Key points
- The advantages and disadvantages of oral rather than intravenous administration of anticancer drugs are summarised.
- The oral bioavailability of many anticancer drugs is low and highly variable because of sub-optimal physicochemical properties or appreciable first-pass metabolism and efflux transport or both.
- Potential solutions to low oral bioavailability include the development of pro-drugs, co-administration with inhibitors of metabolism or efflux transport and formulation in carrier systems.
Introduction
Changes in the treatment of cancer mean that more drugs can be administered orally as well as through the traditional intravenous route. Most patients would prefer to have oral chemotherapy in their home[1],[2],[3],[4] . However, while there are distinct advantages in using oral rather than intravenous administration, not the least being greater convenience and less discomfort, there are some significant disadvantages (see Box 1).Box 1: Advantages and disadvantages of oral anticancer drugs
Advantages- Convenience (administration in the home);
- Avoidance of discomfort and risks of infection, phlebitis and extravasation of intravenous (IV) lines;
- Avoidance of hypersensitivity to IV vehicles (e.g. Chremophore EL®);
- Avoidance of the costs of hospitalisation;
- Modulation of drug release from the dosage form, affording options for optimising effect–time profile;
- More sustained inhibition of target.
- Low and highly variable bioavailability, including dose-limited absorption;
- Non-adherence, incomplete adherence or over-adherence;
- Gastrointestinal side effects (e.g. diarrhoea, cytotoxicity, dyspepsia);
- Gastrointestinal disease and surgery;
- Food–drug and drug–drug (e.g. antacid) interactions;
- Limited dose options;
- Potentially decreased contact with the oncology team;
- Increased costs of developing sophisticated formulations; difficulty in establishing bioequivalence (generics).
The importance of understanding pharmacokinetic properties of oral anticancer therapy
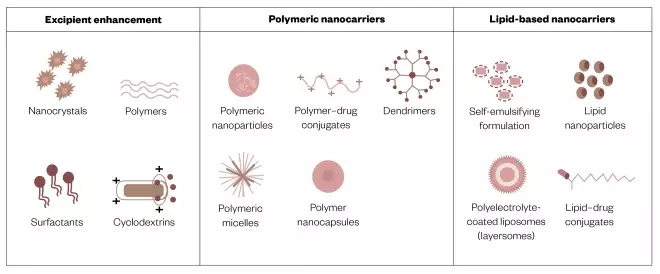
An important class of targeted anticancer drugs is the small molecule tyrosine kinase inhibitors (sTKIs). They are now used widely for cancer chemotherapy and exemplify the need to understand pharmacokinetic properties as a major determinant of successful oral therapy. Although sorafenib showed a three-month survival benefit in phase III clinical trials, a study of survival in real-world patients with advanced hepatocellular carcinoma indicated ineffective treatment (see Figure 1). While this outcome was attributed to more severe disease and worse liver function in the latter patients, additional possibilities include the use of a fixed-dose, tumour heterogeneity, non-adherence and, importantly, highly variable pharmacokinetics (including absorption) — a hallmark of TKIs[9] . Close monitoring of the exposure to these drugs with dose adjustment is essential to their safe and effective use. 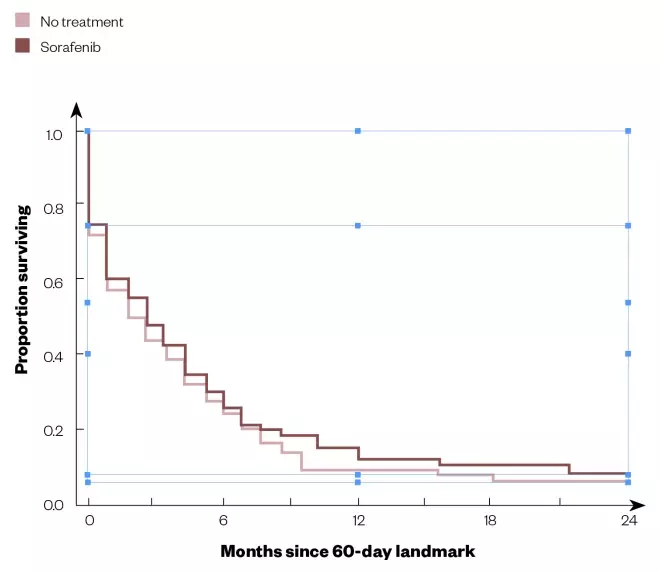
Figure 1: Survival curves for sorafenib treatment versus no treatment in real-world patients with advanced hepatocellular carcinoma
Source: Reproduced with permission from The Oncologist [22]
Kaplan–Meier survival estimates from 60-day landmark of propensity score-matched patients.
