Introduction
Between 2000/01 and 2004/05 NHS drug expenditure in primary care nationally increased by almost 50 per cent, which prompted the NHS to explore opportunities to control drug expenditure without adversely impacting on patient care. In NHS West Midlands a range of proposals were developed for change in primary care trust prescribing activity during 2005/06, and PCT pharmaceutical advisers were subsequently tasked with delivering this change. Although in 2005/06 hospital medicines expenditure represented approximately 20 per cent of the total NHS medicines expenditure, it has been suggested that 16–20 per cent of primary care prescribing is initiated in hospital and a further 40 per cent may also be strongly influenced by hospital prescribing.[1]
As discussed in previous articles there has, hitherto, been a paucity of national data on secondary care prescribing.[2],[3],[4]
project conducted by the National Prescribing Centre in 1998 exposed the problems of collating hospital medicines use data due to the variety of hospital computer systems in use, and differences in the way medicines issues were counted.[5]
A dataset of hospitals’ medicines use is collated by IMS Health, a commercial information company that covers approximately 95 per cent of hospitals in England. We have accessed this dataset to support benchmarking of medicines use and improve medicines management performance. Furthermore we have examined whether comparator data at a strategic health authority level can be used to deliver change in hospital drug usage to support NHS West Midlands indicators for prescribing.
In a previous article[4]
we discussed the problems associated with comparing hospital medicines use, as well as discussing various indicators, arguing that expenditure and usage data alone are of little value because of differences in hospitals’ size, activity and case mix. However, we proposed that proportional use of specific medicines within a therapeutic group or defined daily doses (DDDs) divided by some measure of hospital activity were potential tools to compare different hospitals’ medicines use. This latter indicator has been validated in practice.[3]
In this paper we will show how one of these tools (proportion of medicines use within a therapeutic group) can be applied in practice. We will also show how these data can be used to bring about change in medicines use in secondary care to that are economically advantageous and that changes achieved are sustainable.
Proton pump inhibitors were chosen for this study since this therapeutic group had been identified by NHS West Midlands as an area where there could be an improvement in primary care cost effective prescribing. The components of this that were thought to be most easily supported by secondary care were simple formulation switches of lansoprazole and omeprazole tablets to capsules. At the time, the capsule formulations were 75 per cent cheaper than tablets in primary care.[6]
Method
Data on use of PPIs in hospitals across NHS West Midlands were extracted from the IMS Health dataset and used to monitor hospital prescribing activity in these target areas on a quarterly basis. Usage data were expressed as proportions of numbers of tablets and capsules for each PPI by hospital.
The NHS West Midlands secondary care pharmaceutical adviser examined data for PPI usage in secondary care in the context of NHS West Midlands primary care prescribing indicators for formulation selection of omeprazole and lansoprazole. A number of trusts were identified in the period October to December 2005 as having most opportunity for change and these were brought to the attention of and discussed with the individual hospital trust chief pharmacist as to why their use of particular formulations of PPIs was at variance to that of most trusts across the West Midlands.
In each of these cases, individual trusts had negotiated a price advantage by using the tablet formulation in preference to capsules. Once the individual trust chief pharmacists were made aware of the variance of their hospital usage relative to the rest of the West Midlands they agreed to change their procurement strategy and promote the use of the capsule formulation within their trusts. This action was designed to bring all hospitals’ use of PPIs across NHS West Midlands into line with the overall prescribing strategy in primary care for this group of drugs.
All hospital trust chief pharmacists across NHS West Midlands were made aware of primary care prescribing targets by the NHS West Midlands secondary care pharmaceutical adviser and the potential for them to be at variance with these targets as a result of local purchasing policies for this group of drugs. The chief pharmacists were then asked to take action to support NHS West Midlands primary care prescribing targets since it is suggested that hospital prescribing strongly influences primary care prescribing.[1]
The pharmaceutical adviser for secondary care continued to review prescribing data for this group of drugs and provided regular feedback to chief pharmacists in order to monitor the effect of individual action plans and maintain the momentum of this initiative.
Results
Analysis of the IMS Health dataset for PPIs in October–December 2005 demonstrated that lansoprazole tablets accounted for 42 per cent of all lansoprazole prescribing in hospitals across the West Midlands. However, in four of the 18 trusts tablets represented more than 90 per cent of all lansoprazole used. When these four trusts were excluded the average percentage usage of lansoprazole tablets in the remaining 14 trusts was 13.6 per cent (sd 6.6 per cent). After the target for switching the formulation of lansoprazole was brought to the attention of chief pharmacists, and their action plan for change was implemented, use of lansoprazole tablets in the four excluded hospitals fell to less than 17 per cent in the period April–June 2006. Furthermore, when these four hospitals were once more included in the calculations, the overall use of lansoprazole tablets across all 18 West Midlands trusts for this period fell to 15 per cent of all lansoprazole use.
