This content was published in 2005. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
1. Introduction
This guide has been updated from previous work on audit carried out by the Royal PharmaceuticalSociety and will help pharmacists implement the audit requirements of the new pharmacy contract introduced in England and Wales on 1 April 2005. Each community pharmacy currently needs to participate in at least two clinical audits each year, one based on its own practice and one multidisciplinary audit determined by the local primary care organisation (PCO).
2. What is audit?
A simple definition of audit is “improving the care of patients by looking at what you are doing, learning from it and, if necessary, changing practice”.This is not anything new. It is something that most health professionals have done fora long time as part of everyday practice. Nowadays, though, clinical audit should be viewed as an integral part of practice, hence the requirements of the new pharmacy contract. Audit provides objective rather than subjective information upon which to base any changes.Clinical audit is part of quality assurance, ensuring that the best possible service to patients is offered and the risk of errors minimised.There are many formal definitions of audit, including:
- The systematic analysis of the quality of health care, including procedures used for diagnosis and treatment, the use of resources and the resulting outcome and quality of life for the patient
- A continuous cycle that involves observing practices, setting standards, comparing practice with standards, implementing improvements and observing new practice to ensure that the improvement is maintained
Clinical audit relates to all aspects of patient care provided by any health care professional. Clinical audit should have clear outcomes that should lead to an improvement in patient care. It should not be looked on as an end in itself but should be seen as a means of assuring and improving the quality of care, ie, maximising positive outcomes.
Some elements of clinical audit are similar to research but audit is not research.Research creates and tests new hypotheses, whereas audit studies standards of care with a view to improving quality of care. Clinical audit is all about improving the quality of one’s work — it should take the guess work out of evaluation.
For pharmacists there are many benefits of being involved in clinical audit, such as:
- It demonstrates a willingness to maintain good professional standards, and as such is part of the new contract for community pharmacy in England and Wales
- It improves the quality of working life by getting evidence-based results
- It enhances efficient use of resources (people, time, money)
- It helps support change by producing objective information about the quality of care
3. What constitutes good quality clinical audit?
“Clinical audit in the NHS”(NHS Executive 1996) laid out definite aims for audit:
- A clear patient focus — involving patients directly in audit processes can be difficult but it is through patient experiences that clinical quality and clinical outcomes become more meaningful
- Greater multiprofessional working across the different clinical and managerial disciplines that contribute to the patient’s episode of care, again recognised in the new pharmacy contract
- An inter-sectoral approach, where a patient’s care is managed across primary, secondary and continuing care, particularly important in chronic illness and disability
- Closer links with education — audit has a role in professional self-development
- Better integration of effectiveness information — the audit process should draw on sound information about potential clinical effectiveness, variations in practice, cost effectiveness, critical appraisal skills and outcome measurement
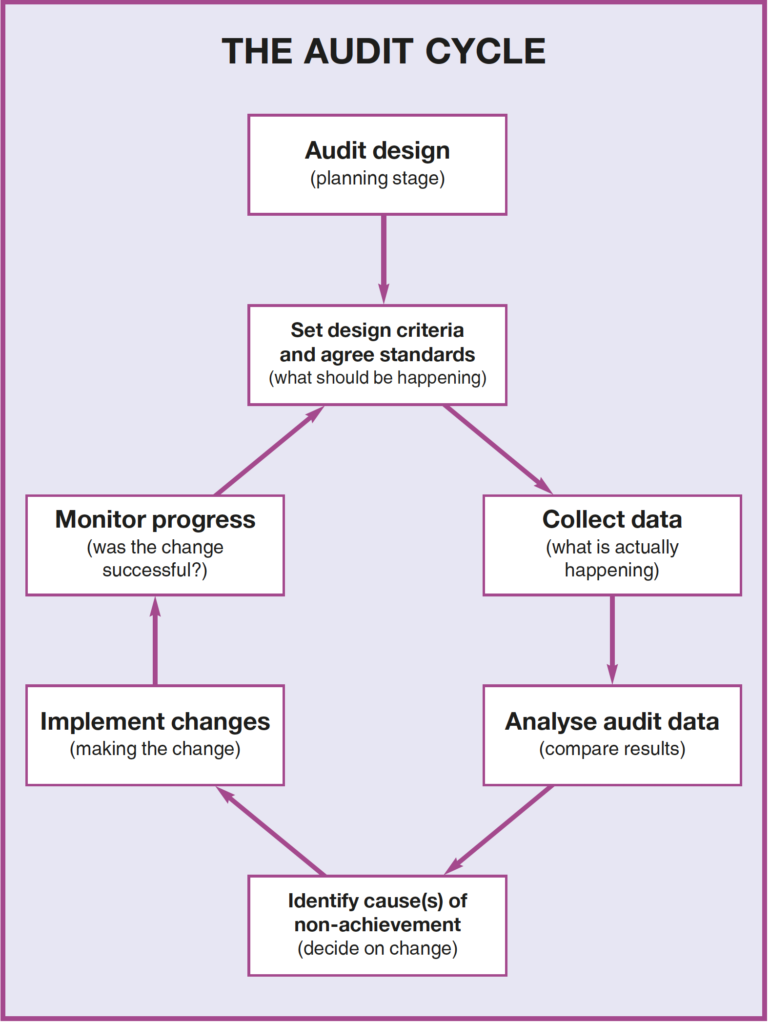
The audit cycle
Although audit is often described as a cycle it should not be seen as a “one-off ” exercise but as an ongoing quest to improve and maintain standards constantly.