Pharmacokinetic barriers related to oral bioavailability
A major problem with many anticancer drugs is their low and variable oral bioavailability. Average absolute bioavailabilities (F) of a range of compounds are shown in Figure 2. While there are some compounds that exhibit complete bioavailability, the range extends well down to virtually zero. In many cases, estimates of oral bioavailability of compounds that are used in this way are not available, reflecting a reluctance to carry out intravenous studies on new compounds intended for oral use only, even though this can be done safely using a micro-dose or nano-dose and allows an understanding of the reason (or reasons) for low bioavailability. 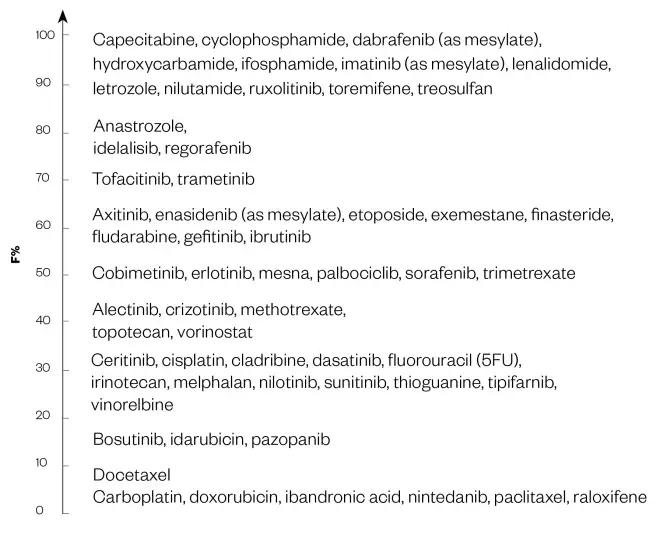
Figure 2: The mean oral bioavailabilities of some anticancer medicines
Source: Values taken from DrugBank
‘F’ indicates the fraction or percentage of the dose that reaches the systematic circulation as intact drug.
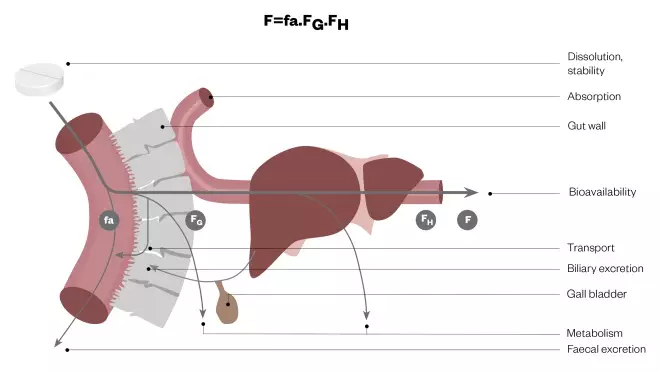
Figure 3: Elements of oral bioavailability
Net bioavailability (F) is seen to be the running product of fa (the fraction of the dose released from the dosage form that dissolves in the gastrointestinal fluid and enters the enterocyte), FG (the fraction that avoids first-pass metabolism and/or efflux transport in the gut wall and is transferred to the liver) and FH (the fraction that avoids first-pass metabolism in the liver and gains entry to the systematic circulation).
- fa — the fraction of the dose released from the dosage form that dissolves in the gastrointestinal fluid and enters the enterocyte;
- FG — the fraction that avoids first-pass metabolism in the gut wall and is transferred to the liver;
- FH — the fraction that avoids first-pass metabolism in the liver and gains entry to the systemic circulation.