Similarly in the period October– December 2005, omeprazole tablets accounted for 35 per cent of omeprazole prescribing in hospitals across the West Midlands. However in four trusts omeprazole tablets represented more than 70 per cent of all omeprazole use. When these four trusts were excluded, the average percentage usage of omeprazole tablets in the remaining 14 trusts was 7.2 per cent (sd 3.7 per cent). Again, after this was brought to the attention of the trust chief pharmacists concerned, and they had implemented their action plan for change, use of omeprazole tablets fell to less than 15 per cent in three of the excluded trusts and less than 35 per cent in the fourth by the period April–June 2006. When the four trusts were once more included in the calculations. overall use of omeprazole tablets across all 18 West Midlands trusts for this period fell to 7 per cent of all omeprazole prescribing.
Furthermore this reduction is the use of omeprazole and lansoprazole tablets was sustained in 2007 and 2008 (Table 1).
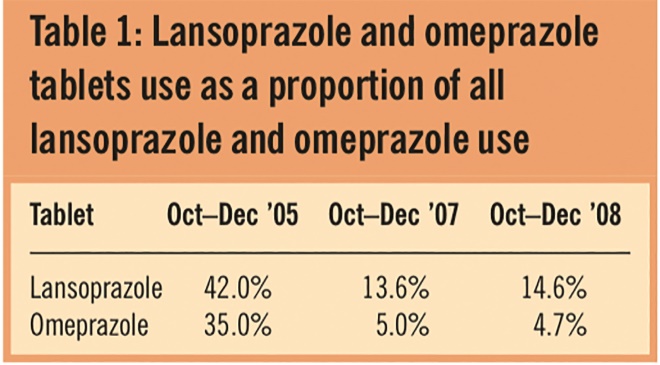
Table 1: Lansoprazole and omeprazole tablets use as a proportion of all lansoprazole and omeprazole use
Discussion
The results presented here use IMS Health hospitals’ medicines usage data expressed as a proportion within a therapeutic class. We have previously demonstrated[7]
that expressing usage data in this way compensates for variables such as hospital size and activity, which have been identified as confounding factors when using raw data.[4]
This study has demonstrated that data expressed in this way can be used to deliver a change in medicines use in hospitals, which is sustained. This in turn can impact on medicines use in primary care through ongoing prescribing activity and, as a result, support PCTs in meeting their prescribing targets. It is clear that some chief pharmacists were unaware that their usage of lansoprazole or omeprazole was at variance with use throughout the rest of the West Midlands. It is, however, surprising they had not considered the impact of their hospitals’ use of these PPIs on their PCT’s management of its drug budget. However it was pleasing to note that the “rogue” trusts were amenable and quick to respond to proposed change in order to help the PCT meet its prescribing target. The lack of secondary care comparative data also hindered pharmaceutical advisers in their host PCTs in ensuring their local provider trust was implementing economically advantageous prescribing policies. It is equally surprising that these pharmaceutical advisers had not exercised their commissioning and performance management opportunities accordingly.
Although there was an overall reduction in the use of omeprazole tablets across the West Midlands in three individual trusts use increased. (It should be noted that data on usage of omeprazole tablets includes Losec MUPS, for which there was no price advantage in secondary care.) The reason for the increased use of tablets in these three trusts is likely to be clinical decision unrelated to price.
Individual hospitals monitor medicines use closely and feed the data back to clinical specialties, but they are generally unaware of their trust’s overall prescribing patterns when these are compared with those of other hospital trusts within the SHA owing to a lack of comparative data. Furthermore, it would appear from our results that in some health economies either communication or relationships are not sufficiently robust to foster collaboration on medicines management strategies, and other mutually supportive opportunities may, therefore, also be missed.
