Introduction
The three most frequently occurring types of medication error reported to the National Patient Safety Agency’s National Reporting and Learning System are wrong dose, omitted medicine and wrong medicine.[1]
Mistakes occur at all stages of prescribing, from the decision to use a medicine in the treatment of an individual to writing it correctly and legibly — including calculating or selecting the correct dose or dosage form. At the decision stage, knowledge of the patient’s history of medicines use and any previous adverse drug event must be taken into account; if it is not then a prescribing error has been made.
Strategies for reducing errors include organisational interventions such as ward pharmacy services,[2]
and process changes such as the use of information technology in the ordering of medicines.[3]
An electronic prescribing system (e-prescribing) solves problems with illegibility and minimises mistakes in transcribing and processing (preparing and dispensing the ordered medicine).[4],[5]
In addition, many hospital e-prescribing systems provide computerised decision support, with links direct from the prescribing screen to, for example, laboratory results, allergy data and prompts or alerts for interactions and duplicate medicines. However, new types of error may be introduced, for example, through careless selection from a drop-down menu of the wrong drug or the wrong dose.[6],[7]
Having recently implemented inpatient e-prescribing and administration recording, we were interested in comparing features of this system with traditional handwritten prescriptions (HWPs) on paper drug charts. We report here on the findings from pharmacists’ intervention data, where prescribing errors were judged for their potential for patient harm had they not been intercepted.
Methods
Ethical approval was obtained from the local research ethics committee.
Selection criteria/participants
The study was carried out in a 480-bed teaching hospital undergoing full implementation of e-prescribing. All outpatient and take-home prescriptions for discharged inpatients were already computer-generated using an existing system. Over a period of several months all wards were being changed to e-prescribing from traditional handwritten drug charts.
The e-prescribing system includes the hospital formulary as a menu for drop-down selection and a separate list of non-formulary medicines (both of which have inbuilt decision support). The system also features link buttons for accessing patient demographics, laboratory data, radiology, communication notes from other users and the British National Formulary, the BNF for Children and all hospital procedures, policies and guidelines via the intranet. At all times during prescribing, the patient’s allergies and weight are on the screen (see Figure 1).
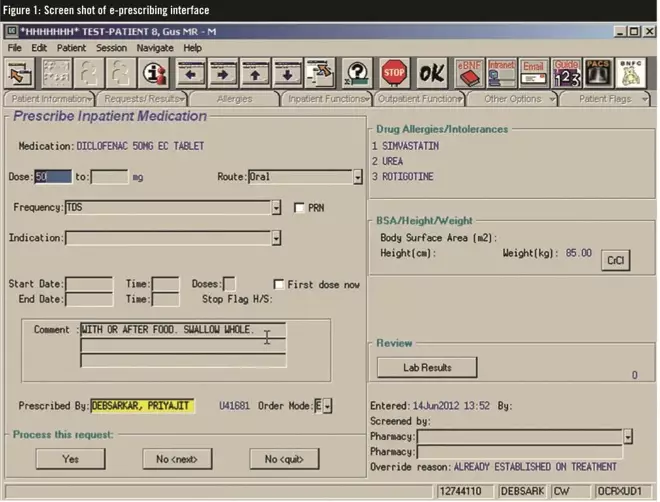
Figure 1: Screen shot of e-prescribing interface
Alerts “pop up” as a clinician enters or checks medicines to which the patient is known to be allergic, that may interact with other prescribed medicines or are duplicates (see Figure 2).
