarkers of gene expression can be used to identify bacterial or viral infection.
“What this study adds is to identify markers that discriminate between illness of bacterial or viral aetiology and illness of non-infectious causes in addition to healthy controls,” he says.
The researchers, who published their findings in Science Translational Medicine on 20 January 2016[1]
, say that the inclusion of patients with non-infectious illness was important. Previous studies have often compared patients with bacterial and viral infections to healthy controls only. However, gene expression markers of patients who are suffering from a non-infectious illness may overlap with those who have an infection.
Initially, the researchers compared infected patients to healthy controls to see if this could accurately predict patients without an infection. However, when these markers were applied to the 88 patients with a non-infectious illness, 48 patients were identified as having a bacterial infection, 35 patients had a viral infection, and 5 patients were healthy. After this, the ill but not infected group was used as the control group.
“Should a rapid point-of-care test incorporating these biomarkers eventually become available in clinical practice, there is obvious potential to reduce unnecessary antibiotic prescribing by providing reassurance to patients, parents and doctors that antibiotics would be unlikely to offer benefit,” Hand comments.
But the authors of the study highlight that “the technical hurdle to transfer these targets to a reliable, timely, affordable, and accessible platform remains”.
The prescription of antibiotics for acute respiratory illness, most of which are viral, has been an ongoing problem in the fight against antibiotic resistance. In the United States, 73% of outpatients with acute respiratory illness are prescribed an antibiotic, compared with 54% in the UK.
References
[1] Tsalik E, Henao R, Nichols M et al. Host gene expression classifiers diagnose acute respiratory illness etiology. Science Translational Medicine 2016. doi: 10.1126/scitranslmed.aad6873


