Key points
- There are patient safety risks associated with medicines use when patients are discharged from hospital;
- Community pharmacy can help support patients with their medicines;
- An evaluation of a transfer of care around medicines service highlighted the type of services, such as medicines use reviews, provided by community pharmacists;
- The most common intervention provided by pharmacists was education and information about medication during the patient follow-up.

Source: Shutterstock.com
Community pharmacy is becoming increasingly involved in the follow-up care of patients who are discharged from secondary care
Introduction
It has been well demonstrated that patients experience discontinuity of care at hospital discharge, which can potentially endanger their safety as the process carries a risk of medication-related problems, adverse events and even readmissions[1],[2],[3],[4]
. A study by Karapinar-Çarkıt et al. suggested that there are three causes of medication errors at transitions of care: insufficient patient information; insufficient communication between healthcare providers; and incomplete medication lists, with subsequent inappropriate medication reconciliation[5]
. Primary care providers, such as the patient’s general practitioner (GP), are often not informed, or not informed in a timely manner, of medication changes that occurred during hospital admission and the reasons for these changes[4]
. Therefore, GPs can have difficulties in monitoring a patient’s entire medication regimen following a hospital admission[6],[7]
.
Community pharmacy services are, however, transforming to become more clinically focused. For example, community pharmacy is becoming increasingly involved in the follow-up care of patients who are discharged from secondary care, back into the community[8]
. Community pharmacists (CPs) can bridge this transition in care, because of their accessibility and the continuity of care they provide for many of their patients. Providing such a service could enable CPs to help resolve medication-related problems after discharge[8]
. Studies have highlighted CPs willingness to provide discharge medicines support, recognising that measures to improve the accessibility of information for CPs, integrate them more fully into primary care teams and promote the advanced services they offer, would enhance the level of care they can provide to patients after hospital discharge[9],[10]
. However, despite extensive efforts to improve care transitions, CPs are still confronted with problems, such as not knowing when a patient had been in hospital, or not being aware that a patient’s medication had changed, owing to inadequate documentation at discharge[11]
.
Transfer of care services, or transfer of care around medicines (TCAM) as they have been named in England, have been developed, promoted and evaluated in many countries, though the actual service or intervention provided by the CP varies depending on its nature and location[8],[12]
. As there is no national specification on how the service should be delivered, differences exist in the cohorts of hospital inpatients targeted for a TCAM service, and the capacity that hospital pharmacy teams have to engage with these patients may vary across sites. The electronic platforms that are used to refer patients to the CP may have different functionality, and there may be different levels of engagement among CPs to respond to such a (currently unremunerated) referral. These factors mean that there is a lack of consistency and scale in how TCAM services are provided.
Although several English studies have investigated the benefits of TCAM, such as a reduced readmission rate, there are limited details on the interventions or actions undertaken by the CPs that could prevent readmission, with some studies providing limited description of how the CP provided care to the patient[13],[14]
[15]
. This is in contrast to other community pharmacy clinical services, where analysis of the specific interactions between the CP and the patient has been undertaken, demonstrating that CPs can allay minor concerns related to taking medicines, and provide an opportunity for the patient to ask questions about any new medicines[16],[17]
.
Transfer of care in medicines service in Cornwall
The TCAM service at our 750-bed teaching district general hospital in Cornwall was introduced in late 2013, following national guidance[18]
. Although there are several electronic referral systems available, such as Refer-to-Pharmacy, we use the PharmOutcomes software to facilitate a secure method of electronic transfer of information related to medicines between hospital and community pharmacies[19],[20]
. In our TCAM service, hospital pharmacy staff (e.g. pharmacy technicians and clinical pharmacists) discuss with adult patients how they may benefit from a follow-up consultation with a CP during the medicines reconciliation process at the point of admission. There are no patient eligibility criteria (e.g. age, number of prescribed medicines) applied when offering this service, other than the patient responding to the medicines reconciliation process and nominating a community pharmacy based in Cornwall.
