Abstract
Objectives
To determine whether or not inpatients newly started on warfarin at Glan Clwyd Hospital, Denbighshire, had been initiated according to audit standards based on local anticoagulation guidance.
Methods
Audit standards based on local anticoagulation guidance were developed. All medical and surgical patients starting warfarin treatment were prospectively identified. Compliance with the audit standards was audited retrospectively via the patients’ medical notes. The data captured were: indication for warfarin; baseline international normalised ratio (INR) results; and adherence to local guidance relating to frequency of INR testing and dosing.
Results
122 patients were included in the audit, with a mean age of 74 years. The indication for warfarin was stated for 96% of the patients. Of the group under 70 years of age and with a baseline INR <1.4, 10 out of 27 (37%) complied with the audit standards and the proportion of patients with a therapeutic INR on discharge was 90% in the group that complied and 87% in the group that did not. Of the patients 370 years of age or with an INR 31.4, only 33 out 95 (35%) were initiated according to the audit standards and a therapeutic INR was achieved on discharge in 68% of the group that complied and 70% in the group that did not.
Conclusion
This audit shows that there is considerable room for improvement in correctly following the anticoagulant guidelines for initiating warfarin therapy.
Warfarin is the most frequently prescribed anticoagulant in the UK and is indicated for stroke prophylaxis in patients with atrial fibrillation (AF), treatment of thromboembolism, use in certain cardiac diseases, and for patients with mechanical heart valves.1 Warfarin use in the elderly has increased dramatically in recent years due to evidence demonstrating reduction of ischaemic stroke in AF.2–4
At Glan Clwyd Hospital, Denbighshire, the junior medical staff generally undertake the prescribing of warfarin for acute inpatients, as is common across the UK. Following discharge from hospital, subsequent monitoring of international normalised ratio (INR) and warfarin dose adjustment is often undertaken by a patient’s GP. The British National Formulary recommends that a baseline INR should be recorded before warfarin is started. It also recommends starting elderly patients at a lower dose.5 An audit carried out at Glan Clywd Hospital in 2007 showed that 13 out of 33 patients (40%) had a baseline INR 31.4 before starting warfarin. There is no published guidance on how to initiate warfarin in patients who have elevated baseline INR.
The “Safer patients initiative” in 2005 highlighted the importance of developing local guidance on the prescribing of warfarin.6 Following recommendations from the National Patient Safety Agency, local anticoagulation initiation guidance (ie, for days 1–4 of treatment) was updated to take into account both patient age and baseline INR (see Figure 1).
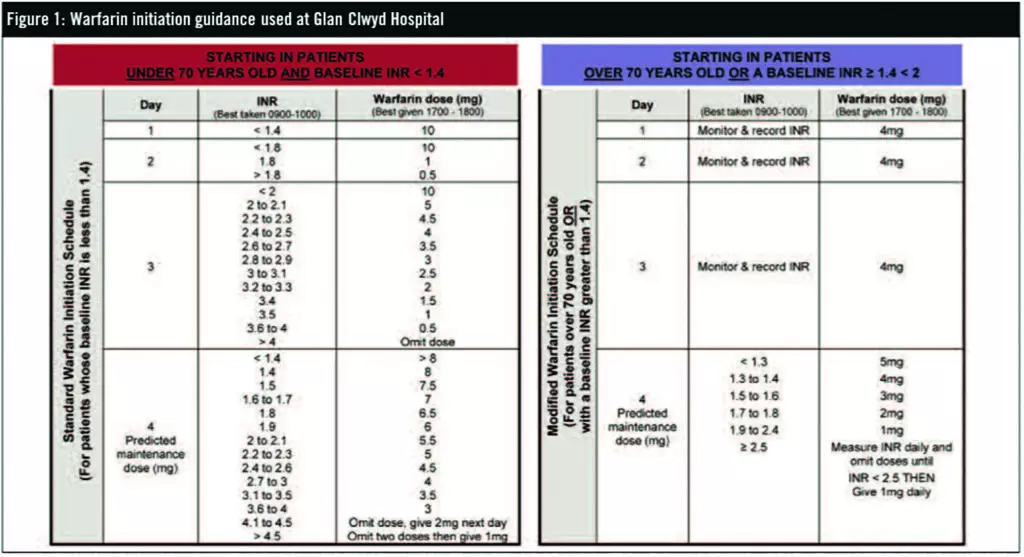
Younger patients (<70 years of age) with a baseline INR <1.4 receive dosing according to the Fennerty regimen, which requires daily INR monitoring for four consecutive days; the warfarin dose for each day is selected based on the INR result.7 Patients with a baseline INR 31.4 or elderly patients (370 years of age) receive the regimen recommended by Siguret and colleagues.8 It is important to note that Siguret and colleagues only studied elderly patients with a baseline INR <1.3. However, it was agreed locally also to adopt this initiation protocol for patients with a baseline INR 31.4. With the latter regimen, the dose is fixed at 4mg daily for three consecutive days (ie, days 1–3) then on day 4 the patient’s INR is measured and warfarin dose selected accordingly. When designing the guidance it was agreed locally that INR would be monitored daily for this group of patients as well, even though it would not affect the dose for the first three days (and therefore was not strictly necessary).
