Introduction
Pharmacy services — traditionally conceptualised as commodity-based as in the dispensing of prescribed medicines — are increasingly oriented towards service provision, as illustrated by the first advanced service (medicines use review) and, most recently, the new medicine service. This shift in orientation is also reflected in recent NHS White Papers[1],[2]
announcing the creation of a new Public Health Service, and recognising community pharmacy teams are a “valuable and trusted public health resource”, “with millions of contacts with the public every day” and pharmacy will be enhanced and used “more effectively” in the future. Pharmacy therefore is seen as having an important and expanding role in supporting better health.
However, each additional service increases demand for the pharmacists’ time and places pressure on them to optimise the skill mix of the pharmacy team to provide services where a pharmacist’s input is not always necessary, as with public health and health promotion initiatives.
Community pharmacies provide a growing range of public health services producing positive public health outcomes, with an evidence base focused on smoking cessation, diabetes, emergency contraception provision, flu immunisation and drug misuse.[3]
Further evidence[4]
on the role of pharmaceutical public health has been shown from the healthy living pharmacy (HLP) initiative instigated in Portsmouth, through which community-based local pharmacies provide access to trained health advisers who can support local people to access reliable information interventions.[5]
These HLPs promote healthy living and well-being as a core activity so the public have better access to health and well-being services including stop smoking, alcohol interventions, sexual health services and NHS health checks. Building on this initiative, additional areas across England have been selected to become HLP pathfinders, with expected benefits including the ability to demonstrate to future commissioners that engaged and motivated community pharmacy teams can deliver proactive health and well-being interventions as a core activity.
Hence across England there are currently different levels of health promotion service being offered, from the contractual framework essential service of the promotion of healthy lifestyle and signposting, to a more intense, proactive approach as adopted by the HLP model. However, there is little published work that explores the idea of pharmacy positioning and promoting itself as a “public health champion” or “pharmacy healthy living adviser” (PHLA) thereby motivating and referring patients to providers of public health services. Success in delivering a service beyond that specified in the contract role depends in part on the receptivity of community pharmacy teams to undertake this wider role. Pharmacy support or counter staff are often the first point of contact for pharmacy customers and can potentially play a vital role in alleviating time constraints on pharmacists by engaging customers in health improvement discussions and signposting on to public health services.
Making use of the 10 pharmacies that had volunteered for a member of their staff to become a PHLA, we set out to explore the broader contextual circumstances of how pharmacy counter staff view such a role and whether they have the capacity to integrate this role into their existing activities, and the impact of receiving appropriate public health training on their confidence to perform this new role.
Method
A mixed method approach was adopted that involved qualitative and quantitative elements. In order to explore the beliefs and expectations of the support staff as PHLAs two focus groups were convened. The first (in November 2010) was designed to explore support staff’s perception and receptivity to the role before its commencement and before undertaking training in delivering a public health role. The group was facilitated by an experienced researcher (GH) and the content informed by a topic guide. The researcher ensured all participants had equal opportunity to participate and to ensure against participant’s contributions being subject to the group effect, ie, that a full range of opinions and beliefs was expressed among the group rather than a common consensus emerging. A pharmacist (MS) acted as moderator and contributed to proceedings on issues pertinent to pharmaceutical service delivery.
The second focus group was convened several months later when participating staff had completed their public health training and aimed to map their experiences in assuming the role of PHLAs and to compare this with their earlier perceived expectations and beliefs.
Proceedings from both groups were audio recorded and, in accordance with best practice, extemporaneous notes were taken. Proceedings were then loosely transcribed, and together with notes, were analysed for emergent themes derived using an adapted framework approach.[6]
This analysis was validated by MS.
Quantitative data were captured during a six-week period when the PHLAs completed a diary entry for each intervention undertaken, and a customer feedback form was used to measure customers’ experience and acceptance of the advice. The data collection diary was standardised so that entries made provided detailed information about the intervention, and any public health bookings made. The customer feedback form asked the customer to endorse if the information given was “very useful”, “quite useful”, or “not useful”; if they would follow the advice given (“yes”, “maybe” or “no”) and if they would seek help from the PHLA again (“yes”, “maybe” or “no”). In addition, PHLAs were asked to score themselves using a five-point Likert-type scale (1= lowest, 5= best) on their ability and confidence in undertaking this role. This was carried out by sending a brief questionnaire (plus Freepost envelope for return) to the PHLAs both before and after the training plus intervention period.