The patient is informed that their medication details at discharge will be communicated to their CP, who may then contact them once they have left the hospital. The patient is asked to nominate their regular community pharmacy to receive this electronic communication. At this stage, the relevant patient details are entered into the PharmOutcomes platform. Then, at discharge, the community pharmacy receives an electronic notification on the PharmOutcomes platform. This communication includes a list of the discharge medication. These referrals can either be accepted or rejected (as described elsewhere)[21]
. Rejections require the pharmacist to complete a note box selecting the reason for rejection (e.g. CP unable to contact the patient). Patients are not informed that their referral has been rejected. If the community pharmacy does not acknowledge the referral or carry out further action, the status of that referral remains ‘referred’.
Subsequent to the consultation with the patient, pharmacists select the services they have provided from a number of drop-down menus on PharmOutcomes, which may capture multiple services for the same patient (e.g. medicines use review [MUR] and a new medicines service [NMS]). An overview of the drop-down menus and general advice for CPs on how to complete the referral documentation in PharmOutcomes, including a prompt about any possible adverse drug reactions (ADRs), has been described elsewhere[22]
. However, it is important to note that this is not a standardised view, as some of the service options may differ between health communities in different parts of the country. The Figure provides an illustration of the service stages from the perspective of the CP.
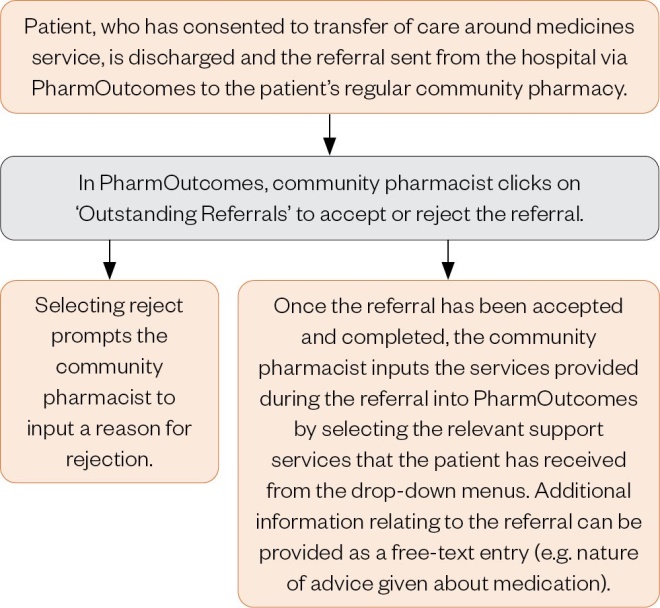
Figure: Illustrating the TCAM service from the community pharmacist perspective
Examples of the service options available can be seen in Box 1. This TCAM service is not a remunerated service for the CP, although patients may be eligible for an MUR or NMS.
Box 1: Example of service options available on PharmOutcomes
- Commenced monitored dosage system;
- Home delivery;
- Medicines use review;
- Medicines reconciliation;
- New medicines service;
- Pharmacy managed repeat service;
- Review monitored dosage system arrangements;
- Other.
This study aimed to retrospectively analyse the Royal Cornwall Hospitals NHS Trust community pharmacy TCAM service to describe the type of medication-related problems identified during pharmacist consultation with patients and the services provided.
Method
Participants
At the time of the study, there were around 2,000 discharges per month (adults and children) from the Royal Cornwall Hospital NHS Trust, although only around 15% attracted a TCAM service. There were 104 community pharmacies across Cornwall during this period, but not all were expected to receive discharge referrals owing to their distance from the hospital.
Study design
This was a retrospective service evaluation based on relevant data extracted from PharmOutcomes in September 2019, from 1 April 2018 to 31 March 2019.
Analysis
Quantitative data relating to service activity were analysed, using descriptive statistics, and converted to percentages, where appropriate, to represent proportions. The authors quantified all services provided by the CP, noting that some patients were recorded as receiving more than one service. Additional comments, which can be made on the PharmOutcomes platform by the CP as free-text entries, were collated, manually coded by two of the authors (MW and FL), and then analysed. The coding of these drug-related problems (DRPs) used the DOCUMENT classification system[23]
. This system, designed for the community pharmacy setting, has been used and refined in studies spanning more than ten years of research into DRP detection and resolution by CPs. It is comprehensive and focuses on prescribing, dispensing, medication administration, patient knowledge, compliance to therapy and the need for monitoring. The DOCUMENT system consists of eight main categories, broadly defining DRPs as: drug selection; overdose; compliance; undertreated; monitoring; education; not classifiable; and toxicity[23]
.