Physicochemical properties
Important considerations in the design of drugs for oral use include lipid solubility (as it affects passive permeability across the enterocyte), chemical stability in the gut lumen and aqueous solubility (as it affects dissolution and potential re-precipitation in the gut lumen). Accordingly, structural features contributing to a sub-optimal log P value[11] (representing the partition of drug between octanol and aqueous buffer at a pH of 7.4 as a measure of lipid solubility), poor chemical stability and low aqueous solubility will predict a low fa value. If the log P value is below around –0.4, the compound will have difficulty diffusing across the enterocyte. However, this will be facilitated if the log P value is above around 5, albeit at the expense of a greater difficulty in getting into the solution in the gut lumen. Many oral anticancer drugs have log P values either above or below this optimal range. Poor chemical stability in gastric and intestinal fluids is a primary cause of the low and variable oral bioavailability of etoposide and chlorambucil, for example[7] . The biggest issue in oral bioavailability is often poor aqueous solubility. Although this tends to be inversely related to lipid solubility, medicinal chemists make a distinction between ‘brickdust’ and ‘grease’. While compounds in both categories exhibit low aqueous solubility, those in the former group have a lower lipid solubility than the latter, which might limit their ability to diffuse across the gut wall. The sTKIs have aqueous solubilities that are similar to limestone and quartz (see Figure 4), although they do have reasonable log P values. Thus, their low aqueous solubility rather than a problematic lipid solubility is likely to contribute to the incomplete and variable oral bioavailability of some of these compounds[8],[9] . The balance between membrane permeability and aqueous solubility is reflected in the Biopharmaceutics Classification Scheme[12] , which defines four permutations:- Class 1: high permeability and solubility;
- Class 2: high permeability and low solubility;
- Class 3: low permeability and high solubility;
- Class 4: low permeability and solubility.
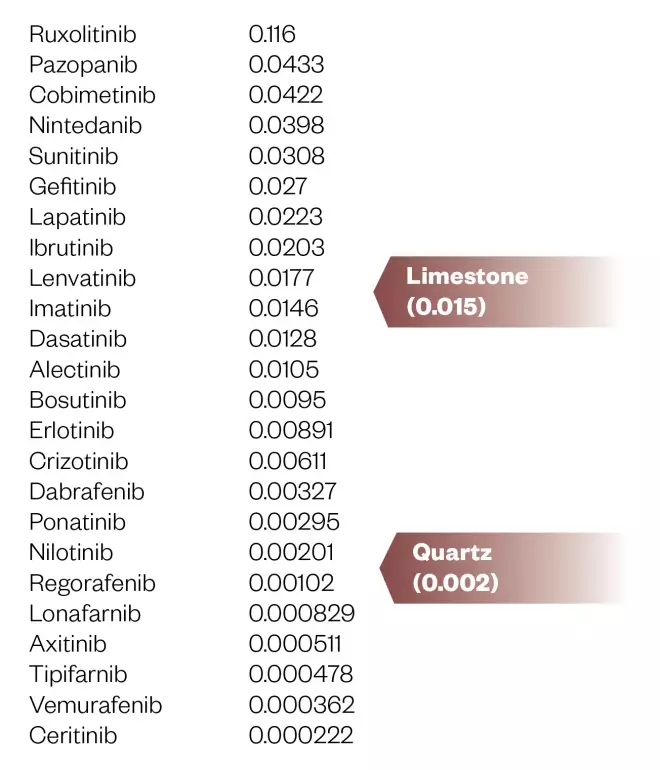
Figure 4: Aqueous solubility (mg/mL) of small molecule tyrosine kinase inhibitors (predicted or experimental)
Data taken from DrugBank
First-pass metabolism and efflux transport
Many anticancer drugs undergo significant first-pass metabolism in the gut wall, the liver or both. 5-fluorouracil (5FU) has an erratic oral bioavailability because of first-pass metabolism by dihydropyrimidine dehydrogenase (DPD) and sTKIs, with the exception of afatinib, which does not appear to be metabolised at all, are to varying extents substrates of intestinal and hepatic CYP3A[7],[8],[9],[13] . Compounding the impact of sub-optimal physicochemical properties and first-pass metabolism on the extent of oral availability is the fact that many anticancer drugs are also substrates of efflux transporters in the gut wall, particularly P-glycoprotein (ABCB1), the multidrug-resistance associated proteins MRP2 and 4 (ABCCCs) and the breast cancer resistance protein BCRP (ABCG2)[7],[8] . Efflux back into the gut lumen will augment exposure to gut wall enzymes following any reabsorption. These transporters are also responsible for the efflux drugs from tumours and their up-regulation leads to resistance to therapy.Potential solutions to low oral bioavailability