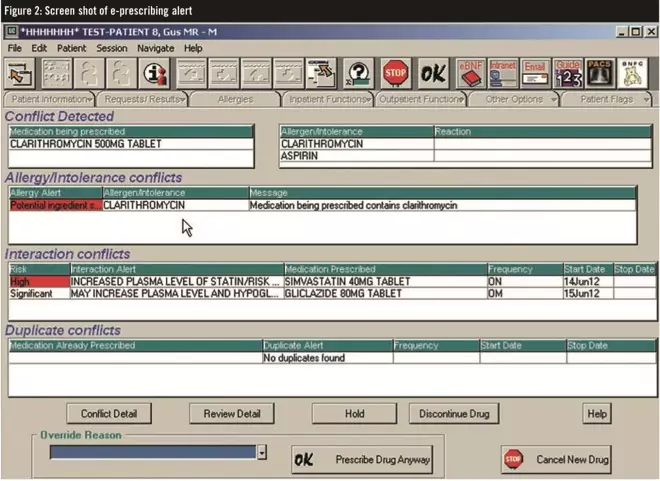
Figure 2: Screen shot of e-prescribing alert
These alerts have to be “answered” from a menu on screen before the prescription entry can be made.
We conducted a before-and-after study on two adult surgical wards — the first to move to inpatient electronic prescribing. The timetable for implementation was set several months before the overnight changeover on these wards from HWPs. Each ward has 28 beds for patients admitted for surgery requiring at least an overnight stay. All prescriptions were checked and, where necessary, the prescriber contacted for clarification or alteration as per the usual ward pharmacy service.
Data collection
Pharmacists recorded all consecutive interventions (defined as any communication between pharmacist and clinician, verbal or written, with the intention of influencing prescribing) for four months immediately before e-prescribing and then on the same wards after full implementation. The periods of study were of the same four-month duration before and after implementation. There were no other changes made to the ward that might be expected to influence prescribing. A settling-in period of three months was allowed between implementation and the “after” phase of the study.
Interventions were coded by type. Certain cases were not considered prescribing errors for the purposes of this study, for example, using brand name or non-formulary prescribing. This is in line with previously published data on errors.[8]
Errors intercepted were categorised as omissions, wrong drug, wrong dose, wrong route or other incorrect instruction (after Dean et al).[9]
We included a further category: unauthorised prescriber.
Where there was an unintentional omission of a regular medicine which should have been continued, we noted if this occurred at admission to hospital (where the drug history would have had to have been checked).
Prescribing errors involving wrong drug included prescriptions for a medicine: to which the patient has a documented allergy or intolerance (but not where it develops later); that interacts with other prescribed medicines; or is an inadvertent duplication of same or similar medicines.
We recruited three senior pharmacists and three consultant doctors to assess the severity of the prescribing errors, as recorded and described by the intervening pharmacists. They scored all the error cases individually, in terms of their potential for harm, on a visual analogue scale from 0 to 10 (where 0 represented an error with no potential effect on the patient and 10 an incident that would be likely to result in death). The mean score for each intervention was the harm score. This is a validated scoring system[10]
used in previous studies of medication errors.[11],[12]
Severity categories were assigned according to the mean harm score:
- Low — harm score 0–3
- Moderate — harm score 4–7
- Serious — harm score 8–10
All coded interventions were entered into an SPSS database for analysis, comparing those collated before with those after implementation of inpatient e-prescribing. A P-value of less than 0.05 was set as the significance level.
Results
Pharmacists intervened on 251 HWPs and 248 electronic prescriptions. From these interventions, as defined in the method, we found and assessed 183 and 178 prescribing errors, respectively.
The most common type of error pharmacists identified was omission (regular medicine unintentionally missed from a rewritten or transcribed prescription); this accounted for 41.5% of HWP errors and 37% of e-prescription errors. Such errors occurred particularly at admission, with the admitting doctor inadvertently failing to prescribe regular medicines from the drug history (43 of the 72 HWP omissions and 28 of the 66 e-prescribing omissions).
The harm score average before e-prescribing was 2.46 and after was 2.18 (t-test for equality of means, 95% confidence interval 0.07–0.49; P=0.009), representing a reduction in severity of 11%. The stages of the prescribing process where each error was intercepted are shown in Box 1, along with the harm category assigned.