As this is a service evaluation, ethics approval was considered unnecessary.
Results
Qualitative evaluation
Twenty participants (counter assistants and dispensing technicians) attended the first focus group. Although all participants attending the first group were invited to attend, only five PHLAs attended the follow up focus group. Analysis of both proceedings yielded four emergent themes illuminating factors impacting on the effectiveness of the PHLA role.
Theme 1: competent capacity
Participants considered they had the necessary capacity to assume the role of PHLAs and training for this role provided them with the necessary skill and competencies to deliver this role effectively. It was largely agreed among the first focus group participants that this role involved considerably more activities than serving customers, and that this extended role was welcomed as it conferred broader responsibilities. There was also recognition that the role of PHLAs now involves the need for compliance with a number of regulations and that with this came a degree of responsibility not commonly associated with sales staff. Indeed, having to operate within a regulatory framework was considered to be a strength by the participants in that it elevated their status beyond that of simply a sales activity and promoted a sense of responsibility to the public’s health.
The second focus group proceedings indicated there was a considerably greater sense of the PHLAs’ strengths in facilitating the public’s health as a consequence of their formal training. Most notably the impact of their training was to increase their levels of confidence, particularly in identifying, instigating and dealing with customers’ health related issues. Completion of the course also encouraged an increased vigilance in identifying customer potential for health promotion and associated pharmacy based support and had effectively changed the way they work. Key to a strengthened sense of vigilance was the ability, derived from their training, to begin conversations with customers considered to benefit from strategies to improving health, eg, smoking cessation, weight loss and so forth.
Theme 2: role identity
Commensurate with a sense of elevated sense of responsibility among participants was a concern for this to be recognised and enshrined in their identity as key players in promoting the public’s health. Because of this extended role there was a sense of wanting their responsibilities to be acknowledged and recognised: “… that’s why a certificate is important. You don’t get the recognition of the experiential knowledge you have.”
The experiential knowledge acquired by PHLAs regarding the trajectory of regular customers’ health status over time was considered a particularly strong element of their identity as community-based health promoters. In effect they acted as agents for health surveillance — able to monitor purchasing activities among regular customers that might indicate potential health issues, and refer patients on to the pharmacist if necessary.
The group expressed the tendency for some members of the public to request to talk only to the pharmacist. However when customers are satisfied with the PHLAs’ advice this builds public confidence and they tended to return to them for future informational needs. Assuming the role of knowledge provider also required they acknowledge the limits of their knowledge and hand over queries to the pharmacists when considered necessary. This was managed by the PHLAs by first questioning the customer in a formulaic fashion, in accordance with standard operating procedures. However PHLAs reported being skilled in teasing out pertinent information from patients. This ability among others was raised in the second focus group proceedings as distinguishing characteristics differentiating them from sales assistants, as illustrated by the practice of explaining to customers the reasons for the procedures, eg, explaining to customers why paracetamol cannot be sold in quantity.
Familiarity of the PHLAs with the public — on first name terms with some customers — was considered a considerable strength and a significant feature of their identity. Their argument for spending time with patients is supported economically: “If you don’t spend the time with that customer you won’t foster customer loyalty.” PHLAs also trade their knowledge of repeated observations of other customer’s experience to new customers.
The need for trust between pharmacist and PHLAs was equally important and the PHLAs felt the weight of responsibility to the pharmacist and customer to ensure their information, based on their existing knowledge and experience, was correct. However, having received formal training this served to strengthen PHLAs’ self belief in their health-promoting activities.