Data were quantitatively analysed using Microsoft Excel.
Ethical approval was not sought, because this was a retrospective assessment, involving no changes to the service delivered to patients. The principles of ethical research, such as confidentiality, anonymity and consent, were followed.
Results
A total of 3,443 discharge referrals were made during the 12-month period (mean patient age 72 years, 49% female) provided to 92 unique pharmacies. Removing rejected and non-completed referred records left 38% (n=1298) that were actioned (mean patient age 72 years, 48% female). Of these 1298 referrals, the services provided were MUR recorded for 50.0% (n=649) of patients; medicines reconciliation for 8.0% (n=104); commencement or review of monitored dosage system for 7.3% (n=95); NMS for 5.3% (n=69); and instituting a pharmacy managed repeat service for 5.1% (n=66). Other additional pharmaceutical or support services (e.g. home delivery, medicines administration record chart, review dose form) that were provided less frequently were also recorded, while services were recorded as not provided for 26.8% (n=348) of patients.
Pharmacists recorded instances of ADRs in 5.3% (n=69) of patients, of which 50 were associated with an MUR or NMS provision. There were 46 instances categorised as ADR that were manageable and non-harmful (i.e. patient fine to continue drug), and in 23 cases the patient had stopped taking the medicine (and was to be referred to GP). In none of these 69 instances was it recorded that the pharmacist had completed a Yellow Card.
Additional actions were recorded in free text for 26.9% (n=349) of the 1,298 referrals. Of these free-text entries, 43.2% (n=151) were recorded for patients noted as receiving an MUR; 3.4% (n=12) were for those who received medicines reconciliation; 2.9% (n=10) for commenced or reviewed monitored dosage system; and 2.6% (n=9) for an NMS. This brief text entry attempted to capture the outcome of the follow-up consultation between the pharmacist and the patient or carer, such as helping to clarify patient concerns about their medicines. The categorisation of the free-text entries according to DOCUMENT is shown in the Table.
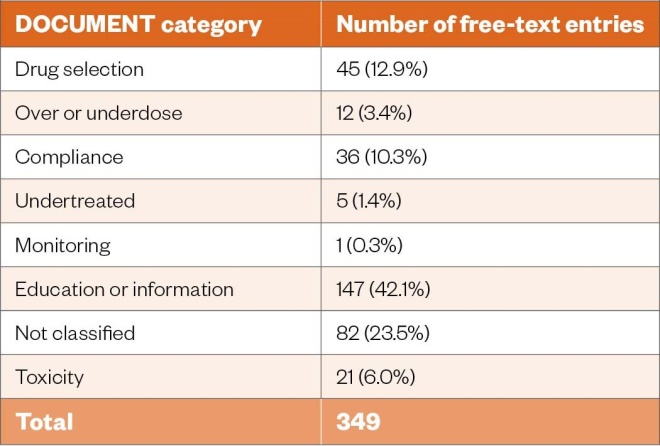
Table: Categorisation of free-text entries using the DOCUMENT system
Examples of free text provided for the main categories are shown in Box 2.
Box 2: Free-text examples included for each of the main DOCUMENT categories
Education or information
- “The patient was a bit concerned about some of her medication, but we went through all of them and she is now reassured and happy to carry on”;
- “Reassured patient regarding rivaroxaban”;
- “No new or changed long-term medicines following this admission”.
Drug selection
- “Helped patient to order her medications and advised her to stop Epilim, as stated on discharge letter, as she is on levetiracetam now. Counsel medicine changes”;
- “Patient in contact with GP to get apixaban added to repeat slip”.
Compliance
- “Blister pack chart/meds updated. Repeat rx for meds correct and in place”;
- “Patient has got difficulties taking the medication, has decided to put him on blister pack”.
Toxicity
- “Patient urgently need another INR test and maybe warfarin reversal if still too high”;
- “Asthma well controlled, concerned antibiotic making her feel faint”.
