Introduction
Medicines use review (MUR) was introduced as an advanced service in 2005 and is widely practised in community pharmacies. While many of the MURs carried out have been rated as “very good”, there is a wide variation in quality. This may in part be due to a lack of minimum standards for MUR content and delivery. The Department of Health has expressed concerns over the quality of MURs and has accused pharmacists of conducting them only to get the associated payment.[1]
A number of groups have introduced various initiatives in an attempt to remedy the issue of variable MUR quality. One pharmacist was able to demonstrate the quality of his MURs by monitoring recommendations made on MUR action plans. He was able to show that his interventions improved the standard of patient care, with respect to improving compliance; stopping, optimising and switching medicines; adding a medicine and optimising quantities prescribed.[2]
Both the Devon and Hampshire and the Isle of Wight local pharmaceutical committees attempted to improve MUR quality by providing pharmacists with a resource pack of “crib sheets” to be used during MURs. Each A4 crib sheet comprised triggers for MURs, concordance hints, signposting hints and advice on conducting MURs.[3]
These checklists contain information similar to that present in the quality and outcomes framework (QOF) system used by GPs.
The QOF system was introduced as a voluntary incentive programme for GPs in 2004 with the aim of being able to reward GPs for patient care. It uses a set of evidence- based indicators to demonstrate effective care provision. There are four domains, each of which consists of a set of indicators, against which GP surgeries score points according to their level of achievement. The four domains are:
- Clinical care indicators for 19 clinical areas (such as hypertension)
- Organisational indicators in the areas of records; information for patients; education and training; practice management and medicines management
- Patient experience indicators relating to patient surveys and length of consultations
- Additional services indicators in service areas like child health surveillance, maternity services.[4]
A quality and outcomes framework has been developed for use in community pharmacies in the Doncaster primary care trust area. The aim was to encourage contractors to implement processes, practices and systems beyond the basic contractual requirements.
The quality and outcomes framework consisted of 25 indicators, each assigned a points value. Activities such as the reporting of significant events and undertaking internal audits were assigned more points than, for example, the number of MURs completed legibly and in full.[5]
The aim of this study was to evaluate pharmacists’ opinions on the use of a QOF as a tool to improve the standard of MURs using an asthma checklist as an example of a possible proposed quality and outcomes framework.
Method
Postal questionnaires were sent in January 2010 to all 202 pharmacies in the Derby City and Derbyshire County primary care trust regions.
Pharmacists were asked to return completed anonymous questionnaires in prepaid envelopes.
The questionnaire was designed to collect pharmacists’ views on the following:
- Why they thought the DoH had called for an improvement in MUR quality
- The potential effects of quality and outcomes framework implementation on the following: MUR quality, patient disease management, patient satisfaction, remuneration and pharmacist training requirements
- Which indicators should be used to assess the quality of MURs, such as clinical (pharmacist demonstrating up-to-date practice), organisational (MUR form documentation) and patient experience, as evaluated by satisfaction surveys?
Demographic data were collected, including the number of years registered as a pharmacist, type of pharmacy (whether a large chain, independent or other) and length of time accredited to conduct MURs. Respondents were given the opportunity to write comments about the concept of QOF development for MURs.
It was thought that being able to envisage what a QOF might look like would help pharmacists to complete questionnaires effectively. Therefore, an example of an asthma QOF was developed (Panel 1). This QOF was an evidence-based checklist that could be used as a structured guide to completing an MUR on patients with asthma.
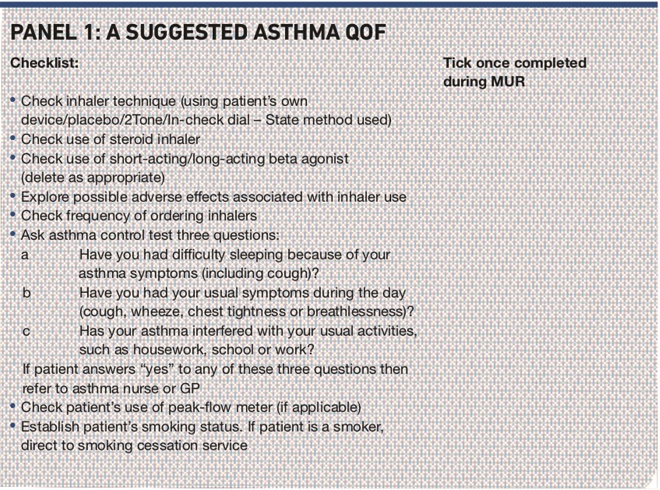
Panel 1. Asuggested asthma QOF
Results
A response rate of 40 per cent (80 out of 202 questionnaires) was generated from the postal pharmacy questionnaire. Table 1 shows the pharmacist demographic data obtained.