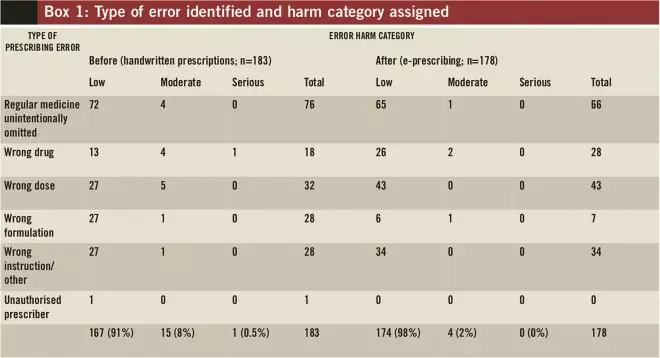
Box 1: Type of error identified and harm category assigned
We judged as having serious potential for harm one error intercepted from an HWP and none from e-prescribing. The HWP with a serious potential for harm was for a patient known to be allergic to penicillin who was prescribed co-amoxiclav as a new discharge medicine.
Fifteen (8%) of the HWP errors, and four (2%) of the e-prescribing errors, were judged to have potential for moderate harm. Of the four e-prescribing errors, two involved the prescriber over-riding inbuilt alerts:
- Co-codamol prescribed together with paracetamol
- Morphine prescribed for an inpatient who was allergic to the drug
The two other moderate e-prescribing errors are considered likely to occur with either system:
- Pharmacist asked doctor to review prescribing of diclofenac in view of deteriorating kidney function (as indicated by assessment of creatinine clearance)
- Diazepam 10mg/2ml emulsion injection prescribed via intramuscular route (wrong route for this formulation)
In both phases of the study, most errors were scored as low harm. When those that occurred during e-prescribing were examined we found that, on more than one occasion, a lack of familiarity with the computerised entry system may have contributed to these errors. For example:
- Error in selecting aspirin from menu as enteric-coated instead of the intended dispersible formulation
- Potassium 20mmol in glucose 5%, ordered as glucose with additive detailed in the comments section (the prescriber should have selected a pre-mixed bag from the system)
- Prescription for cefuroxime for surgical prophylaxis prescribed as 750–1,500mg three times a day (eight hourly) for one day instead of three stat doses sequentially (1,500mg, 750mg and 750mg) which can be entered as an order set
Discussion
We have shown benefits of e-prescribing over HWPs in reducing the severity of potential harm to patients from prescribing errors.
There is some difficulty comparing our results with those from other researchers because of the differences in systems used, especially outside the UK. Many researchers refer to “computerised physician order entry systems” (CPOEs) which may or may not have a clinical decision support system inbuilt. This is an inherent limitation of our study.
In addition, our patient population was limited to surgical wards, where there is relatively less prescribing outside protocol, for example, for antibiotic prophylaxis. We did include particular analysis of medicines stopped or continued from the patients’ drug histories at admission; some studies may not have counted these as errors.
Our denominator was not the number of prescriptions seen but a period equal in duration before and after implementation of e-prescribing. Our rates of errors are therefore over time and can only usefully be compared before and after at our hospital rather than with any degree of certainty against rates elsewhere.
In another UK study similar to ours, the prescribing error rates on a 36-bed orthopaedic ward were significantly reduced after introducing e-prescribing (from 7.4% to 4.7%).[13]
Looking at the incidence of all medication errors at a hospital in Belgium where paper and e-prescribing coexist, a lower incidence (3.4%) was measured in e-prescribing compared with paper-based prescriptions (27%).[14]
Dean and colleagues found the frequency of prescribing errors fell from 3.8% before to 2.0% after the introduction of their “closed loop e-prescribing and dispensing system”, although no difference was found in harm scores before and after.[15]
Their average harm score means were higher at 4.2 and 4.6, compared with our study findings of 2.5 and 2.2. Differences in data collection methods and the e-prescribing systems used may account for this.
Another UK study conducted in a renal unit, involving nearly 90,000 medication orders placed electronically, showed that 58% were “disallowed” by the computer system because they were for allergies and serious interactions that might otherwise have resulted in an adverse event.[16]
Alerts have also been shown to reduce likelihood of dosing errors for patients with renal insufficiency[17]
and in prescribing for thromboprophylaxis by our team, previously reported.[18]
In our study, many of the HWP errors were due to medicines prescribed for patients with known allergy and judged as having potential for moderate harm. The one scored as serious was an allergy conflict. It may be that these errors are reduced because prescribers are better alerted to allergies when using e-prescribing compared with paper prescriptions.