Discussion
Concerns related to patient safety problems arising from suboptimal transfer of care at discharge are recognised globally[4]
. There is increasing interest in the role of community pharmacy in managing medication safety when patients leave the hospital setting, with the nature and intensity of the services provided differing from country to country[24],[25]
. In the UK, for instance, a funded discharge medicines review service was introduced in Wales in 2011[26]
. This is a two-part, CP-led service which includes identifying discrepancies between the first prescription post-discharge and the discharge advice letter, followed up by a supportive medication review focused on adherence. In Scotland, there is no such formal service, although the pharmacy care record is one of two main avenues for sharing information between secondary care and primary care. In England, a TCAM service is now expected to be an essential community pharmacy service from January 2021[27]
.
Although involving CPs in medication management after discharge can reduce DRPs (e.g. through reconciliation against the patient’s repeat prescription to reduce unintentional changes or errors), the evidence for humanistic benefits, such as improved quality of life or influences in patients’ daily functioning, is limited and conflicting[8],[15],[28]
.
Our study has shown that following hospital discharge, CPs, as part of a TCAM service, provided a range of services in around three-quarters of the followed-up patients, including undertaking MURs, medicines reconciliation, introduction of a monitored dosage system, undertaking NMS, and implementing a pharmacy managed repeat service. A 2016 study by Nazar et al. also used the PharmOutcomes platform, although the drop-down options of services offered may have been different to ours, as this menu is not standardised on PharmOutcomes across the country[13]
. In the study by Nazar et al., 2,029 inpatients were referred, though only 31% (n=619) received a follow-up consultation. This high rejection or drop-out rate means that a large proportion of patients were not able to take advantage of the interaction with the CP. Ascertaining why referrals were not accepted or rejected, and the outcome for these patients, requires further research.
Most of the completed referrals by Nazar et al. did not receive any additional pharmaceutical or support services (53.4% compared with our value of 26.8%)[13]
. Of those who did receive a service, Nazar et al. reported 46.6% received an MUR (compared with our value of 50.0%), 38.9% were enrolled on the NMS (compared to our value of 5.3%), and 4.5% received medicines reconciliation (compared with our value of 8.0%). It is unclear why there is such a difference in the proportion of patients enrolled in the NMS. Nazar et al. analysed 2014–2015 data, whereas this study analysed data from 2018–2019; over this period there has been an increase of around 20% in the total number of NMS provided by community pharmacies in England[29]
. The disparity may reflect the types of new medicines that patients were taking at the time of discharge from the respective hospitals. We have not analysed how many of our patients were taking medicines that would be eligible for an NMS, although there were differences in the proportion of patients with specific conditions. For example, a cardiovascular condition was reported in 53.0% (n=328) of patients by Nazar et al., compared with 22.8% (n=296) in this study, and a respiratory condition was reported for 20.4% (n=126) of patients by Nazar et al., compared with 7.6% (n=99) in this study[13]
.
The proportion of patients who received information from the CP on their medication also differed between the studies. Nazar et al. reported 90.0% (n=557) received ‘more information on medication’ and 84.2% (n=521) had a ‘side effect check’, whereas only 68.3% (n=886) of patients in our study were recorded as receiving information relating to medication from any of the three categories of ‘the purpose of their medication’, ‘when or how to take their medication’ or ‘when to take or use their medicines’[13]
. It is uncertain if this difference is owing to factors such as our patients not requiring the same degree of support on their medication; pharmacists not recognising that such medication information was needed; or information being provided, but such action not being recorded on PharmOutcomes.
Nazar et al. reported that most patients did not report an ADR to the CP during the consultation. In the 65.4% (n=106/162) of patients who did, the ADR was considered manageable and non-harmful to the patient, and thus patients were advised to continue taking their medication as prescribed[13]
. In our study, CPs identified 46 ADRs (66.7%) as manageable and non-harmful to the patient. Completion of a Yellow Card was not recorded on PharmOutcomes by the CP in the 23 cases where the patient had ceased taking the medicine because of an ADR, though we do not know if other action was taken and not recorded. This may be owing to time pressure, or lack of confidence in identifying and knowing how to report ADRs[30]
. A negligible rate of Yellow Card reporting by community pharmacy has been observed in an analysis of the NMS, while underreporting of ADRs by a range of health professionals has been reported[31],[32]
. Underreporting of ADRs has an impact on the benefit/risk evaluation of medicines, as such reports are important tools in helping to monitor medicine safety.