The most valuable benefit of the training was the knowledge provided. In fact, what they appreciated the most was that the course largely confirmed and affirmed their existing knowledge because they have been tested on the course content and passed, ie, have actively engaged with the course information and not simply passively read the literature: “… it stays in your mind better.” Being given the role of PHLAs also enabled them to “push through them barriers”, ie, lack of confidence, and “you get more confident each time you do it”. This in turn led to a pharmacy-wide recognition of their role as PHLAs as “other staff begin to rely on you and ask you things” and they are recognised by their pharmacy colleagues as the person who deals with certain issues, eg, smoking cessation, because they possess the latest, up-to-date knowledge.
Theme 3: sustainable support
Sustained public support
A concern for the first group participants was a perceived need for specific training and ongoing support for particular health promotion issues. There was also a shared concern among the group that they required training in how to approach customers in order to engage them with health promotion without offending them. This was associated with a concern over their title — counter assistant — which they believed fostered the impression among the public that they did not hold any specialist knowledge. On the other hand they also considered it important to indicate to customers the limits to their knowledge — something they considered to be an assurance for the customer. A name badge identifying them to the public as qualified PHLAs with specific training and skills in signposting customers on to services, as distinct from a general counter assistant, was considered an effective response.
Sustained employer support
Chain pharmacies were perceived as potentially undermining the PHLAs because they require them to encourage customers to have their prescriptions delivered (as part of an attempt to secure market share). To some PHLAs this, somewhat perversely, dissuaded customers from visiting the pharmacy. Allied to this was the target-driven culture of the large chain pharmacies which was also perceived as a threat to PHLAs. However they (PHLAs) while acknowledging the need to meet targets were of the opinion that “their customer comes first… and you have to like the public. To make people well and to give them options you have to change their mindset and that doesn’t happen overnight.You have to put yourself in their position and you have to know that whatever you’ve done and whatever you’ve recommended is best for that person.”
One supermarket-based PHLA reported that this location potentially weakened their effectiveness in promoting health in that their location was incongruous to their role. Concern was also expressed over the likelihood of being released by their employer to undertake public health training.
Sustained organisational support
Participants also perceived an opportunity for the PCT to promote the greater integration of PHLAs into primary care and recognised the benefits of integrating with others working to the healthy living agenda, eg, sexual health services. Participants at the second focus group also raised the issue of career development as PHLAs. The opportunity to attend refresher course to sustain and develop their role was also mentioned “because things are always changing … new products always come out” and in the absence of formal continuing training were reliant on other PHLAs as a source of new information. PHLAs believe keeping their knowledge and skills up to date is vital and an opportunity to do so is key to developing their role.
Theme 4: assimilating the PHLA role in primary care
Overall PHLAs perceived systemic challenges to developing their role. Paradoxically the fact they were familiar with their clientele was also a potential barrier to their advice-giving role. The final concluding proceedings from the first focus group were summed up by one participant: “Your role [as PHLA] is to help customers and if you can’t help them, then you will find someone or something that will, and that is your role, and a simple thing like a badge can mean a lot, because they have trust in you.” Central to this sentiment was a perception that PHLAs did not perceive themselves to be part of a broader health care team. The second focus group provided an opportunity to establish the extent to which, having received training as a PHLA, this led them to have shifted perception and consider themselves members of a wider health promoting team. Although full integration appeared to be some way off, the participants considered there was some increasing awareness of their new role in health promotion, although it was considered there was an element of resistance from general practice and primary care. Perceived problems integrating with the GP surgery resulted from a sense that most surgeries do not appreciate what the pharmacy can offer. There was also a sense of “boundary encroachment” with PHLAs seemingly competing with nurses in primary care who are running health promotion clinics. However this was not necessarily a major issue and as one participant observed, there were a lot of them (PHLAs) relative to the numbers of practice nurses. An additional and somewhat unexpected challenge was that the PHLAs reported particular difficulties in proffering advice to women with small children over a concern to be perceived as passing moral judgements on the customer’s health risk behaviours.
Quantitative evaluation
Completed analysis of the diary entries indicated that the number of customers signposted to services by PHLAs varied considerably across the 10 participating pharmacies. During the six week data collection period 73 customers received an intervention (mean 7.3 per pharmacy, range 1–15), with 64 (88 per cent) of these involving a discussion and signposting to public health service providers. Overall 30 customers had bookings with service providers made for them by nine of the 10 PHLAs (see Table 1). The topics of the interventions covered all the major public health priorities, with smoking cessation accounting for 49 per cent of the interventions and 53 per cent of the bookings made.