Implementing this updated guidance was supported by providing education to junior medical staff by pharmacists on warfarin prescribing which was repeated to new intakes of junior staff.
The aim of this audit was to identify whether or not inpatients who were newly started on warfarin had been initiated according to the audit standards below.
Method
Audit standards were drawn from the anticoagulation guidance and were as follows:
- All patients should have their target INR range and indication for warfarin documented
- All patients <70 years of age and with a baseline INR <1.4 should have daily INR monitored and correct dosage selected according to the guidance from days 1 to 4
- All patients 370 years of age or with a baseline INR 31.4 should have daily dosage according to guidance from days 1 to 4
- All patients aged 370 years of age or with a baseline INR 31.4 should have their INR checked on day 4 and dose adjusted accordingly (although the guidance stipulates the need to monitor INR daily, this does not affect the dose of warfarin, which should remain fixed at 4mg daily for three days; INR monitoring on days 1–3 was therefore not included in the audit standards)
A data capture form was designed to record all the relevant information required based on the audit standards. The audit was carried out for five months, from February to June 2008. All medical and surgical patients newly started on warfarin were identified prospectively by pharmacy staff. Medical records were then reviewed retrospectively and therefore ethics approval was not required. All data were collected by the auditor (RO). Patients discharged before day 4 were excluded.
Results
A total of 134 patients were initiated on warfarin treatment but 12 were discharged before day 4 so were excluded. The age range of the 122 patients included in the audit was 36 to 101 years with a mean age of 74 years. Patients over 70 years of age accounted for 78% of the group (95 patients) and 28% of eligible patients had a baseline INR 31.4 with liver enzymes within the normal range (34 patients). The main indications for warfarin were AF (55%) and thromboembolism (39%). See Box 1 for a summary of the results.
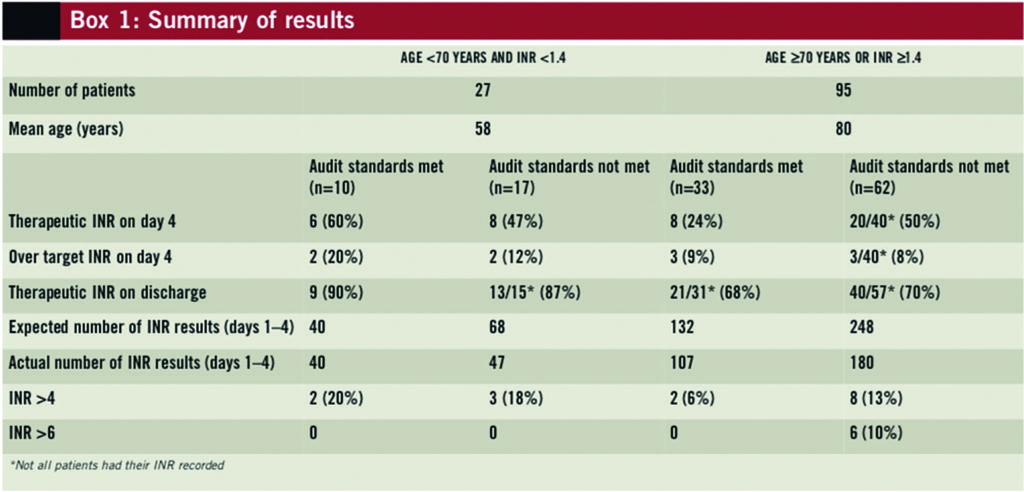
In the group of patients <70 years of age with an INR <1.4, 10 out of 27 (37%) had daily INR monitoring and appropriate doses according to local guidance for four consecutive days. Therefore, 17 patients were not initiated according to the audit standards — either because their INR was not measured daily (only 47 out the possible 68 INR results were recorded) or because the doses prescribed were not in keeping with the guidance. Nevertheless, the number of patients achieving therapeutic INR was similar in the group that followed the guidance (90%) and the group that did not (87%). The frequency of over-anticoagulation was similar in the groups (20% versus 18%). See Box 2 for a summary of compliance with the audit standards.