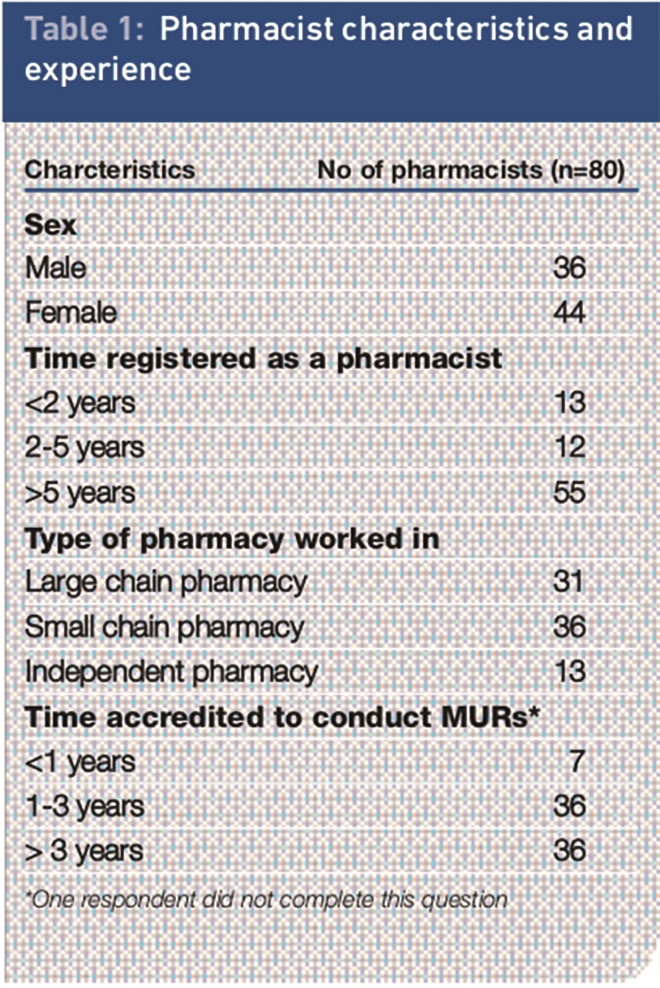
Table 1. Pharmacist characteristics and experience
When pharmacists were asked why they thought that the DoH had requested an improvement in MUR quality, 69 per cent of responses indicated that this was either because unnecessary MURs were being conducted to meet company targets or for monetary gain. Table 2 shows a breakdown of the responses to this question. Pharmacists could choose more than one response.
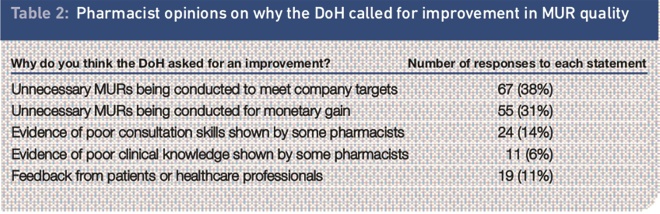
Table 2. Pharmacist opinions on why the DoH called for improvement in MUR quality
A number of statements were made to the pharmacists. Of 80 respondents, 52 (65 per cent) agreed that implementing a quality and outcomes framework for MURs would be a positive step towards improving MUR quality. Forty-six pharmacists (58 per cent) agreed that quality and outcomes framework implementation for MURs would be a positive step towards improving patient disease management.
Interestingly, however, only 36 per cent of pharmacists agreed that a QOF for MURs would be a positive step towards improving patient satisfaction with MURs. Table 3 outlines pharmacists’ opinions on the possible outcomes of QOF implementation.
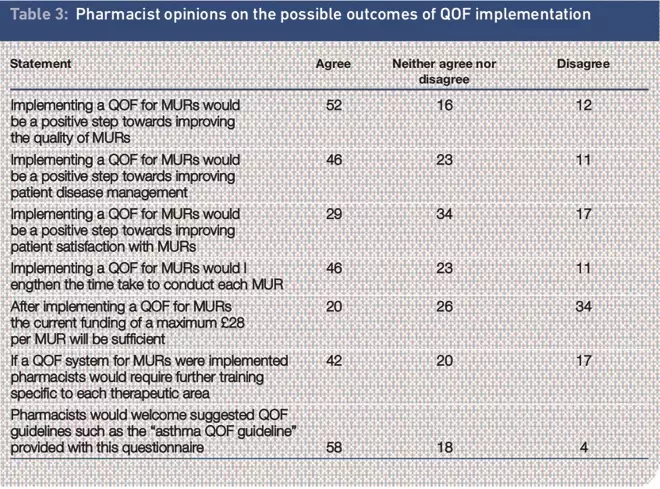
Table 3. Pharmacist opinions on the possible outcomes of QOF implementation
The final question was “If a QOF for MURs were introduced, are the following domains appropriate for assessing the quality of MURs? Pharmacists were required to answer “yes” or “no” to each of the following:
- Clinical (eg, demonstrating up-to-date practice)
- Organisational (MUR form documentation, accurate patient information and patient education)
- Patient experience (eg, patient satisfaction surveys)
At the end of this question, there was an opportunity for free-text comments to be made.