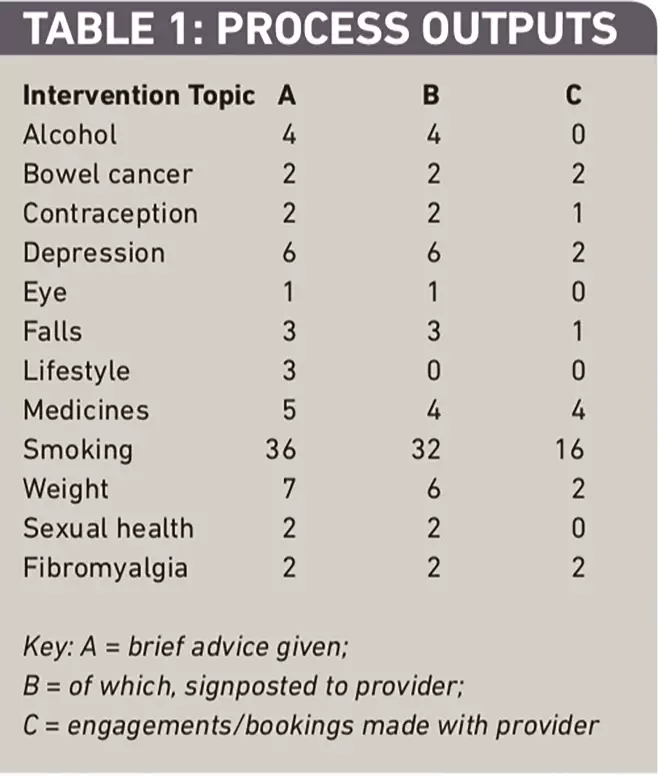
Table 1: Process outputs
Feedback questionnaires were returned by 50 customers and satisfaction with the service was largely positive, with most considering the information provided by the PHLAs to be “very useful”, and a significant number pledging to follow the advice offered (see Table 2). Nearly all of these 50 considered the experience sufficiently useful to warrant using the services of the PHLA again if required. This was especially significant given that, of the 12 topics advised on, smoking cessation accounted for half.
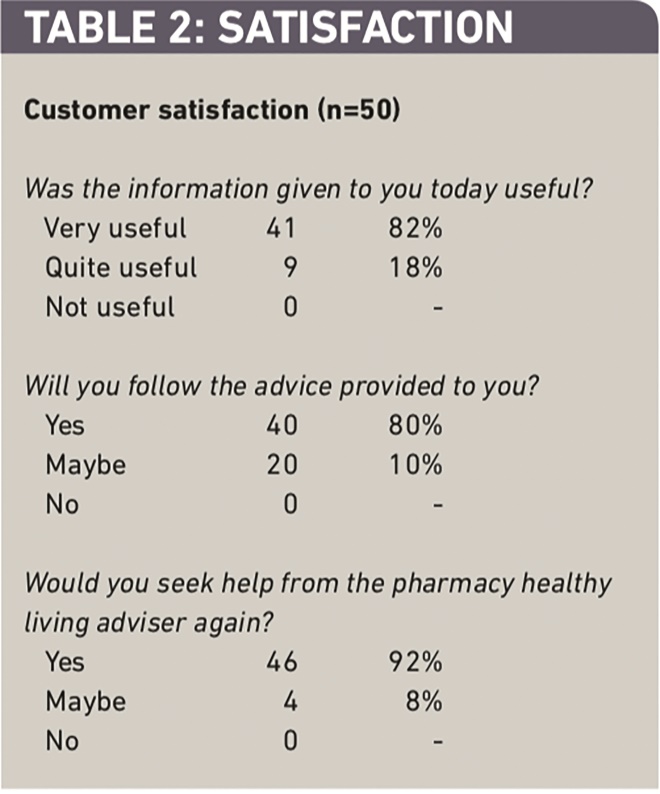
Table 2: Satisfaction
Actions undertaken to address the identified weaknesses and barriers identified from the focus groups included: delivering the Royal Society of Public Health level 2 award “Understanding health improvement” training; creating a role in the pharmacies for the PHLA; providing badges and promotional material to raise the profile of the role; creating a signposting reference source for all the local service providers; and organising a local network of PHLAs. The outcome of these actions contributed to a trend in increased confidence of the staff in their skills and knowledge (see Table 3).