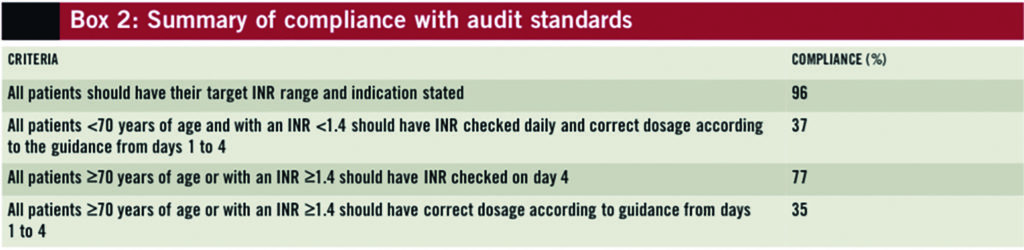
In the group containing elderly patients and patients with a baseline INR 31.4, dosing according to local guidance was given to 33 out 95 patients (35%). A therapeutic INR was achieved on discharge in 68% (21/31) of the group in which the guidance was followed and 70% (40/57) of the group in which the guidance was not followed. It is notable that in the group where the guidance was not followed an INR >6 occurred in 10% of patients (n=6).
Discussion
The group of patients studied was, largely, an elderly population (78% of patients starting warfarin treatment were over the age of 70 years and their mean age was 80 years), which is in line with the demographics of central-north Wales. This investigation, along with a previous audit, showed that a substantial number of acutely ill patients had a baseline INR 31.4 at the time of starting warfarin. These patients did not have any obvious liver disease. This high incidence of elevated baseline INR values has not been previously reported and merits further investigation.
The anticoagulation guidance was developed to reflect our population and local observations because the most readily available reference source, the BNF, gives no specific guidance other than stating that a lower dose of warfarin should be prescribed in these circumstances.
Despite the guidance, only 43 out of 122 patients (35%) had their INR monitored and warfarin dosed according to local guidance from days 1 to 4. This result is not dissimilar to that of other audits performed in UK hospitals, which have shown that recommended regimens were followed correctly for 27% of patients (11/41)9 and 39% of patients (16/41).10
Surprisingly, a therapeutic INR was achieved in a similar proportion of patients at discharge irrespective of whether or not guidance was followed (around 90% in the younger group; around 70% in the older group). This may be explained by the small size of the entire study population, which was subsequently divided into younger and elderly groups.
With respect to the frequency of INR monitoring, the guidance states that INR should be monitored daily in the group containing elderly patients and those with a higher baseline INR. Despite this, there is probably no need to tests these patients’ INRs for the first three days because the guidance recommends a fixed dose of 4mg daily. Therefore, only two INR results are required (baseline and day 4) and the audit standards reflect this. We counted the number of INR results in this group of patients. If INR tests were conducted at baseline and on day 4, we would expect 190 INR results for 95 patients in this group. However, 380 INR results were recorded, implying that 50% of the tests were potentially unnecessary. This matter will need to be addressed at the next revision of the anticoagulant guidance.
The average length of hospital stay from warfarin initiation to discharge was 6.9 days. Siguret and colleagues8 found that the mean time needed to achieve a therapeutic INR was 6.7 days and that the predicted dose on day 4 was the actual maintenance dose in 72% of the patients. In the younger group 60% were in the therapeutic range on day 4 and 90% on discharge. This latter finding is comparable to Fennerty and colleagues’ findings.7
No serious adverse events were reported in this audit; however, 15 of the 122 patients (12%) had at least one INR result >4. In the younger group, the number of patients with an INR >4 was similar in those for whom the audit standards were met and those for whom they were not (20% versus 18%, respectively). For the older patient group, 6% of patients in whom the audit standards were met had at least one INR result >4, compared with 13% in those for whom the audit standards were not met. The age range of the elderly cohort not treated according to guidance was 75 to 101 years with a mean age of 85 years. This is of concern because incidence of intracranial haemorrhage due to warfarin increases substantially in patients over the age of 80 years with an INR >4.11,12
Junior medical staff received education on warfarin prescribing but its effectiveness was not formally evaluated in this audit. There is evidence to show that providing feedback to staff can lead to some improvement in prescribing13 but education and feedback requires formal evaluation with respect to warfarin prescribing. In order to improve inpatient anticoagulation, further studies need to be undertaken to address issues around educating the junior medical staff about warfarin prescribing (eg, whether or not undertaking the BMJ learning module14 before beginning their ward duties leads to improvement in subsequent prescribing).
Recently, the British Pharmacological Society has recommended that junior medical staff follow 10 principles to improve safe and effective use of medicines.15 This message has to be promoted to all staff involved in prescribing and one means of delivering this could be by having a clinical pharmacist teacher-practitioner involved in tutoring medical staff.