The DOCUMENT categorisation system was used in an attempt to determine the nature of the discussion and interaction that occurred between the CP and the patient or carer. Education or information was the most frequent category of free-text entry in 42.1% (n=147) of instances, followed by not classified (n=82; 23.5%), drug selection (n=45; 12.9%) and then compliance (n=36;10.3%). The category of education and information covered a broad range of free-text entries, some of which quite clearly suggested that specific medication advice was provided to the patient, while other entries were more general (e.g. ‘No new or changed long-term meds following this admission’). We also noted that commencement or review of a monitored dosage system was recorded for 7.3% (n=95) of patients. There is much interest in tackling the problem of medication adherence; however, the long-term effectiveness of CP services, such as NMS, remains uncertain, while the provision of monitored dosage systems is increasingly seen as controversial because of issues such as reduced medicine stability and increased medicines wastage[33],[34]
.
Studies reporting on CP involvement at transitions of care in other countries, although of interest, are not directly comparable to the English setting. An evaluation of a pharmacy-led transitional care programme across two hospitals and 50 community pharmacies in the Netherlands by Daliri et al. recorded interventions initiated by the CP at home visits into three categories[35]
:
- Discrepancies (e.g. correcting unintentional differences between the documented medication in the discharge letter and actual medication use of the patient registered during the home visit);
- Optimisation of medication;
- Patient handling interventions (e.g. improving patients’ medication use by providing advice on adherence issues, education relating to medication indication, advice on time of administration and intended duration of treatment)[35]
.
Daliri et al. concluded that a pharmacy-led transitional care programme reduced medication-related problems after discharge, but advised that implementation research was needed to determine how best to embed these interventions in existing processes[35]
.
An American study, using trained ambulatory pharmacists to provide comprehensive medication management (CMM) before and after hospital discharge, reported that during the ambulatory CMM intervention delivered to 61 patients, medication ‘non-adherence’ and ‘lack of needed drug’ were the most common medication problems identified and resolved (each identified in 25%; n=15 patients), followed by ‘lack of understanding’ (19.7%; n=12 patients) and ‘adverse drug reaction’ (18.0%; n=11 patients)[36]
.
Likewise, a further study from the Netherlands looked at a collaboration between hospitals and CPs, with an intervention that comprised of medication verification and counselling at admission, medication screening by the hospital pharmacist during admission, outpatient pharmacy discharge consultation and support, and a CP home visit within one week post-discharge, using a modified version of DOCUMENT[25]
. In this study, a total of 745 DRPs were identified, with CPs identifying the majority (83.6%; n=623) during the home visit for 152 patients, of which the most frequently identified types of DRPs were the need for additional ‘education or information’ (39.0%; n=243), ‘compliance’ issues (17.7%; n=110), and ‘non-clinical’ (11.7%; n=73).
If patients are confused or uncertain about changes to their medicines after a hospital admission and wish to undertake medication communication with healthcare professionals, this could provide a useful opportunity for the involvement of CPs in TCAM services. NHS England sees TCAM as an essential way to achieve medicines optimisation and improve patient safety, and has commissioned Academic Health Science Networks to roll out the service to 50% of acute NHS trusts by the end of 2020[37],[38]
. It had been envisaged that it would be possible for hospitals to digitally refer recently discharged patients to community pharmacies across England for advice on new and updated prescriptions from July 2020, though this timeline has slipped[39]
.
Limitations
The authors acknowledge the limitations of this study, which only analysed instances of completed referrals, and did not delve into why referrals were rejected or not actioned, nor tried to understand why around a quarter of followed-up patients did not receive any service. Classifying DRPs is an important part of pharmaceutical care practice and research, yet there is no universally accepted classification system[40]
. The DOCUMENT system was designed by Australian CPs to classify DRPs and has not been validated for the service described in this study. There is a lack of evaluation of the quality of the documentation (i.e. accuracy, meaningfulness). It should be noted that some of the free-text entries in the database, which are not mandatory to make, were often vague, as some CPs were less thorough in their documentation, making the categorisation of issues difficult. We relied on CPs for the completeness of documentation in the PharmOutcomes platform, who in some cases may have addressed issues during consultations that they failed to document. If this is the case, the overall number of issues identified may have been underestimated. The categorisation of issues introduced bias to the study owing to their subjective nature. Patients were only followed up once, and it is not possible to judge the impact of the advice provided by the pharmacists. In addition, only certain patient demographic details were captured (i.e. age, gender), and not the full range of possible comorbidities.