In a prospective cohort study conducted in a UK intensive care unit over a 70-week period, prescribing errors were significantly fewer for e-prescribing than for handwritten orders (4.8% and 6.9%, respectively; P<0.04).[7]
However, there were three e-prescribing errors that, had the medicines been administered, would have led to permanent harm or death. Intensive care was not included in our study so direct comparisons cannot be made but, examining the details, we believe that these serious errors are unlikely to occur with our local e-prescribing system because of the alerts and inbuilt decision support.
Many of our prescribing errors were omissions found by pharmacists when undertaking medicines reconciliation soon after patient admission; overall these accounted for nearly 20% of all intercepted errors. This is a common finding in keeping with those from other studies and gives support to pharmacists continued vigilance in the medicines reconciliation process. There was a reduction in omission errors with e-prescribing; greater clarity of the documentation of drug histories on the computer screen compared with HWPs may be a factor.
In one published study, 61% of all patients were found to have one or more of their regular medicines not entered on the e-prescribing system.[19]
A later study showed that omissions from drug histories accounted for 62% of all medication errors at a UK hospital’s acute medical assessment unit.[20]
The authors judged 20% of these to be moderate errors, and 0.4% major errors. No omissions in our study were judged as serious.
An investigation into the causes of prescribing errors in a London teaching hospital showed that a lapse in attention or failure to apply relevant “rules” (eg, how to reduce a dose in renal failure) were common underlying causes.[21]
Having electronic links to such rules might be expected to reduce errors caused by the latter.
Prescribing rules were also referred to in the EQUIP study, along with miscommunication on the part of a third party, and deficiency of (often complex) knowledge.[22]
An editorial in The Lancet commenting on the EQUIP study findings suggested that the variety of UK hospital HWP charts contribute to error rates and recommended standardisation as a method to minimise errors.[23]
There was, however, no reference to electronic prescription forms.
When an error in prescribing (including an omission) is identified by pharmacists, nurses or other healthcare colleagues, the prescriber is contacted and, in some cases, the details and outcome of the intervention are documented. These documented data do not represent total numbers of prescribing errors — some will, inevitably, be missed by everyone and many will not be recorded. Nor is the total number of medication errors picked up, since only the prescribing, and to a certain extent transcribing and monitoring, is assessed but not mistakes made in the other areas. Delays in prescribing might be expected with a new system. This type of prescribing “error” was not adequately assessed using our study methodology. However, intervention monitoring, in addition to providing a sample for investigating prescribing errors as described here, can guide and influence training and inform organisations of near misses and ways in which risk to patients can be minimised.
Conclusions
We have shown that a fully computerised system for prescribing inpatient medicines decreases the potential for harm to patients. Although errors are still made and intercepted by pharmacists, their severity is reduced significantly. Our locally adopted electronic system contributes to the goal of error-free prescribing, reducing potential for harm compared with traditional handwritten methods. However, like other researchers (despite comparisons being limited by differences in e-prescribing systems) we found errors are not eliminated at every stage of the prescribing process and different errors, albeit with less potential for harm, are introduced. During the study period, and after the introduction of electronic prescribing, locally there were no errors identified that had potential for serious harm.
Acknowledgements
Thanks to Nick Cooley, pharmacist, Mark Bower, consultant medical oncologist, Deirdre Richardson, pharmacist, and Chris Chung, pharmacist, all at Chelsea and Westminster Hospital NHS Foundation Trust. Thanks also to Neil McCall Peat, pharmacist and data collation and electronic prescribing specialist, formerly at Chelsea and Westminster Hospital NHS Foundation Trust.
Declaration of interests
The authors declare that they have no competing interests.