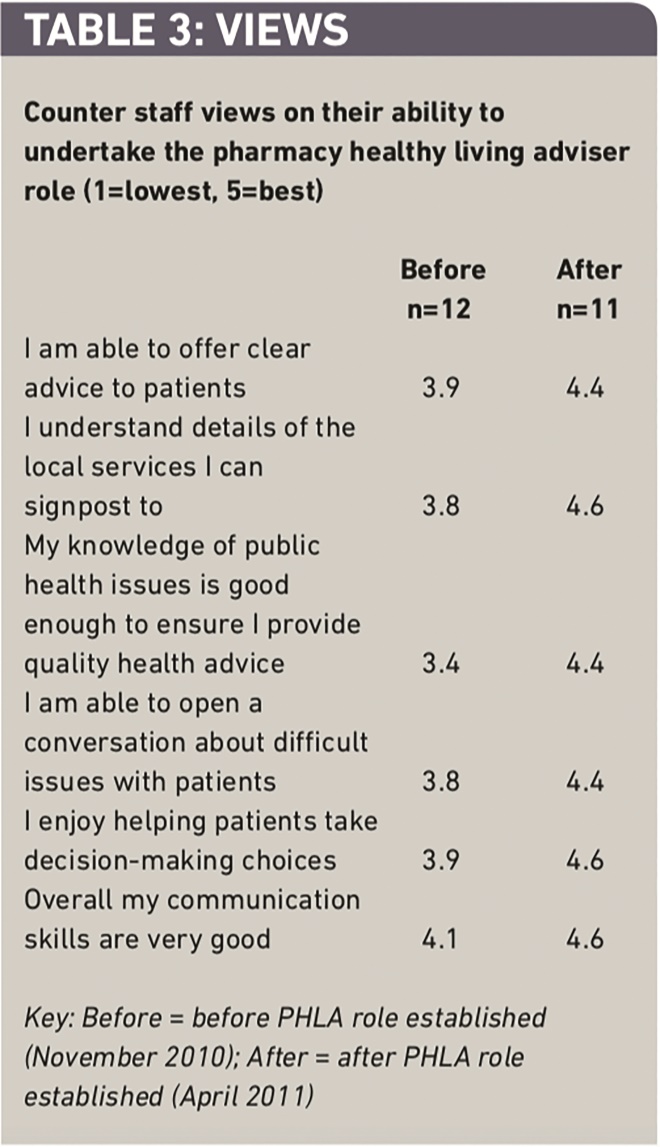
Table 3: Views
Discussion
The role of these PHLAs represents a significant acknowledgement of their potential to make a positive contribution to public health. When suitably trained to undertake this role, PHLAs appear able to contribute directly to improving the public health, and are particularly well placed as they are invariably the first point of contact for the public. Moreover they are a largely stable workforce which, for some PHLAs, leads to long established relationship with their clientèle. What this pilot indicates is that PHLAs who elect to take on an extended role possess a notable capacity and aptitude to extend their role to promote healthy living. The number of smoking cessation interventions undertaken illustrate the potential benefits to accrue from this extended role. The extent of signposting to public health service providers (88 per cent of interventions) and the high degree of customer satisfaction mirrors other research.[7]
We did observe, however, that the range of conditions on which advice was offered extends beyond the competencies covered in the public health training and this would require addressing in any more formal extension of this pilot.