It is interesting to note that one trust was already a low user of lansoprazole tablets (0.7 per cent), and this was worthy of further examination. On investigation it appears that the trust was offered by the manufacturer a price advantage to use lansoprazole tablets in preference to capsules. It then raised this at its area prescribing committee where the trust’s lost opportunity to make savings and the potential adverse impact on primary care expenditure was considered. The PCT agreed to compensate the hospital trust for this provided the hospital actively policed the appropriate use of lansoprazole tablets to minimise its consequent impact on primary care. The hospital appeared to be successful in this policing activity and the low usage of lansoprazole tablets was maintained throughout the study period. It is also interesting that the primary care trust concerned has the highest use of low cost PPIs in the West Midlands.[8]
Data for 2007/08 demonstrate that the change delivered was sustained. Furthermore these data on hospital use of low cost PPIs compared with primary care data suggest that secondary prescribing is more consistent with NICE clinical guidelines[9]
but whether this is influencing primary care prescribing is unclear. This issue will be explored more fully in a subsequent paper.
For a number of years the NHS has been able to compare the cost of delivering healthcare in different NHS trusts.[10]
Attention on prescribing activity appears to be continuing in proposed “Better care, better value” indicators for the NHS[11]
although, currently, this appears to be focused on primary care. This is probably because good comparative data on prescribing have existed in primary care for many years.[12]
However, as demonstrated in this article, national data on hospital prescribing do exist, and we have explored how these data can be analysed to compensate for variables such as hospital size and activity to allow meaningful comparison of hospital medicines use. Our results demonstrate how these comparative data can be used to effect change that is potentially of benefit for the whole of the West Midlands health economy. It has also exposed a lack of communication between primary and secondary care in some cases. In the current NHS environment of “Better care, better value” indicators, practice-based commissioning, integrated care pathways etc. it is more important than ever that there is robust dialogue and collaboration between medicines management services in primary and secondary care. This is something to which chief pharmacists and pharmaceutical advisers will need to give greater attention
Conclusion
This study has demonstrated that IMS hospital medicines usage data expressed as the proportional use of each medicine can be used to compare the use of medicines within a class in different hospitals. This study has also demonstrated that these comparative data can be used to facilitate change within hospitals in support of primary care prescribing objectives and that this change can be sustained. Evidence in the West Midlands is that chief pharmacists are willing to collaborate in this way to support PCTs in meeting their targets and achieve savings. Evidence also exists in one West Midlands area that primary and secondary care are able to collaborate to counteract manufacturer “loss leading” into secondary care.
About the authors
R. G. Pate, MCPP, FRPharmS, is secondary care pharmaceutical adviser at Keele University
R. W. Fitzpatrick, PhD, FRPharmS, is clinical director of pharmacy at Royal Wolverhampton Hospitals and professor of pharmacy at Wolverhampton University
P. Woodvine, BSc, is data analyst in the department of medicines management at Keele University.
In collaboration with West Midlands hospital chief pharmacists.
Correspondence to: Ron Pate, Department of Medicines Management, Keele University, Keele, Staffordshire ST5 5BG
e-mail r.pate@mema.keele.ac.uk
References
[1] National Audit Office. Prescribing costs in primary care. London: Stationery Office, 2007.
[2] Fitzpatrick RW, Pate RG. Development of an indicator to compare hospital use of sevoflurane. 42nd Mid Year Meeting of the American Society of Health System Pharmacists, Las Vegas, 2007.
[3] Fitzpatrick RW, Edwards CM. Evaluation of a tool to benchmark hospital antibiotic prescribing in the UK. Pharmacy World and Science 2008;30:73–8.
[4] Fitzpatrick RW, Pate RG. Hospital prescribing: a taste of each other’s medicine. Health Services Journal 2008;(Nov 13):28–9.
[5] Walker D. Prescribing information in secondary care — the value of a national database. Pharmaceutical Journal 2000;264:262–5.
[6] British National Formulary (52nd ed). London 2005.
[7] Fitzpatrick RW, Pate RG. Comparing the use of inhalation anaesthetics. Pharmaceutical Journal 2009;283:540–1.
[8] Prescribing information to support LDP — PCT data appendix. Keele: Keele University, 2008.
[9] Dyspepsia: managing dyspepsia in adults in primary care. National Institute for Health and Clinical Excellence Clinical Guideline 17. London: NICE, 2004.
[10] Department of Health. Reference costs 2006/07. London: The Department, 2008.
[11] NHS Institute for Innovation and Improvement. Better Care Better Value Indicators 2008. Coventry: The Institute, 2008.
[12] Jones MI. Greenfield SM, Jowett S, Nayak A, Stevenson FA, Bradley CP. Monitoring prescribing: GPs’ use of Prescription Analysis and Cost (PACT) data. Primary Healthcare Research and Development 2002;3:105–14.