About the authors
Vanessa Marvin is deputy chief pharmacist for clinical services, India Hardy was, at the time of writing, lead pharmacist for electronic prescribing, Richard Morgan is a consultant physician, Deirdre Linnard is head of pharmacy and David Asboe is a consultant physician, all at Chelsea and Westminster Hospital NHS Foundation Trust.
Email: vanessa.marvin@chelwest.nhs.uk
References
[1] National Patient Safety Agency. Safety in doses: improving the use of medicines in the NHS. April 2007. www.nrls.npsa.nhs.uk/resources (accessed 3 April 2012).
[2] Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998;280:1311–6.
[3] Bates DW. Using information technology to reduce rates of medication errors in hospitals. BMJ 2000;320:788–91.
[4] Mekhjian HS, Kumar RR, Kuehn L, et al. Immediate benefits realized following implementation of physician order entry at an academic medical center. Journal of the American Medical Informatics Association 2002;9:529–39.
[5] Devine EB, Hansen RN, Wilson-Norton JL, et al. The impact of computerized provider order entry on medication errors in a multispecialty group practice. Journal of the American Medical Informatics Association 2010;17:78–84.
[6] Koppel R, Metlay JP, Cohen A,et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293:1197–203.
[7] Shulman R, Singer M, Goldstone J,et al. Medication errors: a prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Critical Care 2005;9:R516–21.
[8] Dean B, Barber N, Schachter M. What is a prescribing error? Quality and Safety in Health Care 2000;9:232–7.
[9] Dean B, Schachter M, Vincent C, et al. Prescribing errors in hospital inpatients: their incidence and clinical significance.Quality and Safety in Health Care 2002;11:340–4.
[10] Dean BS, Barber ND. A validated, reliable method of scoring the severity of medication errors. American Journal of Health-System Pharmacy 1999;56:57–62.
[11] Brady D, Dean-Franklin B. An evaluation of the contribution of the medical admissions pharmacist at a London teaching hospital. International Journal of Pharmacy Practice 2004;12:1–6.
[12] Barber ND, Alldred P, Raynor DK, et al. Care homes’ use of medicines study: prevalence, causes and potential harm of medication errors in care homes for older people. Quality and Safety in Health Care 2009;18:341–6.
[13] Fowlie F, Bennie M, Jardine G. Evaluation of an electronic prescribing and administration system in a British hospital. Pharmaceutical Journal 2000; 265(suppl):R16.
[14] Colpaert K, Claus B, Somers A, et al. Impact of computerized physician order entry on medication prescription errors in the intensive care unit: a controlled cross-sectional trial. Critical Care 2006;10:R21.
[15] Dean-Franklin B, O’Grady K, Donyai P, et al. The impact of a closed-loop electronic prescribing and administration system on prescribing errors, administration errors and staff time: a before and after study. Quality and Safety in Health Care 2007;16:279–84.
[16] Nightingale PG, Adu D, Richards NT, et al. Implementation of rules based computerised bedside prescribing and administration: intervention study. BMJ 2000;320:750–3.
[17] Galanter WL, Didomenico RJ, Polikaitis A. A trial of automated decision support alerts for contraindicated medications using computerized physician order entry. Journal of the American Medical Informatics Association 2005;12:269–74.
[18] Yarranton H, Marvin V, Hardy I, et al. Does electronic prescribing improve appropriate use of thromboprophylaxis for surgical inpatients? British Journal of Clinical Pharmacy 2010;2:213–17.
[19] Lau HS, Florax C, Porsius AJ, et al. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. British Journal of Clinical Pharmacology 2000;49:597–603.
[20] Rees S, Thomas P, Shetty A, et al. Drug history errors in the acute medical assessment unit quantified by use of the NPSA classification. Pharmaceutical Journal 2007;279:469–71.
[21] Dean B, Schachter M, Vincent C, et al. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002;359:1373–78.
[22] Dornan T, Ashcroft D, Heathfield H, et al. An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education. EQUIP study. www.gmc-uk.org/about/research/research_commissioned.asp (accessed 8 December 2009).
[23] Editorial (anon). How to reduce prescribing errors. Lancet 2009;374:1945.