Out of 80 respondents, 56 believed that a clinical domain was appropriate; 62 thought an organisational domain was appropriate and 47 thought that patient experience was appropriate.
Although the organisational domain was believed by most pharmacists to be the most appropriate way of assessing MUR quality, some comments were made to the contrary.
Concerns were expressed over the increased workload and time that would be needed to conduct an MUR based on a QOF, with no overall perceived increase in quality. One respondent said: “A quality and outcomes framework is just another admin tool, which I don’t need.” Another said: “The MUR paperwork is already quite a burden, although improved recently.” A third said: “A quality and outcomes framework will increase paperwork, not quality.”
Discussion
The quality and effectiveness of MURs is likely to show wide variations across geographical areas. The national MUR audit launched by the Royal Pharmaceutical Society is aimed at providing feedback on the quality and effectiveness of MURs. Four key groups — community pharmacists, GPs, primary care organisations and patients who have experience of MURs — are being asked to provide feedback on the MUR service.
Early results show that 93 per cent of patients are likely to follow advice about their medicines given to them during an MUR and 84 per cent believed their knowledge about medicines improved as a result.[6]
Seventy- three per cent (58/80) of pharmacists in this study would welcome the introduction of QOF guidelines, such as the example provided here for asthma. This may be because many pharmacists in this survey think the addition of a QOF to structure MURs, would improve MUR quality and patient disease management.
Disease-specific targeted MURs have been shown to provide real benefit to patients and a measure of MUR quality. The community pharmacy asthma MUR project in Hampshire and the Isle of Wight was able to illustrate the important role community pharmacist can play in the management of asthma patients through delivery of targeted MURs.[7]
One limitation of our survey is the response rate to the questionnaire of 40 per cent. However, it is clear that the pharmacists surveyed would welcome the concept of a QOF and although there is a perception of it increasing the time taken to conduct an MUR it may also improve the quality. One pharmacist commented: “I feel a quality and outcomes framework would standardise the quality of MURs across community pharmacy. Currently there is a large variation between the quality of MURs conducted by different pharmacists.”
Concerns were expressed over patients with multiple disease states hence requiring a QOF per condition. One pharmacist thought that “it would be nice if a national electronic MUR tool was developed by the Pharmaceutical Services Negotiating Committee and DoH that was available to pharmacy contractors to generate and manage the MUR paperwork. Such a tool could incorporate the individual disease QOFs to help the MUR process.” Over half of the pharmacists in our survey agreed that if QOFs were implemented, further training would be needed to deal with specific therapeutic areas. There are increasing pressures on healthcare providers to provide quality and cost-effective services for patients. As a profession, pharmacists will be required to demonstrate quality outcomes in the services they provide. The use of quality and outcomes frameworks could be an integral part of this process, although not all contractors may welcome this approach.
Conclusion
It is vital not to lose sight of the original intention of the introduction of MURs, which was to help patients make better use of their medicines. As the number of pharmacists accredited to do MURs and the number of MURs performed continues to increase, the profession has a collective responsibility to ensure that the quality of MURs is maintained. The introduction of an accredited system may be one element of a quality assurance process that helps to ensure the standard of MURs is appropriate to achieving excellent patient outcomes in the use of medicines.
About the authors
Susan Youssef MRPharmS, is senior lecturer in pharmacy practice and community pharmacist
Kishan Karia was a fourth-year pharmacy student
Sandra Hall MRPharmS, is head of pharmacy practice
All at De Montfort University, Leicester.
Correspondence to: Susan Youssef, Senior Lecturer in Pharmacy Practice, Leicester School of Pharmacy, De Montfort University, The Gateway, Leicester LE1 9BH (email: syoussef@dmu.ac.uk)
References
[1] Rose C. DoH says quality of MURs must improve. Pharmaceutical Journal 2009;282:759.
[2] Choudhury A. Do we know how many of our MUR recommendations are followed? Pharmaceutical Journal 2009; 282:715.
[3] Connelly D. MURs: increasing quality and quantity. Pharmaceutical Journal 2007; 278:213.
[4] NHS. Quality and Outcomes Framework. Available at: www.qof.ic.nhs.uk
[5] Connelly D. Aim for quality and reap the rewards. Pharmaceutical Journal 2009;283:477.
[6] Over 90 per cent of patients follow MUR advice, national audit finds. Pharmaceutical Journal 2010;284:178.
[7] Portlock J. Holden M, Patel S. A community pharmacy asthma MUR project in Hampshire and Isle of Wight. Pharmaceutical Journal 2009;282:109–12.
You may also be interested in
The importance of diverse clinical imagery within health education

Government should consider ways to prevent ‘inappropriate overseas prescribing’ of hormone drugs, review recommends
