This content was published in 2014. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Oral medicine often requires the use of off-label treatments to manage complex conditions such as recurrent aphthous ulceration, oral lichen planus and mucous membrane pemphigoid.
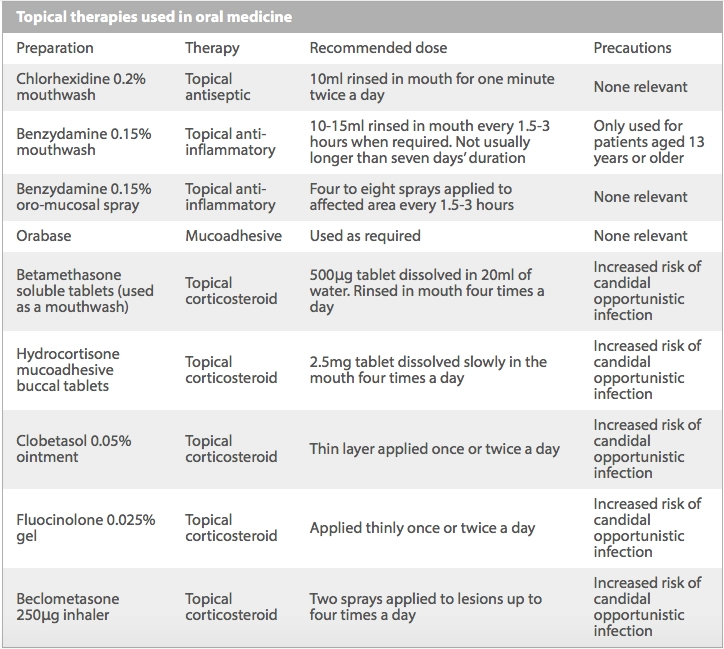
Pharmacists need to be aware of the main counselling points for patients, particularly around the use of topical corticosteroids.
The management of oral medical conditions can be complex. Although they may be managed in primary care by a dentist, more commonly patients are referred to an oral medicine specialist centre and their treatment requires a multidisciplinary approach.
Pharmacists have an important role in supporting these patients, because treatment can involve the use of off-label and extemporaneously prepared medicines that require comprehensive counselling for their use.
This article looks at three oral conditions that pharmacists may encounter.
Recurrent aphthous ulceration
An ulcer is a break in the oral epithelium. This exposes the nerve endings present in the underlying connective tissue,[1] which can often lead to pain and discomfort.
There are numerous causes of oral ulceration. These range from local trauma to ulceration secondary to systemic diseases (eg, Crohn’s disease, leukaemia, iron deficiency) or drug therapy (eg, nicorandil, cytotoxic medicines). Oral malignancy may also present as persistent ulceration, and any ulcer that lasts for more than three weeks with no sign of resolution requires referral to a GP or dentist for further investigation.[2]
The most common cause of oral ulceration is recurrent aphthous ulceration (RAU), which can affect up to 20% of the population[3]. RAU is more common during periods of stress, during and after stopping smoking, and in higher socio-economic populations.
RAU is characterised by recurrent episodes of single or multiple mouth ulcers with no identifiable cause, and therefore diagnosis can only be made following exclusion of local or medical causes. It is generally diagnosed from a patient’s clinical history; histopathological and haematological investigations may also be performed to ensure the ulceration is not caused by a systemic disorder.
RAU episodes are managed by relieving a patient’s symptoms, and an individual approach to treatment is required.
Barrier agents (eg, Orabase) are useful in the management of minor ulceration.[3] These adhere to the mucosa, preventing irritation and infection and promoting healing. The mucosa should be as dry as possible before application. This ensures the agent will adhere to the mucosa, protecting the specific area of the mouth.
Topical anti-inflammatories, such as benzydamine 0.15% mouthwash and spray, are also useful in managing the inflammation that occurs when a break in the epithelium develops. The mouthwash should be used undiluted, but can be diluted with water if stinging occurs.
Topical corticosteroids are considered the main treatment for aphthous ulceration. They help reduce the inflammatory response, which in turn helps to reduce pain.
Topical corticosteroids suppress the local flora and can cause an overgrowth of Candida spp, which can complicate therapy. Candidiasis can be managed by reducing or stopping the corticosteroid treatment (if appropriate) and applying a topical antifungal, such as miconazole gel, to help control the infection. Systemic corticosteroids, dapsone and colchicine can be prescribed for more severe cases of RAU that are unresponsive to topical therapy.[4]
The Cochrane Collaboration has conducted a review of systemic interventions for aphthous ulceration.[3] This review highlighted the lack of well designed randomised controlled trials, and as a result found that no single treatment was found to be significantly more effective than any other.

Source: Bristol Dental Hospital
Medical photograph showing aphthous ulcer
Oral lichen planus
Oral lichen planus (OLP) is a chronic mucocutaneous disorder that affects 1% of the population.[5] Its appearance can range from white striated lesions to ulcers and atrophy, with a variable degree of pain or discomfort.
For some patients, OLP can be asymptomatic and treatment is not necessary.[5] However, other patients may have severe erosive lesions involving multiple mucosal surfaces and extensive areas of ulceration. Such extreme disease can interfere with feeding and oral hygiene, and can have an adverse effect on quality of life.
OLP tends to last for several years, with periods of symptoms and remission. Although the exact disease process is not fully understood, it is known to be immune-mediated. OLP is considered to be a potentially malignant condition and around 1% of patients develop malignancy over a 10-year period. Patients need to be aware that they require regular follow-up with a dentist or specialist. The interval between appointments varies from three months to a year depending on the severity of symptoms, risk factors and a patient’s medication.
Treatment is based on the severity of symptoms. Analgesic and antiseptic mouthwashes can be used to reduce soreness and prevent secondary infection.[6]
Typically, patients with mild inflammation who present with localised atrophic or erosive lesions will respond to topical corticosteroids. The Cochrane reviews on OLP treatments could find no evidence that one topical steroid is better than another.[6],[7]
Patients with severe OLP may not respond to topical treatment. Treatments prescribed in specialist oral medicine units may include the calcineurin inhibitor tacrolimus in an adhesive base, applied topically. The British Society of Oral Medicine guidelines state that calcineurin inhibitors should be second-line in the treatment of OLP.[5]
The Medicines and Healthcare products Regulatory Agency (MHRA)[8] has issued a warning about using tacrolimus topically because post-marketing surveillance data suggest there is an increased risk of developing malignancy. There is no strong evidence that use of topical tacrolimus in the mouth carries a similar risk.