Future developments
With the future demise of the MUR service, and the wider roll-out of a TCAM service as an essential community pharmacy service across England from January 2021, we intend to refocus action locally, in conjunction with relevant stakeholders, to increase the proportion of referrals that are actioned by CPs[27],[41]
. The promotion of the role of CPs in Yellow Card reporting also represents another potential area of future work. Unfortunately, the COVID-19 pandemic has dramatically altered the responsibilities and workflow of CPs, meaning the additional training, education and campaigns needed to promote and improve the service cannot currently be prioritised. The synthesis that Luetsch et al. give for the contexts and mechanisms that can be activated to influence the outcomes of pharmacist conducted medication reviews provides guidance for the future development of a TCAM service[42]
.
Conclusion
The transition from hospital to home is a recognised source of medication-related problems, that may lead to hospital readmission. Interventions or services bridging this transition, such as self-management education, telephone follow-up and medication reconciliation activities, can support patients’ medication continuity and may help reduce hospital readmission caused by medication-related problems. When provided with discharge medication details, CPs can provide education and information and address patients’ medication concerns via a post-discharge follow-up. This service allows CPs to potentially contribute to improved medicines optimisation and adherence.
About the authors
Michael Wilcock is the head of the Prescribing Support Unit at Royal Cornwall Hospitals NHS Trust; Liam Bastian is lead pharmacist for ePrescribing and Digital Medicines at Royal Cornwall Hospitals NHS Trust; and Fiona Lee is a pharmaceutical advisor for NHS Kernow Clinical Commissioning Group.
Correspondence to: mike.wilcock@nhs.net
Financial and conflicts of interest disclosure
The authors have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in this manuscript. No writing assistance was used in the production of this manuscript.
References
[1] Williams H, Edwards A, Hibbert P et al. Harms from discharge to primary care: mixed methods analysis of incident reports. Br J Gen Pract 2015;65:e829–837. doi: 10.3399/bjgp15X687877
[2] Parekh N, Ali K, Stevenson JM et al. Incidence and cost of medication harm in older adults following hospital discharge: a multicentre prospective study in the UK. Br J Clin Pharmacol 2018;84:1789–1797. doi: 10.1111/bcp.13613
[3] Himmel W, Kochen MM, Sorns U et al. Drug changes at the interface between primary and secondary care. Int J Clin Pharmacol Ther 2004;42(2):103–109. doi: 10.5414/CPP42103
[4] World Health Organization. Medication safety in transitions of care. 2019. Available at: https://www.who.int/patientsafety/medication-safety/TransitionOfCare.pdf?ua=1 (accessed December 2020)
[5] Karapinar-Çarkıt F, Borgsteede SD, Zoer J et al. The effect of the COACH program (Continuity Of Appropriate pharmacotherapy, patient Counselling and information transfer in Healthcare) on readmission rates in a multicultural population of internal medicine patients. BMC Health Serv Res 2010;10:39. doi: 10.1186/1472-6963-10-39
[6] Kattel S, Manning DM, Erwin PJ et al. Information transfer at hospital discharge: a systematic review. J Patient Saf 2020;16(1):e25–e33. doi: 10.1097/PTS.0000000000000248
[7] Markiewicz O, Lavelle M, Lorencatto F et al. Threats to safe transitions from hospital to home: a consensus study in North West London primary care. Br J Gen Pract 2019;70:e9–e19. doi: 10.3399/bjgp19X707105
[8] Nazar H, Nazar Z, Portlock J et al. A systematic review of the role of community pharmacies in improving the transition from secondary to primary care. Br J Clin Pharmacol 2015;80(5):936–948. doi: 10.1111/bcp.12718
[9] Veerena JC, Rogers PJ, Taylor ADJ et al. Improving communication across the primary–secondary care interface: a survey of the attitudes and experiences of community pharmacists in England. Int J Pharm Pract 2019;S2:9–10. doi: 10.1111/ijpp.12532
[10] Urban R, Paloumpi E, Rana N et al. Communicating medication changes to community pharmacy post-discharge: the good, the bad, and the improvements. Int J Clin Pharm 2013;35:813–820. doi: 10.1007/s11096-013-9813-9
[11] Hodson KL, Blenkinsopp A, Cohen D et Âal. Evaluation of the discharge medicines review. 2014. Available at: http://www.cpwales.org.uk/Contract-support-and-IT/Advanced-Services/Discharge-Medicines-Review-(DMR)/Evaluation-of-the-DMR-Service/Evaluation-of-the-DMR-service.aspx (accessed December 2020).