The positive responses to this service from consumers (albeit a limited number of people) are in line with the findings from a review of public health in community pharmacy.[8]
These authors make the valid observation that the more public health services are offered and experienced by the general public, the more positive attitudes will become. However, others suggest that while members of the public recognised the need for many activities to improve public health, their perceptions of the involvement of community pharmacy in such activities was limited.[9],[10]
We argue that if community pharmacy is to become engaged in roles which might include the provision of targeted advice, including signposting and booking of appointments, the role of trained counter staff in owning this function is crucial. In one pilot study of screening and brief interventions for risky drinkers, the pharmacy which fully involved its counter staff was the one which provided this service to most people.[11]
We noted in our qualitative study that staff required sustained support and recognition of their extend role as PHLAs from the public, their employers, health professionals and administrative authorities. career development in a public health promotion role was seen as an issue that needed consideration, mirroring the concern that counter staff used to hold over duties now accepted as standard.[12]
There are a number of limitations of this pilot. The nature of the pilot necessarily required the intervention period to be brief limiting the quantity of intervention data recorded. relatively few participants were able to be recruited within the time frame, and those who were recruited were self-selected and typically represented support staff that were particularly enthusiastic about the initiative. The public health training programme (one day) limited the range of competencies and skills that could be covered. The second focus group was poorly attended and hence any outputs from that small group may have limited generalisability.
It appears from this small pilot that the concept of a trained PHLA role has the potential to impact on the public’s health by promoting uptake of services — in particular, smoking cessation programmes. What is not known, however, is whether these referrals lead to clients actually attending, or whether those who did attend sustained any resulting behaviour change. Given the encouraging results from this pilot, a development of this role focusing on key health issues, and the introduction of a mechanism to record the outcome of signposting to these services would be appropriate. This would generate standardised and measurable evidence of the extent of the effectiveness of the PHLA role.
Declaration of interest
The Healthy Living Project evaluation was funded by the National Prescribing Centre via the South West Strategic Health Authority.
About the authors
Geoff Harding, PhD, is honorary senior research fellow at Peninsula College of Medicine and Dentistry, Exeter. Mark Stone, MRPharmS, is project pharmacist at Devon Local Pharmaceutical Committee. Mike Wilcock, MRPharmS, is head of the prescribing support unit at Pharmacy Department, Royal Cornwall Hospitals NHS Trust, Truro.
Correspondence to: Mark Stone at Devon Local Pharmaceutical Committee, Deer Park Business Centre, Haldon Hill, Kennford, Exeter EX6 7XX (email mark@devonlpc.org)
References
[1] Department of Health. Equity and excellence: liberating the NHS. London: DoH; 2010.
[2] Department of Health. Healthy lives, healthy people: our strategy for public health in England. London: DoH; 2010.
[3] Anderson C, Blenkinsopp A, Armstrong M. The contribution of community pharmacy to improving the public’s health. London: Pharmacy Health Link; 2009.
[4] Katikireddi SV, Higgins M, Bond L, et al. How evidence based is English public health policy? BMJ 2011;343:d7310.
[5] Bowhill J, Bowhill S, Evans D, et al. An interim report on the outcomes from the Portsmouth Health Living Pharmacy initiative.
[6] Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R (editors). Analysing qualitative data. London: Routledge; 1993, pp173–94.
[7] Rodgers R, Collins S, Ghir S. An exploration of the public acceptability of signposting by community pharmacies. International Journal of Pharmacy Practice 2011;19(Suppl 2):74–75.
[8] Eades CE, Ferguson JS, O’Carrol RE. Public health in community pharmacy: A systematic review of pharmacist and consumer views. BMC Public Health 2011;11:582.
[9] Krska J, Morecroft CW. Views of the general public on the role of pharmacy in public health. Journal of Pharmaceutical Health Services Research 2010;1:33–38.
[10] Saramunee K, Krska J, Mackridge A, et al. General public’s views on community pharmacy public health services: a qualitative study. International Journal of Pharmacy Practice 2011;19(Suppl 2):78.
[11] Watson M. Community pharmacy and alcohol-misuse services: a review of policy and practice. London: Royal Pharmaceutical Society of Great Britain, 2008.
[12] Seston EM, Nicolson M, Hassell K, et al. “Not just someone stood behind the counter”: the views and experiences of medicines counter assistants. Journal of Social and Administrative Pharmacy 2001;18:122–8.