Source: Bristol Dental Hospital
Medical photograph showing oral lichen planus
Mucous membrane pemphigoid
Mucous membrane pemphigoid (MMP) is an uncommon auto-immune blistering condition that can affect the mouth. It usually occurs in middle-aged or elderly patients and is more common in women.[9]
It is characterised by blistering, ulceration, erosions and soreness affecting any mucous membrane (eg, mouth, eyes and genitals).[9] The blisters can remain intact for days and can often be filled with blood.
If a diagnosis of MMP is suspected, the patient should be referred to an ophthalmologist because scarring of membranes in the eye can occur, leading to blindness. Patients with MMP should be managed by a multidisciplinary team including dermatology, oral medicine and ophthalmology specialists.
Although mild-to-moderate MMP can be managed with topical corticosteroids, moderate-to-severe MMP is unlikely to be controlled sufficiently with topical treatment alone and immunosuppressants such as azathioprine and mycophenolate mofetil are often prescribed. The use of these immunosuppressants is off-label but widely accepted in oral medicine specialist practice.[9],[10]
A Cochrane review of treatment for MMP suggests that more trials are needed to determine which therapy is the most effective.[10]

Source: Bristol Dental Hospital
Medical photograph showing mucous membrane pemphigoid
Topical corticosteroid counselling points
Adhesive medication
Clobetasol ointment 0.05% can be mixed with Orabase to allow it to adhere to the oral mucosa. Patients should mix the clobetasol with Orabase in a 1:1 ratio and apply it to the lesion inside their mouth. The lesion should be as dry as possible before application to ensure the mixture adheres.
Mouthguards
Fluocinolone gel 0.025% and its dilutions can be placed into a specially designed mouthguard to ensure good contact with the gingivae — this is usually made by the patient’s own dentist in line with directions from an oral medicine team. The strength of gel prescribed will normally decrease as the patient’s condition improves.
Inhalers
Corticosteroid inhalers are often used to deliver steroids to the mucosa. Patients should be advised to direct the inhaler toward the lesion and deliver a dose.
Mucoadhesive buccal tablets
Hydrocortisone mucoadhesive buccal tablets can be held by the tongue against the affected area and allowed to dissolve in the mouth.
Betamethasone as a mouthwash
Soluble betamethasone can be used as an oral rinse, with one tablet dissolved in 20ml of water. Patients should be told not to swallow the solution.
References
- Scully C, Felix DH. Oral Medicine –— update for the dental practitioner. Aphthous and other common ulcers. British Dental Journal 2005;199:259–64.
- National Institute for Health and Care Excellence. Referral guidelines for suspected cancer. June 2005 (modified April 2011) www.nice.org.uk/cg27 (accessed 1 July 2014).
- Brocklehurst P, Tickle M, Glenny AM, et al. Systemic interventions for recurrent aphthous stomatitis (mouth ulcers). Cochrane Database of Systematic Reviews. September 2012. www.onlinelibrary.wiley.com/doi/10.1002/14651858.CD005411.pub2/abstract (accessed 1 July 2014).
- British Society for Oral Medicine. Recurrent aphthous stomatitis (recurrent mouth ulcers). January 2011. www.bsom.org.uk/wp-content/uploads/pdf/BSOM-PiL-Recurrent-Aphthous-Stomatitis-Jan-2011.pdf (accessed 1 July 2014).
- British Society for Oral Medicine. Oral lichen planus. October 2009. www.bsom.org.uk/wp-content/uploads/pdf/BSOM-PiL-Lichen-Planus-Oct-2009.pdf (accessed 1 July 2014).
- Thongprasom K, Carrozzo M, Furness S, Lodi G. Interventions for treating oral lichen planus. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No.: CD001168. DOI: 10.1002/14651858.CD001168.pub2.
- Cheng S, Kirtschig G, Cooper S, Thornhill M, Leonardi-Bee J, Murphy R. Interventions for erosive lichen planus affecting mucosal sites. Cochrane Database of Systematic Reviews 2012, Issue 2. Art. No.: CD008092. DOI: 10.1002/14651858.CD008092.pub2.
- Medicines and Healthcare products Regulatory Agency. Tacrolimus ointment (Protopic): Reminder of a possible risk of malignancies including lymphomas and skin cancers. June 2012. www.mhra.gov.uk/safetyinformation/drugsafetyupdate/CON155759 (accessed 1 July 2014).
- British Society for Oral Medicine. Oral pemphigoid. October 2009. www.bsom.org.uk/wp-content (accessed 1 July 2014).
- Kirtschig G, Murrell DF, Wojnarowska F, Khumalo NP. Interventions for mucous membrane pemphigoid and epidermolysis bullosa acquisita. Cochrane Database of Systematic Reviews 2000, Issue 4. Art. No.: CD004056. DOI: 10.1002/14651858.CD004056.