[12] Clark C. Transfer of care: how electronic referral systems can help to keep patients safe. Pharm J 2016;297(7891). doi: 10.1211/PJ.2016.20201492
[13] Nazar H, Brice S, Akhter N et al. New transfer of care initiative of electronic referral from hospital to community pharmacy in England: a formative service evaluation. BMJ Open 2016;6(10):e012532. doi: 10.1136/bmjopen-2016-012532
[14] Hockly M, Williams S & Allen M. Transfer of care – a randomised control trial investigating the effect of sending the details of patients’ discharge medication to their community pharmacist on discharge from hospital. Int J Pharm Pract 2018;26(2):174–182. doi: 10.1111/ijpp.12364
[15] Sabir FRN, Tomlinson J, Strickland-Hodge B et al. Evaluating the Connect with Pharmacy web-based intervention to reduce hospital readmission for older people. Int J Clin Pharm 2019;41(5):1239–1246. doi: 10.1007/s11096-019-00887-3
[16] Latif A, Boardman HF & Pollock K. Understanding the patient perspective of the English community pharmacy Medicines Use Review (MUR). Res Social Adm Pharm 2013;9(6):949–957. doi: 10.1016/j.sapharm.2013.01.005
[17] Latif A, Waring J, Watmough D et al. ‘I expected just to walk in, get my tablets and then walk out’: on framing new community pharmacy services in the English healthcare system. Sociol Health Illn 2018;40(6):1019–1036. doi: 10.1111/1467-9566.12739
[18] Royal Pharmaceutical Society. Keeping patients safe when they transfer between care providers — getting the medicines right. 2012. Available at: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Publications/Keeping%20patients%20safe%20transfer%20of%20care%20report.pdf (accessed December 2020)
[19] National Institute for Health and Care Excellence. Refer-to-pharmacy and medicines optimisation. 2017. Available at: https://www.nice.org.uk/sharedlearning/refer-to-pharmacy-and-medicines-optimisation (accessed December 2020)
[20] PharmOutcomes. 2013. Available at: https://pharmoutcomes.org/pharmoutcomes/ (accessed December 2020)
[21] Wilcock M, Kelly L & Yelling P. Discharge communications from hospital to community pharmacy: reasons for rejection. J Pharm Management 2019;35(2):33–37. Available at: https://www.pharman.co.uk/uploads/imagelib/pdfs/Journal_articles_by_issue/JoPM%20Apr%202019/Discharge%20Communications.pdf (accessed December 2020)
[22] South Staffordshire Local Pharmacy Committee. PharmOutcomes referral services TCAM pharmacy follow-up. 2019. Available at: https://psnc.org.uk/south-staffordshire-lpc/wp-content/uploads/sites/95/2019/11/PharmOutcomes-Referral-Service-TCAM-Pharmacy-Follow-up-1.pdf (accessed December 2020)
[23] Peterson G, Tenni P, Jackson S et al. Documenting clinical interventions in community pharmacy: PROMISe III. 2009. Available at: http://6cpa.com.au/wp-content/uploads/Documenting-Clinical-Interventions-in-CommunityPharmacy-PROMISe-III-Final-Report.pdf (accessed December 2020)
[24] van der Heijden AAWA, de Bruijne MC, Nijpels G et al. Cost‑effectiveness of a clinical medication review in vulnerable older patients at hospital discharge, a randomized controlled trial. Int J Clin Pharm 2019;41(4):963–971. doi: 10.1007/s11096-019-00825-3
[25] Ensing HT, Koster ES, Dubero DJ et al. Collaboration between hospital and community pharmacists to address drug-related problems: the HomeCoMe-program. Res Social Adm Pharm 2019;15(3):267–278. doi: 10.1016/j.sapharm.2018.05.001