Audit design and planning
Audit is easiest when it is well designed and simple.The choice of topic is vital.
It is easier to motivate participation when all involved can identify with the topic and see the benefits. This is especially important with multiprofessional audit.
Topics
Choosing a topic can be the hardest part. The topic has to be important to the pharmacy, patients or practice. Topics to be considered include:
- High risk
- High volume
- Local issues
- Targets
- Areas of concern
- Areas of financial concern using a large amount of resources (time, people, money)
- Areas in the new pharmacy contract such as medicines use review (MUR) and repeat dispensing
Performance is often broken down into three aspects:
- Structure —what you need
2. Process — what you do
3. Outcome — what you expect to happen
An early expert on quality in health care, Donabedian, put this into three questions to ask of health care:
- What facilities are there?
2. What was done to the patient?
3. What was the result for the patient?
Whatever topic is chosen it is important to consider a few practical points:
- Is it realistic?
- Is it a real problem?
- Has it a measurable activity?
- Can standards be set?
- Can a change be made?
- Is the effort required acceptable?
- Is it a controversial subject?
- Would changes be welcomed by everyone?
- Has the group involved (especially if multiprofessional) the necessary expertise and enthusiasm?
It is best to start on a small scale and build on success rather than start with the hardest problem.
Other important points to consider are:
- Select one member of the team to be co-ordinator for that particular audit project with responsibility for the overall management of the project
- Decide how long the audit should run (using the simplest method for the shortest time is a great motivator)
- Include effecting change as an intention of the audit
- Stress confidentiality
- Focus on a specific aspect
- Aim only to collect data that are necessary
- Stress that the audit is not designed to bean inspection or to criticise individuals but to improve patient care
The audit must be owned by participants. Sample audits can be given for guidance but it is useful if they are not written in tablets of stone or if people have had chance to comment on them.
Step 1. Setting criteria and agreeing standards (what should be happening)
The criteria need to be decided first. This needs to be a simple statement about the delivery of service or patient care. It does not need to be a summary of all aspects of care but should focus on key points that are clinically relevant, clearly defined and measurable.
The next step involves setting the standard. This can be one of the most difficult areas and stimulates a lot of discussion. Standards should be:
- Realistic
- Measurable
- Achievable
- Agreed
The audit will compare current practice against what is seen as a desirable standard of care.There are different ways of setting standards and negotiation will be needed, especially in multiprofessional settings. If someone’s views are overlooked their commitment to the audit will not be as strong.
Standards may vary from one place to another, eg, in a PCO standards may differ from practice to practice, for instance if a practice is single-handed or part of a group.
Guidelines may be available or drawn up. These differ from the audit standard in that they will cover all aspects of the patient’s management whereas the standard will focus on one aspect only.
Step 2.Collect data (what is actually happening)
To carry out an audit and compare current practice to the standard set, data (information) need to be collected.It is important to collect appropriate data only and to keep data collection as simple as possible. It is easy to get carried away and collect too much data. The aim of an audit is not to collect as much data as possible and produce lists of statistics.
Step 3. Analyse audit data (compare results)
There should be no need for a high degree of expertise in statistics although statistics may need to be used.
When evaluating the results several points need to be considered:
- Was the information collected complete and accurate? Was all the information collected in busy periods?
- Did anything exceptional happen during the audit that might affect the results, eg, staff sickness, locum cover?
Whoever collects the data needs to make sure that they:
- Concentrate on answering the audit questions
- Make sure the time and place are suitable for any participants
- Allow time for questions and discussion
If changes in practice are needed, it will be necessary to think about explaining why: commitment to change will not be present if participants are not sure why change isneeded.
When completed the audit should provide a fair representation of normal practice. The audit results may be confidential but the group involved should have the chance to discuss them
Step 4. Identify cause(s) of non-achievement (decide on change)
This is where the multiprofessional team involved needs to consider whether the standard has been met. If the standard has not been met, then the audit should have produced information about what changes are needed to improve practice and therefore meet the standard in future. If the standard has been met, the results of the audit may show a way of making further improvements.
Step 5. Implement changes (making the change)
Changes in working practices can be difficult to bring about. Involving the relevant people in the audit will make implementing any changes easier. Ownership of the audit is vital. If change in practice is needed, participants must be able to see why or commitment to change will not be present.
Step 6.Monitor progress (was the change successful?)
This is where the cycle continues. If changes are made to practice, with a view to evaluating their success, then performance needs to be remeasured after making the change and the audit cycle must begin again.