An alternative to junior medical staff prescribing warfarin would be for other healthcare professionals to undertake its management. Several studies support this concept.16–18
Conclusion
Local anticoagulation guidance was updated to reflect both the local elderly population and NPSA recommendations for patients starting warfarin treatment. This guidance was followed in only a third of the patients newly started on warfarin treatment. Irrespective of guidance, therapeutic INR on discharge was achieved in 90% of the younger patient group and in 70% in the elderly group. However, some patients had elevated INR values possibly because of poor compliance with the guidance.
Based on the findings of this audit, this anticoagulant guidance should be revised, in terms of the number of INR tests required, and then the updated guidance reaudited in a larger group of patients.
About the authors
Uttamlal Chouhan is principal pharmacist for clinical services and Ranj Omar was, at the time of writing, pharmacist, both in Central Area of North Wales NHS Trust.
Email: uttam.chouhan@wales.nhs.uk
References
- Baglin TP, Keeling DM, Watson HG, et al. Guidelines on oral anticoagulation (warfarin): third edition. British Journal of Haematology 2005;132:277–85.
- Hart RG, Benavente O, McBride R, et al. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Annals of Internal Medicine 1999;131:492–501.
- Segal JB, McNamara RL, Miller MR, et al. Prevention of thromboembolism in atrial fibrillation. A meta-analysis of trials of anticoagulants and antiplatelet drugs. Journal of General Internal Medicine 2000;15:56–67.
- Aguilar MI, Hart R. Oral anticoagulants for preventing stroke in patients with non- valvular atrial fibrillation and no previous history of stroke or transient ischemic attacks. Cochrane Database Systemic Reviews 2005; issue 3.
- British National Formulary. Chapter 2.8.2: Oral anticoagulants. In: British National Formulary 57th Edition. London: BMJ Group and Pharmaceutical Press; 2009: pp127–9.
- Baglin TP, Cousins D, Keeling DM, et al. Safety indicators for inpatient and outpatient oral anticoagulant care: Recommendations from the British Committee for standards inHaematology and the National Patient Safety Agency. British Journal of Haematology2007;136:26–9.
- Fennerty A, Dolben J, Thomas P, et al. Flexible induction dose regimen for warfarinand prediction of maintenance dose. BMJ 1984;288:1268–70.
- Siguret V, Gouin I, Debray M, et al. Initiation of warfarin therapy in elderly medical inpatients: a safe and accurate regimen. American Journal of Medicine 2005;118:137–42.
- Moody J, Coleman J. Adherence to the patient safety agency guidelines: actions thatcan make anticoagulation therapy safer. 2007 Pharmacy department, Oxford Radcliffe Hospital. 5th joint national conference of the Guild of Healthcare Pharmacists and the United Kingdom Clinical Pharmacy Association. Leicester. 15–17 May 2009.
- Purcell S, Power B, Caldwell NA, et al. Audit of safety indicators for anticoagulation therapy. Pharmacy department, Wirral University Teaching Hospital NHS Foundation Trust. 5th joint national conference of the Guild of Healthcare Pharmacists and the United Kingdom Clinical Pharmacy Association. Leicester. 15–17 May 2009.
- Fang MC, Chang Y, Hylek EM, et al. Advanced age, anticoagulation intensity and risk for intracranial hemorrhage among patients taking warfarin for atrial fibrillation. Annals of Internal Medicine 2004;141:745–52.
- Stephan D, Fihn MD, Catherine M, et al. The risk for and severity of bleeding complications in elderly patients treated with warfarin. Annals of Internal Medicine 1996;124:970–9.
- Ostini R, Hegney D, Jackson C, et al. Systematic review of interventions to improve prescribing. Annals of Pharmacotherapy 2009;43:502–13.
- Fitzmaurice D, Cousins D, Clark C. Interactive case history starting patients on anticoagulants: how to do it. BMJ Learning. http://learning.bmj.com/learning/search- result.html?moduleId=5004325 (accessed 9 July 2010).
- Titmarsh S. Safer prescribing through education, IT and better systems. Prescriber 2010;21:34–8.
- Ellis RF, Stephens MA, Sharp GB. Evaluation of a pharmacy-managed warfarin- monitoring service to coordinate inpatient and outpatient therapy. American Journal of Hospital Pharmacy 1992;49:387–94.
- Foss MT, Schoch PH, Sintek CD. Efficient operation of a high-volume anticoagulation clinic. American Journal of Health-System Pharmacy 1999;56:443–9.
- Burns N. Evaluation of warfarin dosing by pharmacists for elderly medical in-patients. Pharmacy World and Science 2004;26:232–7.