[26] Andalo D. Discharge medicines reviews in Wales. Pharm J online. 2011. Available at: https://www.pharmaceutical-journal.com/news-and-analysis/discharge-medicines-reviews-in-wales/11088413.article (accessed December 2020)
[27] Wickware C. Digital hospital-to-pharmacy referral service delayed until January 2021. Pharm J 2020;305(7941). doi: 10.1211/PJ.2020.20208305
[28] Lapointe-Shaw L, Bell CM, Austin PC et al. Community pharmacy medication review, death and re-admission after hospital discharge: a propensity score-matched cohort study. BMJ Qual Saf 2020;29(1):41–51. doi: 10.1136/bmjqs-2019-009545
[29] NHS Digital. General pharmaceutical services in England 2008/09 – 2018/19. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/general-pharmaceutical-services/in-2008-09—2018-19-ns (accessed December 2020)
[30] Hughes ML & Weiss M. Adverse drug reaction reporting by community pharmacists — the barriers and facilitators. Pharmacoepidemiol Drug Saf 2019;28(12):1552–1559. doi: 10.1002/pds.4800
[31] Craske M, Youssef E & Twigg M. A descriptive analysis of the New Medicines Service data submitted by English Pharmacy contractors in 2017/18 and 2018/19. Royal Pharmaceutical Society Annual Conference 2019. Medicines Safety Abstract Booklet. R25:28
[32] Hazell L & Shakir SA. Under-reporting of adverse drug reactions. A systematic review. Drug Sa f 2006;29:385–396. doi: 10.2165/00002018-200629050-00003
[33] Franklin BD, Abel G & Shojania KG. Medication non-adherence: an overlooked target for quality improvement interventions. BMJ Qual Saf 2020;29(4):271–273. doi: 10.1136/bmjqs-2019-009984
[34] North East & North Cumbria Academic Health Science Network. Medicines Adherence Support Project. 2019. Available at: http://www.ahsn-nenc.org.uk/wp-content/uploads/2019/02/AHSN-Adherence-Support-Final-Report-January-2019.pdf (accessed December 2020)
[35] Daliri S, Hugtenburg JG, Ter Riet G et al. The effect of a pharmacy-led transitional care program on medication-related problems post-discharge: a before-after prospective study. PLoS One 2019;14(3):e0213593. doi: 10.1371/journal.pone.0213593
[36] Schullo-Feulner A, Krohn L & Knutson A. Reducing medication therapy problems in the transition from hospital to home: a pre- & post-discharge pharmacist collaboration. Pharmacy 2019;7:86. doi: 10.3390/pharmacy7030086
[37] Tobiano G, Chaboyer W, Teasdale T et al. Patient engagement in admission and discharge medication communication: a systematic mixed studies review. Int J Nurs Stud 2019;95:87–102. doi: 10.1016/j.ijnurstu.2019.04.009
[38] Wickware C. Half of hospital trusts to refer to community pharmacy by 2020. Pharm J 2019; 302(7926). doi: 10.1211/PJ.2019.20206557
[39] Wickware C. Government announces digital hospital-to-pharmacy referral service to cut hospital readmissions. Pharm J 2020; online. doi: 10.1211/PJ.2020.20207732
[40] Basger BJ, Moles RJ & Chen TF. Application of drug-related problem (DRP) classification systems: a review of the literature. Eur J Clin Pharmacol 2014;70:799–815. doi: 10.1007/s00228-014-1686-x
[41] Pharmaceutical Services Negotiating Committee. Medicines Use Review (MUR). Available at: https://psnc.org.uk/services-commissioning/advanced-services/murs/ (accessed December 2020)
[42] Luetsch K, Rowett D & Twigg MJ. A realist synthesis of pharmacist-conducted medication reviews in primary care after leaving hospital: what works for whom and why? BMJ Qual Saf. 2020; In press. doi: 10.1136/bmjqs-2020-011418