A number of strategies are used to address the problem of poor oral bioavailability, including the development of pro-drugs, the use of deliberate drug–drug interactions involving inhibition of enzymes or efflux transporters, and formulation in sophisticated carrier systems. While these approaches continue to be investigated, formal regulatory approval lags significantly behind innovation.Pro-drugs
Pro-drugs can improve oral bioavailability by increasing the aqueous solubility or chemical stability of the active drug, or by protecting it from pre-systemic metabolism[7] . The phosphate salt of etoposide and the mesylate of imatinib increase solubility and enhance oral bioavailability significantly. While MTIC (3-methyl-(triazen-1-yl) imidazole-4-carboxamide), a DNA alkylating agent, is highly unstable in gastric fluid, the pro-drug temozolomide is stable at low pH and breaks down rapidly to MTIC by a non-enzymatic chemical reaction at physiological pH. Doxifluridine, capecitabine and tegafur are precursors of 5FU, which are not cleavable by DPD but utilise other enzymes on first-pass through the liver to convert them into the active drug. Capecitabine has been shown to be as effective as the ‘Mayo Clinic IV regimen’ for 5FU[1] .Co-administration with inhibitors of metabolism or efflux transport
The addition of ritonavir (a potent inhibitor of CYP3A) to paclitaxel and docetaxel significantly increases their oral bioavailability while, similarly, the combination of gimeracil, uracil or eniluracil (inhibitors of DPD) with 5FU enhances its systemic exposure[7] . However, eniluracil has proved to be disappointing in a clinical trial[1] . Cyclosporine and elacridar are potent inhibitors of P-glycoprotein and their combination with paclitaxel or topotecan is accompanied by significant gain in the systemic exposure of these agents after oral administration[7] . While the production of a deliberate drug–drug interaction is effective in raising oral bioavailability, it carries the risk of creating unwanted interactions with other drug or nutrient substrates of the affected enzyme or transporter. By knocking out P-glycoprotein at the blood–brain barrier, co-administration of an inhibitor of this transporter could enhance access of the victim drug to a brain tumour. Although, equally, it may increase the likelihood of central nervous system side effects from the agents involved.Formulation in carrier systems
Current research on carrier systems, especially those involving nanotechnology, is flourishing. The objective, with respect to enhancing oral bioavailability, is to improve absorption while getting ‘under the radar’ of exposure to first-pass enzymes and efflux transporters. In doing this, a number of absorption mechanisms as alternatives to transcellular passive diffusion are exploited, including the opening of tight intercellular junctions, endocytosis and pinocytosis, lipid absorption and M-cell uptake[7],[14] (see Figure 5). Notably, some of these mechanism’s direct delivery via the lymphatic system rather than straight into the blood circulation, circumventing significant first-pass metabolism. 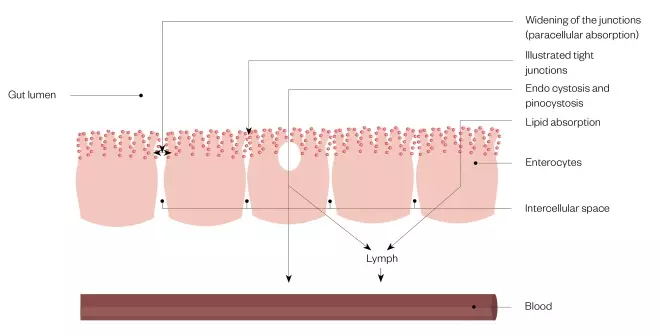
Figure 5: Absorption mechanisms exploited by drug formulations designed to enhance bioavailability
As an alternative to transcellular diffusion across the enterocyte into the blood, access to systemic exposure may be gained by widening of the tight intercellular junctions between the enterocytes to allow enhanced paracellular absorption, endo- or pino-cytosis or by exploitation of absorption pathways for lipids. The latter routes deliver drug into the lymph.
Figure 6: Formulation strategies for the oral delivery of anticancer drugs
Source: Modified with permission from J Contr Rel [14]